Abstract
Purpose
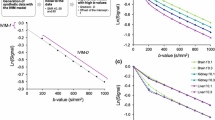
To determine whether a mono-, bi- or tri-exponential model best fits the intravoxel incoherent motion (IVIM) diffusion-weighted imaging (DWI) signal of normal livers.
Materials and methods
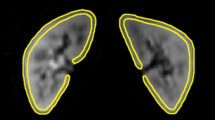
The pilot and validation studies were conducted in 38 and 36 patients with normal livers, respectively. The DWI sequence was performed using single-shot echoplanar imaging with 11 (pilot study) and 16 (validation study) b values. In each study, data from all patients were used to model the IVIM signal of normal liver.
Diffusion coefficients (Di ± standard deviations) and their fractions (fi ± standard deviations) were determined from each model. The models were compared using the extra sum-of-squares test and information criteria.
Results
The tri-exponential model provided a better fit than both the bi- and mono-exponential models. The tri-exponential IVIM model determined three diffusion compartments: a slow (D1 = 1.35 ± 0.03 × 10-3 mm2/s; f1 = 72.7 ± 0.9 %), a fast (D2 = 26.50 ± 2.49 × 10-3 mm2/s; f2 = 13.7 ± 0.6 %) and a very fast (D3 = 404.00 ± 43.7 × 10-3 mm2/s; f3 = 13.5 ± 0.8 %) diffusion compartment [results from the validation study]. The very fast compartment contributed to the IVIM signal only for b values ≤15 s/mm2
Conclusion
The tri-exponential model provided the best fit for IVIM signal decay in the liver over the 0-800 s/mm2 range. In IVIM analysis of normal liver, a third very fast (pseudo)diffusion component might be relevant.
Key Points
• For normal liver, tri-exponential IVIM model might be superior to bi-exponential
• A very fast compartment (D = 404.00 ± 43.7 × 10 -3 mm2 /s; f = 13.5 ± 0.8 %) is determined from the tri-exponential model
• The compartment contributes to the IVIM signal only for b ≤ 15 s/mm 2



Similar content being viewed by others
References
Guiu B, Cercueil JP (2011) Liver diffusion-weighted MR imaging: the tower of Babel? Eur Radiol 21:463–467
Guiu B, Petit JM, Capitan V et al (2012) Intravoxel incoherent motion diffusion-weighted imaging in nonalcoholic fatty liver disease: a 3.0-T MR study. Radiology 265:96–103
Le Bihan D (2008) Intravoxel incoherent motion perfusion MR imaging: a wake-up call. Radiology 249:748–752
Le Bihan D, Breton E, Lallemand D, Aubin ML, Vignaud J, Laval-Jeantet M (1988) Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 168:497–505
Shah B, Anderson SW, Scalera J, Jara H, Soto JA (2011) Quantitative MR imaging: physical principles and sequence design in abdominal imaging. Radiographics 31:867–880
Clark CA, Le Bihan D (2000) Water diffusion compartmentation and anisotropy at high b values in the human brain. Magn Reson Med 44:852–859
Andreou A, Koh DM, Collins DJ et al (2013) Measurement reproducibility of perfusion fraction and pseudodiffusion coefficient derived by intravoxel incoherent motion diffusion-weighted MR imaging in normal liver and metastases. Eur Radiol 23:428–434
Delattre BM, Viallon M, Wei H et al (2012) In vivo cardiac diffusion-weighted magnetic resonance imaging: quantification of normal perfusion and diffusion coefficients with intravoxel incoherent motion imaging. Invest Radiol 47:662–670
Dijkstra H, Baron P, Kappert P, Oudkerk M, Sijens PE (2012) Effects of microperfusion in hepatic diffusion weighted imaging. Eur Radiol 22:891–899
Dyvorne HA, Galea N, Nevers T et al (2013) Diffusion-weighted imaging of the liver with multiple b values: effect of diffusion gradient polarity and breathing acquisition on image quality and intravoxel incoherent motion parameters–a pilot study. Radiology 266:920–929
Hayashi T, Miyati T, Takahashi J et al (2013) Diffusion analysis with triexponential function in liver cirrhosis. J Magn Reson Imaging 38:148–153
Lemke A, Stieltjes B, Schad LR, Laun FB (2011) Toward an optimal distribution of b values for intravoxel incoherent motion imaging. Magn Reson Imaging 29:766–776
Luciani A, Vignaud A, Cavet M et al (2008) Liver cirrhosis: intravoxel incoherent motion MR imaging–pilot study. Radiology 249:891–899
Pasquinelli F, Belli G, Mazzoni LN, Grazioli L, Colagrande S (2011) Magnetic resonance diffusion-weighted imaging: quantitative evaluation of age-related changes in healthy liver parenchyma. Magn Reson Imaging 29:805–812
Patel J, Sigmund EE, Rusinek H, Oei M, Babb JS, Taouli B (2010) Diagnosis of cirrhosis with intravoxel incoherent motion diffusion MRI and dynamic contrast-enhanced MRI alone and in combination: Preliminary experience. J Magn Reson Imaging 31:589–600
Ohtani O, Ohtani Y (2008) Lymph circulation in the liver. Anat Rec (Hoboken) 291:643–652
Moteki T, Horikoshi H (2011) Evaluation of noncirrhotic hepatic parenchyma with and without significant portal vein stenosis using diffusion-weighted echo-planar MR on the basis of multiple-perfusion-components theory. Magn Reson Imaging 29:64–73
Chandarana H, Taouli B (2010) Diffusion and perfusion imaging of the liver. Eur J Radiol 76:348–358
Lemke A, Laun FB, Simon D, Stieltjes B, Schad LR (2010) An in vivo verification of the intravoxel incoherent motion effect in diffusion-weighted imaging of the abdomen. Magn Reson Med 64:1580–1585
Guiu B, Loffroy R, Cercueil JP, Krause D (2008) Multiecho MR imaging andproton MR spectroscopy for liver fat quantification. Radiology 249:1081
Guiu B, Loffroy R, Petit JM et al (2009) Mapping of liver fat with triple-echo gradient echo imaging: validation against 3.0-T proton MR spectroscopy. Eur Radiol 19:1786–1793
Guiu B, Petit JM, Loffroy R et al (2009) Quantification of Liver Fat Content: Comparison of Triple-Echo Chemical Shift Gradient-Echo Imaging and in Vivo Proton MR Spectroscopy. Radiology 250:95–102
Jacqueminet S, Lebray P, Morra R et al (2008) Screening for liver fibrosis by using a noninvasive biomarker in patients with diabetes. Clin Gastroenterol Hepatol 6:828–831
Poynard T, Morra R, Halfon P et al (2007) Meta-analyses of FibroTest diagnostic value in chronic liver disease. BMC Gastroenterol 7:40
Ratziu V, Massard J, Charlotte F et al (2006) Diagnostic value of biochemical markers (FibroTest-FibroSURE) for the prediction of liver fibrosis in patients with non-alcoholic fatty liver disease. BMC Gastroenterol 6:6
Pekar J, Ligeti L, Ruttner Z et al (1991) In vivo measurement of cerebral oxygen consumption and blood flow using 17O magnetic resonance imaging. Magn Reson Med 21:313–319
Wirestam R, Brockstedt S, Lindgren A et al (1997) The perfusion fraction in volunteers and in patients with ischaemic stroke. Acta Radiol 38:961–964
Williams RL (2000) A note on robust variance estimation for cluster-correlated data. Biometrics 56:645–646
Motulsky H (2004) Fitting Models to Biological Data Using Linear and Nonlinear Regression : A Practical Guide to Curve Fitting
Anderson DR (2008) Model based inference in the life sciences: a primer on evidence.
Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M (1986) MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161:401–407
Rani HP, Sheu TW, Chang TM, Liang PC (2006) Numerical investigation of non-Newtonian microcirculatory blood flow in hepatic lobule. J Biomech 39:551–563
Duong TQ, Kim SG (2000) In vivo MR measurements of regional arterial and venous blood volume fractions in intact rat brain. Magn Reson Med 43:393–402
Hayashi T, Miyati T, Takahashi J et al (2014) Diffusion analysis with triexponential function in hepatic steatosis. Radiol Phys Technol 7:89–94
Chow AM, Gao DS, Fan SJ et al (2012) Liver fibrosis: an intravoxel incoherent motion (IVIM) study. J Magn Reson Imaging 36:159–167
Colagrande S, Pasquinelli F, Mazzoni LN, Belli G, Virgili G (2010) MR-diffusion weighted imaging of healthy liver parenchyma: repeatability and reproducibility of apparent diffusion coefficient measurement. J Magn Reson Imaging 31:912–920
Guiu B, Petit JM, Loffroy R et al (2011) Liver methylene fraction by dual- and triple-echo gradient-echo imaging at 3.0 T: Correlation with proton MR spectroscopy and estimation of robustness after SPIO administration. J Magn Reson Imaging 33:119–127
Hussain HK, Chenevert TL, Londy FJ et al (2005) Hepatic fat fraction: MR imaging for quantitative measurement and display–early experience. Radiology 237:1048–1055
Acknowledgements
The scientific guarantor of this publication is Boris Guiu. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
1H-MR Spectroscopy
1H-MRS was performed in all patients. Semiautomated optimization of gradient shimming followed by manual adjustment of central frequency was performed, and water line widths of less than 25Hz were obtained. Water suppression was not performed for any of the sequences.
Single-voxel MR spectroscopic data were acquired using seven breath-hold point-resolved spatially localized spectroscopic (PRESS) pulse sequences (repetition time, 5000 msec; three acquisitions; 2048 data points over 1250 Hz spectral width; and acquisition time, 15 sec) with echo times of 30, 40, 50, 60, 80, 100, and 135 msec to measure the T2 relaxation times of water and methylene (CH2). A long TR was used to minimize T1 effects. Each breath-hold lasted 15 sec.
In all patients, the same 30*30*30-mm (27 ml) voxel was used for these seven sequences and was positioned obliquely on segment VII on the transverse low-T1-weighted section (thus avoiding extra-hepatic fat, large hepatic vessels, and organs adjacent to the liver).
1H-MR spectroscopic data analysis
The Java-based MR user interface spectroscopic analysis package (jMRUI; A van den Boogaart, Catholic University, Leuven, Belgium) was used for the time-domain analysis. Metabolite signals were analyzed using the Advanced Magnetic Resonance (AMARES) fitting algorithm within jMRUI. We measured the water peak at 4.76 ppm and the methylene peak at 1.33 ppm. Spectra were used only if homogeneity after shimming, measured as the full width at 50 % peak height, was better than 25 Hz. Peak integrals were quantified by fitting to a Gaussian line shape.
T2 relaxation times of both metabolites were determined from their peak amplitudes at each echo time using an exponential least-squares fitting algorithm. The peak areas of the methylene and water signals were then corrected for T2 effects (i.e., theoretical peak areas with 0 echo time), using the individually calculated T2 relaxation times.
LFC was calculated as follows:
where A0msec_CH2 and A0msec_WATER were the areas of the methylene and water peaks, respectively, corrected for both T1 and T2 effects.
Triple-echo acquisition
A transverse breath-hold T1-weighted two-dimensional triple-echo spoiled gradient-echo sequence was performed through the liver with the following parameters: repetition time (msec)/echo time (msec) of 192/2.46 (in-phase [IP1]), 3.69 (opposed-phase [OP]), and 4.92 (in-phase [IP2]); flip angle, 60°; section thickness, 6 mm; intersection gap, 1.2 mm; matrix, 256*192; number of sections, 25; and acquisition time, 34 seconds. Parallel imaging (with an acceleration factor of 2) was performed using generalized autocalibrating partially parallel acquisition (GRAPPA; Siemens Medical Solutions Erlangen, Germany). Two separate breath-holds (each lasting 17 seconds) were needed to cover the entire liver volume.
Measurement of T2*
An ROI of 1–2 cm in diameter was drawn in the liver (avoiding large vessels, bile ducts or extra-hepatic areas) in five slices. The signal intensity (SI) in these five ROIs was averaged and recorded for IP1 (TE, 2.46 msec) and IP2 (TE, 4.92 msec) T1-weighted MR images. We used the copy-and-paste function of the workstation (Leonardo; Siemens Medical Solutions) to draw exactly the same ROIs at the same locations on IP images.
As previously reported [37, 38], the IP1 and IP2 images were used to estimate T2* relaxation time.
Rights and permissions
About this article
Cite this article
Cercueil, JP., Petit, JM., Nougaret, S. et al. Intravoxel incoherent motion diffusion-weighted imaging in the liver: comparison of mono-, bi- and tri-exponential modelling at 3.0-T. Eur Radiol 25, 1541–1550 (2015). https://doi.org/10.1007/s00330-014-3554-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3554-6