Abstract
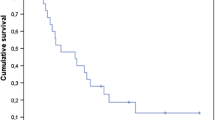
The characteristics of brain metastases (BM) that develop after breast-conserving therapy (BCT) for early-stage breast cancer (BC) remain incompletely defined. We examined 1,434 consecutive patients with stage I/II invasive BC who received BCT from 1997 to 2006, 91 % of whom received adjuvant systemic therapy, according to BC subtype. Median follow-up was 85 months. Overall 5-year cumulative incidence of BM was 1.7 %; 0.1 % for luminal A, 3.3 % for luminal B, 3.2 % for luminal-HER2, 3.7 % for HER2, and 7.4 % for triple negative (TN). Women who developed BM were more likely at BC diagnosis to be younger (P < .0001) and have node-positive (P < .0001), grade 3 (P < .0001), hormone receptor-negative (P = .006), and HER2-positive (P = .01) tumors. Median time from BC diagnosis to BM was 51.4 months (range, 7.6–108 months), which was longer among luminal versus non-luminal subtypes (P = .0002; median, 61.4 vs. 34.5 months). Thirty-four percent of patients who developed distant metastases (DM) eventually developed BM. Median time from DM to BM was 12.8 months but varied by subtype, including 7.4 months for TN, 9.6 months for luminal B, and 27.1 months for HER2. Eighty-one percent of all BM patients presented with neurologic symptoms. Median number of BM at diagnosis was two, and median BM size was 15 mm, with TN (27 mm) and luminal B (16 mm) exhibiting the largest median sizes. In conclusion, the risk of BM after BCT varies significantly by subtype. Given the large size and symptomatic presentation among luminal B and TN subtypes, earlier BM detection might improve quality of life or increase eligibility for non-invasive treatments including stereotactic radiosurgery. Women with DM from these two BC subtypes have a high incidence of BM with a short latency, suggesting an ideal target population for trials evaluating the utility of MRI screening.


Similar content being viewed by others
References
Anderson SJ, Wapnir I, Dignam JJ et al (2009) Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in patients treated by breast-conserving therapy in five National Surgical Adjuvant Breast and Bowel Project protocols of node-negative breast cancer. J Clin Oncol 27:2466–2473
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trials. Lancet 365:1687–1717
Lin NU, Bellon JR, Winer EP (2004) CNS metastases in breast cancer. J Clin Oncol 22:3608–3617
Crivellari D, Pagani O, Veronesi A et al (2001) High incidence of central nervous system involvement in patients with metastatic or locally advanced breast cancer treated with epirubicin and docetaxel. Ann Oncol 12:353–356
Burstein GJ, Lieberman G, Slamon DJ, Winer EP, Klein P (2005) Isolated central nervous system metastases in patients with HER2-overexpressing advanced breast cancer treated with first-line trastuzumab-based therapy. Ann Oncol 16:1772–1777
Barnholtz-Sloan JS, Sloan AE, Davis FG et al (2004) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 22:2865–2872
Nam BH, Kim SY, Han HS et al (2008) Breast cancer subtypes and survival in patients with brain metastases. Breast Cancer Res 10:R20
Niwinska A, Murawska M, Pogoda K (2010) Breast cancer brain metastases: differences in survival depending on biological subtype, RPA RTOG prognostic class and systemic treatment after whole-brain radiotherapy (WBRT). Ann Oncol 21:942–948
Lin NU, Claus E, Sohl J et al (2008) Sites of distant recurrence and clinical outcomes in patients with metastatic triple-negative breast cancer: high incidence of central nervous system metastases. Cancer 113:2638–2645
Kennecke H, Yerushalmi R, Woods R et al (2010) Metastatic behavior of breast cancer subtypes. J Clin Oncol 28:3271–3277
Harrell JC, Prat A, Parker JS et al (2012) Genomic analysis identifies unique signatures predictive of brain, lung, and liver relapse. Breast Cancer Res Treat 132:523–535
Cheang MC, Chia SK, Voduc D et al (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101:736–750
Arvold ND, Taghian AG, Niemierko A et al (2011) Age, breast cancer subtype approximation, and local recurrence after breast-conserving therapy. J Clin Oncol 29:3885–3891
Gray RJ (1988) A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16:1141–1154
Lin NU, Vanderplas A, Hughes ME et al (2012) Clinicopathologic features, patterns of recurrence, and survival among women with triple-negative breast cancer in the National Comprehensive Cancer Network. Cancer. doi:10.1002/cncr.27581
Leyland-Jones B (2009) Human epidermal growth factor receptor 2-positive breast cancer and central nervous system metastases. J Clin Oncol 27:5278–5286
Niwinska A, Tacikowska M, Murawska M (2010) The effect of early detection of occult brain metastases in HER2-positive breast cancer patients on survival and cause of death. Int J Radiat Oncol Biol Phys 77:1134–1139
Miller KD, Weathers T, Haney LG et al (2003) Occult central nervous system involvement in patients with metastatic beeast cancer: prevalence, predictive factors and impact on overall survival. Ann Oncol 14:1072–1077
Borgelt B, Gelber R, Kramer S et al (1980) The palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 6:1–9
Tsao M, Zu W, Sahgal A (2012) A meta-analysis evaluating stereotactic radiosurgery, whole-brain radiotherapy, or both for patients presenting with a limited number of brain metastases. Cancer 118:2486–2493
Sperduto PW, Kased N, Roberge D et al (2012) Effect of tumor subtype on survival and the graded prognostic assessment for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys 82:2111–2117
Acknowledgments
Conflict of Interest
The authors declare that they have no conflicts of interest. Dr. Lin reports receiving research funding from GlaxoSmithKline, Genentech, and Geron.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arvold, N.D., Oh, K.S., Niemierko, A. et al. Brain metastases after breast-conserving therapy and systemic therapy: incidence and characteristics by biologic subtype. Breast Cancer Res Treat 136, 153–160 (2012). https://doi.org/10.1007/s10549-012-2243-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2243-x