Abstract
Objectives
Our aim was to assess whether magnetic resonance imaging (MRI) features predict recurrence-free survival (RFS) after prostate cancer high-intensity focused ultrasound (HIFU) ablation.
Methods
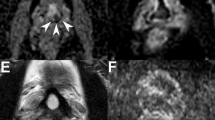
We retrospectively selected 81 patients who underwent (i) whole-gland HIFU ablation between 2007 and 2011 as first-line therapy or salvage treatment after radiotherapy or brachytherapy, and (ii) pre- and postoperative MRI. On preoperative imaging, two senior (R1, R2) and one junior (R3) readers assessed the number of sectors invaded by the lesion with the highest Likert score (dominant lesion) using a 27-sector diagram. On postoperative imaging, readers assessed destruction of the dominant lesion using a three-level score. Multivariate analysis included the number of sectors invaded by the dominant lesion, its Likert and destruction scores, the pre-HIFU prostate-specific antigen (PSA) level, Gleason score, and the clinical setting (primary/salvage).
Results
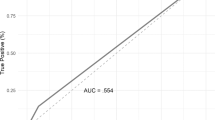
The most significant predictor was the number of prostate sectors invaded by the dominant lesion for R2 and R3 (p≤0.001) and the destruction score of the dominant lesion for R1 (p = 0.011). The pre-HIFU PSA level was an independent predictor for R2 (p = 0.014), but with only marginal significance for R1 (p = 0.059) and R3 (p = 0.053).
Conclusion
The dominant lesion’s size and destruction assessed by MRI provide independent prognostic information compared with usual predictors.
Key Points
• The size of the MR-dominant lesion significantly influences post-HIFU recurrence-free survival.
• The destruction score of the MR-dominant lesion predicts post-HIFU recurrence-free survival.
• Patients with a completely devascularized MR-dominant lesion show better recurrence-free survival
• Pre- and post-HIFU MRI provide prognostic information independent of usual predictors.





Similar content being viewed by others
Abbreviations
- HIFU:
-
High-intensity focused ultrasound
- MR:
-
Magnetic resonance
- TSE:
-
turbo spin echo
- T2w:
-
T2-weighted
- DCE:
-
dynamic contrast-enhanced
- IQR:
-
Interquartile range
- RFS:
-
recurrence-free survival
- ADC:
-
apparent coefficient diffusion
References
Chapelon JY, Rouviere O, Crouzet S, Gelet A (2016) Prostate Focused Ultrasound Therapy. Adv Exp Med Biol 880:21–41
Crouzet S, Chapelon JY, Rouviere O et al (2014) Whole-gland ablation of localized prostate cancer with high-intensity focused ultrasound: oncologic outcomes and morbidity in 1002 patients. Eur Urol 65(5):907–914
Crouzet S, Murat FJ, Pommier P et al (2012) Locally recurrent prostate cancer after initial radiation therapy: early salvage high-intensity focused ultrasound improves oncologic outcomes. Radiother Oncol 105(2):198–202
Ahmed HU, Cathcart P, McCartan N et al (2012) Focal salvage therapy for localized prostate cancer recurrence after external beam radiotherapy: a pilot study. Cancer 118(17):4148–4155
Ahmed HU, Freeman A, Kirkham A et al (2011) Focal therapy for localized prostate cancer: a phase I/II trial. J Urol 185(4):1246–1254
Ganzer R, Fritsche HM, Brandtner A et al (2013) Fourteen-year oncological and functional outcomes of high-intensity focused ultrasound in localized prostate cancer. BJU Int 112(3):322–329
Bratan F, Niaf E, Melodelima C et al (2013) Influence of imaging and histological factors on prostate cancer detection and localisation on multiparametric MRI: a prospective study. Eur Radiol 23(7):2019–2029
Turkbey B, Pinto PA, Mani H et al (2010) Prostate cancer: value of multiparametric MR imaging at 3 T for detection--histopathologic correlation. Radiology 255(1):89–99
Rouviere O, Vitry T, Lyonnet D (2010) Imaging of prostate cancer local recurrences: why and how? Eur Radiol 20(5):1254–1266
Donati OF, Jung SI, Vargas HA et al (2013) Multiparametric prostate MR imaging with T2-weighted, diffusion-weighted, and dynamic contrast-enhanced sequences: are all pulse sequences necessary to detect locally recurrent prostate cancer after radiation therapy? Radiology 268(2):440–450
Abd-Alazeez M, Ramachandran N, Dikaios N et al (2015) Multiparametric MRI for detection of radiorecurrent prostate cancer: added value of apparent diffusion coefficient maps and dynamic contrast-enhanced images. Prostate Cancer Prostatic Dis 18(2):128–136
Alonzo F, Melodelima C, Bratan F et al (2016) Detection of locally radio-recurrent prostate cancer at multiparametric MRI: Can dynamic contrast-enhanced imaging be omitted? Diagn Interv Imaging 97(4):433–441
Mozer P, Roupret M, Le Cossec C et al (2015) First round of targeted biopsies using magnetic resonance imaging/ultrasonography fusion compared with conventional transrectal ultrasonography-guided biopsies for the diagnosis of localised prostate cancer. BJU Int 115(1):50–57
Costa DN, Lotan Y, Rofsky NM et al (2016) Assessment of Prospectively Assigned Likert Scores for Targeted Magnetic Resonance Imaging-Transrectal Ultrasound Fusion Biopsies in Patients with Suspected Prostate Cancer. J Urol 195(1):80–87
Rouviere O, Lyonnet D, Raudrant A et al (2001) MRI appearance of prostate following transrectal HIFU ablation of localized cancer. Eur Urol 40(3):265–274
Kirkham AP, Emberton M, Hoh IM, Illing RO, Freeman AA, Allen C (2008) MR imaging of prostate after treatment with high-intensity focused ultrasound. Radiology 246(3):833–844
Fry FJ (1993) Intense focused ultrasound in medicine. Some practical guiding physical principles from sound source to focal site in tissue. Eur Urol 23(Suppl 1):2–7
Boni RA, Sulser T, Jochum W, Romanowski B, Debatin JF, Krestin GP (1997) Laser ablation-induced changes in the prostate: findings at endorectal MR imaging with histologic correlation. Radiology 202(1):232–236
Beerlage HP, van Leenders GJ, Oosterhof GO et al (1999) High-intensity focused ultrasound (HIFU) followed after one to two weeks by radical retropubic prostatectomy: results of a prospective study. Prostate 39(1):41–46
Fite BZ, Wong A, Liu Y et al (2015) Magnetic resonance imaging assessment of effective ablated volume following high intensity focused ultrasound. PLoS ONE 10(3), e0120037
Rouviere O, Girouin N, Glas L et al (2010) Prostate cancer transrectal HIFU ablation: detection of local recurrences using T2-weighted and dynamic contrast-enhanced MRI. Eur Radiol 20(1):48–55
Oto A, Kayhan A, Jiang Y et al (2010) Prostate cancer: differentiation of central gland cancer from benign prostatic hyperplasia by using diffusion-weighted and dynamic contrast-enhanced MR imaging. Radiology 257(3):715–723
Hoeks CM, Hambrock T, Yakar D et al (2013) Transition Zone Prostate Cancer: Detection and Localization with 3-T Multiparametric MR Imaging. Radiology 266(1):207–217
Chesnais AL, Niaf E, Bratan F et al (2013) Differentiation of transitional zone prostate cancer from benign hyperplasia nodules: evaluation of discriminant criteria at multiparametric MRI. Clin Radiol 68(6):e323–e330
Barentsz JO, Richenberg J, Clements R et al (2012) ESUR prostate MR guidelines 2012. Eur Radiol 22(4):746–757
Vache T, Bratan F, Mege-Lechevallier F, Roche S, Rabilloud M, Rouviere O (2014) Characterization of prostate lesions as benign or malignant at multiparametric MR imaging: comparison of three scoring systems in patients treated with radical prostatectomy. Radiology 272(2):446–455
Uchida T, Shoji S, Nakano M et al (2009) Transrectal high-intensity focused ultrasound for the treatment of localized prostate cancer: eight-year experience. Int J Urol 16(11):881–886
Rouviere O, Sbihi L, Gelet A, Chapelon JY (2013) Salvage high-intensity focused ultrasound ablation for prostate cancer local recurrence after external-beam radiation therapy: prognostic value of prostate MRI. Clin Radiol 68(7):661–667
Cho S, Kang SH (2014) Current status of cryotherapy for prostate and kidney cancer. Korean J Urol 55(12):780–788
Livraghi T, Goldberg SN, Lazzaroni S et al (2000) Hepatocellular carcinoma: radio-frequency ablation of medium and large lesions. Radiology 214(3):761–768
Gervais DA, McGovern FJ, Arellano RS, McDougal WS, Mueller PR (2005) Radiofrequency ablation of renal cell carcinoma: part 1, Indications, results, and role in patient management over a 6-year period and ablation of 100 tumors. AJR Am J Roentgenol 185(1):64–71
Salomon L, Colombel M, Patard JJ et al (1999) Value of ultrasound-guided systematic sextant biopsies in prostate tumor mapping. Eur Urol 35(4):289–293
Murat FJ, Poissonnier L, Rabilloud M et al (2009) Mid-term results demonstrate salvage high-intensity focused ultrasound (HIFU) as an effective and acceptably morbid salvage treatment option for locally radiorecurrent prostate cancer. Eur Urol 55(3):640–647
Anzai Y, Lufkin RB, Hirschowitz S, Farahani K, Castro DJ (1992) MR imaging-histopathologic correlation of thermal injuries induced with interstitial Nd:YAG laser irradiation in the chronic model. J Magn Reson Imaging 2(6):671–678
Barentsz JO, Weinreb JC, Verma S et al (2016) Synopsis of the PI-RADS v2 Guidelines for Multiparametric Prostate Magnetic Resonance Imaging and Recommendations for Use. Eur Urol 69(1):41–49
Rouviere O, Papillard M, Girouin N et al (2012) Is it possible to model the risk of malignancy of focal abnormalities found at prostate multiparametric MRI? Eur Radiol 22(5):1149–1157
Ahmed HU, Dickinson L, Charman S et al (2015) Focal Ablation Targeted to the Index Lesion in Multifocal Localised Prostate Cancer: a Prospective Development Study. Eur Urol 68(6):927–936
Haffner MC, Mosbruger T, Esopi DM et al (2013) Tracking the clonal origin of lethal prostate cancer. J Clin Invest 123(11):4918–4922
Zelefsky MJ, Reuter VE, Fuks Z, Scardino P, Shippy A (2008) Influence of local tumor control on distant metastases and cancer related mortality after external beam radiotherapy for prostate cancer. J Urol 179(4):1368–1373, discussion 1373
Acknowledgments
The scientific guarantor of this publication is Olivier Rouvière. The authors of this manuscript declare relationships with the following companies: Olivier Rouvière, Sébastien Crouzet and Albert Gelet are consultants for EDAP-TMS and participated to clinical studies funded by EDAP-TMS. The authors state that this work has not received any funding. Jean-Pierre Giraud (EDAP-TMS) kindly provided statistical advice for this manuscript.
Institutional Review Board approval was not required because this is a retrospective study. In France retrospective studies do not need approval by Institutional Review Board. Written informed consent was obtained from all subjects (patients) in this study. Written informed consent was not required for this study because this is not required in France for retrospective studies; please note that, since Institutional Review Board do not assess retrospective studies in France, they do not deliver waivers for informed consent as in other countries.
Some study subjects or cohorts have been previously reported in studies reporting the global outcome of HIFU ablations:
• Crouzet S, Chapelon JY, Rouvière O, Mege-Lechevallier F, Colombel M, Tonoli-Catez H, Martin X, Gelet A. Whole-gland Ablation of Localized Prostate Cancer with High-intensity Focused Ultrasound: Oncologic Outcomes and Morbidity in 1002 Patients. Eur Urol. 2013 Apr 30
• Crouzet S, Murat FJ, Pommier P, Poissonnier L, Pasticier G, Rouviere O, Chapelon JY, Rabilloud M, Belot A, Mège-Lechevallier F, Tonoli-Catez H, Martin X, Gelet A. Locally recurrent prostate cancer after initial radiation therapy: Early salvage high-intensity focused ultrasound improves oncologic outcomes. Radiother Oncol. 2012 Nov;105(2):198-202
• Crouzet S, Rebillard X, Chevallier D, Rischmann P, Pasticier G, Garcia G, Rouviere O, Chapelon JY, Gelet A. Multicentric oncologic outcomes of high-intensity focused ultrasound for localized prostate cancer in 803 patients. Eur Urol. 2010; 58:559-66
• Murat FJ, Poissonnier L, Rabilloud M, Belot A, Bouvier R, Rouviere O, Chapelon JY, Gelet A. Mid-term Results Demonstrate Salvage High-Intensity Focused Ultrasound (HIFU) as an Effective and Acceptably Morbid Salvage Treatment Option for Locally Radiorecurrent Prostate Cancer. Eur Urol. 2009, 55:640-647
Methodology: retrospective, prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosset, R., Bratan, F., Crouzet, S. et al. Can pre- and postoperative magnetic resonance imaging predict recurrence-free survival after whole-gland high-intensity focused ablation for prostate cancer?. Eur Radiol 27, 1768–1775 (2017). https://doi.org/10.1007/s00330-016-4491-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4491-3