Abstract
Objectives
To compare 3D-inversion-recovery balanced steady-state free precession (IR-bSSFP) non-contrast-enhanced magnetic resonance angiography (MRA) with 3D-contrast-enhanced MRA (CE-MRA) for assessment of renal artery stenosis (RAS) using digital subtraction angiography (DSA) as the reference standard.
Methods
Bilateral RAS were surgically created in 12 swine. IR-bSSFP and CE-MRA were acquired at 1.5 T and compared to rotational DSA. Three experienced cardiovascular radiologists evaluated the IR-bSSFP and CE-MRA studies independently. Linear regression models were used to calibrate and assess the accuracy of IR-bSSFP and CE-MRA, separately, against DSA. The coefficient of determination and Cohen's kappa coefficient were also generated.
Results
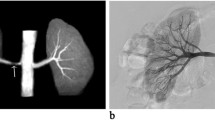
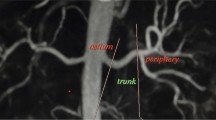
Calibration of the three readers’ RAS grading revealed R2 values of 0.52, 0.37 and 0.59 for NCE-MRA and 0.48, 0.53 and 0.71 for CE-MRA. Inter-rater agreement demonstrated Cohen’s kappa values ranging from 0.25 to 0.65. Distal renal artery branch vessels were visible to a significantly higher degree with NCE-MRA compared to CE-MRA (p < 0.001). Image quality was rated excellent for both sequences, although image noise was higher with CE-MRA (p < 0.05). In no cases did noise interfere with image interpretation.
Conclusions
In a well-controlled animal model of surgically induced RAS, IR-bSSFP based NCE-MRA and CE-MRA accurately graded RAS with a tendency for stenosis overestimation, compared to DSA.
Key Points
• IR-bSSFP and CE-MRA are accurate methods for diagnosis of renal artery stenosis
• IR-bSSFP and CE-MRA demonstrate excellent agreement with DSA
• Both IR-bSSFP and CE-MRA have a tendency to overestimate renal artery stenosis






Similar content being viewed by others
Abbreviations
- bSSFP:
-
Balanced steady-state free precession
- CE-MRA:
-
Contrast-enhanced magnetic resonance angiography
- CTA:
-
Contrast-enhanced computed tomography angiography
- DSA:
-
Digital subtraction angiography
- FMD:
-
Fibromuscular dysplasia
- GBCA:
-
Gadolinium-based contrast agent
- IACUC:
-
Institutional Animal Care and Use Committee
- IR-bSSFP:
-
Inversion-recovery bSSFP
- NCE-MRA:
-
Non-contrast-enhanced magnetic resonance angiography
- PC:
-
Phase contrast
- RAS:
-
Renal artery stenosis
- SAH:
-
Systemic arterial hypertension
- SNR:
-
Signal-to-noise ratio
- TOF:
-
Time of flight
References
Hajjar I, Kotchen JM, Kotchen TA (2006) Hypertension: trends in prevalence, incidence, and control. Annu Rev Public Health 27:465–490
Safian RD, Textor SC (2001) Renal-artery stenosis. NEJM 344:431–442
Cooper CJ, Murphy TP, Cutlip DE et al (2014) Stenting and medical therapy for atherosclerotic renal-artery stenosis. NEJM 370:13–22
Investigators A, Wheatley K, Ives N et al (2009) Revascularization versus medical therapy for renal-artery stenosis. NEJM 361:1953–1962
Bakris GL, Townsend RR, Liu M et al (2014) Impact of renal denervation on 24-hour ambulatory blood pressure: results from SYMPLICITY HTN-3. J Am Coll Cardiol 64:1071–1078
Esler MD, Bohm M, Sievert H et al (2014) Catheter-based renal denervation for treatment of patients with treatment-resistant hypertension: 36 month results from the SYMPLICITY HTN-2 randomized clinical trial. Eur Heart J 35:1752–1759
De Cobelli F, Venturini M, Vanzulli A et al (2000) Renal arterial stenosis: prospective comparison of color Doppler US and breath-hold, three-dimensional, dynamic, gadolinium-enhanced MR angiography. Radiology 214:373–380
Fain SB, King BF, Breen JF, Kruger DG, Riederer SJ (2001) High-spatial-resolution contrast-enhanced MR angiography of the renal arteries: a prospective comparison with digital subtraction angiography. Radiology 218:481–490
Hany TF, Debatin JF, Leung DA, Pfammatter T (1997) Evaluation of the aortoiliac and renal arteries: comparison of breath-hold, contrast-enhanced, three-dimensional MR angiography with conventional catheter angiography. Radiology 204:357–362
Daftari Besheli L, Aran S, Shaqdan K, Kay J, Abujudeh H (2014) Current status of nephrogenic systemic fibrosis. Clin Radiol 69:661–668
Miyazaki M, Lee VS (2008) Nonenhanced MR angiography. Radiology 248:20–43
Herborn CU, Watkins DM, Runge VM, Gendron JM, Montgomery ML, Naul LG (2006) Renal arteries: comparison of steady-state free precession MR angiography and contrast-enhanced MR angiography. Radiology 239:263–268
Khoo MM, Deeab D, Gedroyc WM, Duncan N, Taube D, Dick EA (2011) Renal artery stenosis: comparative assessment by unenhanced renal artery MRA versus contrast-enhanced MRA. Eur Radiol 21:1470–1476
Lanzman RS, Voiculescu A, Walther C et al (2009) ECG-gated nonenhanced 3D steady-state free precession MR angiography in assessment of transplant renal arteries: comparison with DSA. Radiology 252:914–921
Maki JH, Wilson GJ, Eubank WB, Glickerman DJ, Millan JA, Hoogeveen RM (2007) Navigator-gated MR angiography of the renal arteries: a potential screening tool for renal artery stenosis. AJR Am J Roentgenol 188:W540–W546
Wyttenbach R, Braghetti A, Wyss M et al (2007) Renal artery assessment with nonenhanced steady-state free precession versus contrast-enhanced MR angiography. Radiology 245:186–195
Francois CJ, Lum DP, Johnson KM et al (2011) Renal arteries: isotropic, high-spatial-resolution, unenhanced MR angiography with three-dimensional radial phase contrast. Radiology 258:254–260
Angeretti MG, Lumia D, Cani A et al (2013) Non-enhanced MR angiography of renal arteries: comparison with contrast-enhanced MR angiography. Acta Radiol 54:749–756
Glockner JF, Takahashi N, Kawashima A et al (2010) Non-contrast renal artery MRA using an inflow inversion recovery steady state free precession technique (Inhance): comparison with 3D contrast-enhanced MRA. J Magn Reson Imaging 31:1411–1418
Goetti R, Baumueller S, Alkadhi H et al (2013) Diagnostic performance of a non-contrast-enhanced magnetic resonance imaging protocol for potential living related kidney donors. Acad Radiol 20:393–400
Laurence I, Ariff B, Quest RA et al (2012) Is there a role for free breathing non-contrast steady-state free precession renal MRA imaging for assessing live donors? A preliminary study. Br J Radiol 85:e448–e454
Liu X, Berg N, Sheehan J et al (2009) Renal transplant: nonenhanced renal MR angiography with magnetization-prepared steady-state free precession. Radiology 251:535–542
Miyazaki M, Akahane M (2012) Non-contrast enhanced MR angiography: established techniques. J Magn Reson Imaging 35:1–19
Serai S, Towbin AJ, Podberesky DJ (2012) Non-contrast MRA using an inflow-enhanced, inversion recovery SSFP technique in pediatric abdominal imaging. Pediatr Radiol 42:364–368
Utsunomiya D, Miyazaki M, Nomitsu Y et al (2008) Clinical role of non-contrast magnetic resonance angiography for evaluation of renal artery stenosis. Circ J: Off J Jap Circ Soc 72:1627–1630
Brau AC, Beatty PJ, Skare S, Bammer R (2008) Comparison of reconstruction accuracy and efficiency among autocalibrating data-driven parallel imaging methods. Magn Reson Med 59:382–395
Lum DP, Busse RF, Francois CJ et al (2009) Increased volume of coverage for abdominal contrast-enhanced MR angiography with two-dimensional autocalibrating parallel imaging: initial experience at 3.0 Tesla. J Magn Reson Imaging 30:1093–1100
Carey VJ LT, Ripley BD (2009) gee: Generalized Estimation Equation solver. R package version 4.13–14. http://CRAN.R-project.org/package=gee
R Development Core Team (2009) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0. http://www.R-project.org [R2.10.0]
Maki JH, Wilson GJ, Eubank WB, Glickerman DJ, Pipavath S, Hoogeveen RM (2007) Steady-state free precession MRA of the renal arteries: breath-hold and navigator-gated techniques vs. CE-MRA. J Magn Reson Imaging 26:966–973
Buijs PC, Klop RB, Eikelboom BC et al (1993) Carotid bifurcation imaging: magnetic resonance angiography compared to conventional angiography and Doppler ultrasound. Eur J Vasc Surg 7:245–251
Scarabino T, Carriero A, Magarelli N et al (1998) MR angiography in carotid stenosis: a comparison of three techniques. Eur J Radiol 28:117–125
Acknowledgments
The scientific guarantor of this publication is Scott Reeder. Two of the authors (NT, JB) were employees of GE Healthcare at the time of this study. All other authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The University of Wisconsin receives research support from GE Healthcare and Bracco Diagnostics, although no support was received for this study. This study was funded by the University of Wisconsin Department of Radiology Research and Development fund. One of the authors has significant statistical expertise. Institutional Review Board approval was not required because this study did not involve human subjects. Approval for animal use was obtained from the University of Wisconsin Institutional Animal Care and Use Committee (IACUC). Methodology: prospective, experimental, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bley, T.A., François, C.J., Schiebler, M.L. et al. Non-contrast-enhanced MRA of renal artery stenosis: validation against DSA in a porcine model. Eur Radiol 26, 547–555 (2016). https://doi.org/10.1007/s00330-015-3833-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3833-x