Abstract
Mycobacterium tuberculosis (M. tuberculosis) is an intracellular pathogen causing long-term infection in humans that mainly attacks macrophages and can escape from the immune system with the various mechanisms. The only FDA-approved vaccine against M. tuberculosis (MTB) is Mycobacterium bovis bacillus Calmette-Guérin (BCG). The protection of this vaccine typically lasts 10–15 years. Due to the increasing number of people becoming ill with MTB each year worldwide, the need to develop a new effective treatment against the disease has been increased. During the past two decades, the research budget for TB vaccine has quadrupled to over half a billion dollars. Most of these research projects were based on amplifying and stimulating the response of T-cells and developing the subunit vaccines. Additionally, these studies have demonstrated that secretory and immunogenic proteins of MTB play a key role in the pathogenesis of the bacteria. Therefore, these proteins were used to develop the new subunit vaccines. In this review, based on the use of these proteins in the successful new subunit vaccines, the PPE44, HSPX, CFP-10 and ESAT-6 antigens were selected and the role of these antigens in designing and developing new subunit vaccines against TB and for the prevention of TB were investigated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mycobacterium tuberculosis (M. tuberculosis) as a human pathogen is the causative agent of pulmonary Tuberculosis (TB). TB is considered as an urgent disease according to the World Health Organization (WHO) [1, 2]. The WHO global TB report 2020 shows that, approximately, 10 million people fell ill with TB worldwide and 1.5 million people died from TB in the same year [3]. Additionally, the WHO report demonstrates that approximately one-third of the world's population infected with TB bacteria [4]. Despite the identification of the bacterium responsible for the development of the disease, as well as excellent therapeutic methods and scientific advances, TB still remains an important health-threatening problem. M. tuberculosis (MTB) grows slowly, having a very flexible cell wall, has a highly contagious nature and has several strategies to escape the immune system [1, 2]. Notwithstanding, directly observed treatment, short-course (DOTS, also known as TB-DOTS) control strategy and vaccination with BCG, TB still has more pathogenic factors than other infectious agents [3, 4]. In addition, one of the most alarming factors in TB patients, also found in patients with HIV, is the emergence of multi-drug resistant species [5]. Many new methods against TB have been developed within the last 25 years. Today, the principles of the molecular invasion, factors involved in the severity of the disease and the activation of TB are also identified which are essential for the survival and proliferation of the causative agents within macrophage cells [5, 6]. Nowadays, vaccination is necessary to control infectious diseases and have drastically reduced the rate of mortality caused by them throughout the world such as measles, mumps, polio and diphtheria. The WHO estimates that 80% of all infectious diseases in the world are related to the deaths of more than 20 million people globally [5]. However, vaccines play a key role in controlling infectious diseases, which are cost-effective. One of the most successful vaccines produced is inactivated/killed vaccines that contain whole bacteria or viruses that are killed or functionally altered so they cannot reproduce. As it is known, inactivated/killed vaccines do not contain any live bacteria or viruses to cause disease, even in people with extremely weakened immune systems. The killed vaccines have some advantages over the live attenuated vaccines; the most important benefits are as follows: (1) producing high-level protection against the specific diseases; (2) unlike attenuated vaccines, there is no risk for reversion and (3) there is no need to store these vaccines at low temperatures. However, inactivated vaccines have some distinct disadvantages including (1) not always elicit strong or long-lasting immune responses and for this reason, there is a need for regular booster injections; (2) the treatment processes involved in inactivation of a vaccine is quite expensive comparing to other vaccines [7, 8], therefore, no promising killed vaccine against TB is developed.
Up till now, old or first-generation vaccines against TB were synthesized from live and attenuated microorganisms, which had several problems. Some ongoing research projects have designed cost-effective vaccines with higher viability that can stimulate the immune system against a specific pathogen. Currently, the attenuated strain of Mycobacterium bovis (M. bovis) bacillus Calmette-Guérin (BCG) is used in many countries to generate immunity. This vaccine is the only approved vaccine for humans. The efficacy of this vaccine varies widely throughout the world and has shown efficacy ranges from 0 to 80% [9, 10].
Additionally, the BCG vaccine induces immunity in children, while it has low effects on the prevention of adult pulmonary TB. For this reason, the production of new vaccines that are more beneficial than BCG is highly required for preventing TB. Vaccines, such as viral vectors, DNA vaccines, subunit vaccines, attenuated M. tuberculosis and the recombinant BCG are among the most important newly designed vaccines in the last 20 years [9,10,11,12] (Table 1 and Fig. 1). Nowadays, bioinformatics and immunoinformatics have accelerated the development of novel vaccine candidates against infectious disease [11,12,13] as well as against TB [14, 15].
M. tuberculosis is a facultative intracellular bacterium and the main way that bacterium enters the body is the respiratory tract. The primary cells that fight this pathogen are the alveolar macrophages and different types of T-cells must be activated to overcome bacterial resistance against host defense system. CD4+ T-cells have a role in the production of various types of cytokines, such as IFN-γ and TNF-α. CD8+ T-cells play an important role in inducing appropriate immune responses against M. tuberculosis through cytotoxic activity and induction of programmed death in infected cells. Cellular immunity is the basis of host responses against TB infection. Recent studies have also highlighted the importance of the innate and humoral immune systems in controlling TB infection. By providing accurate knowledge about immune systems, novel strategies for the design and the development of a new generation of vaccines and drugs are attained [26, 27].
Nowadays, different antigens are used to develop various vaccines against TB. Among all, subunit vaccines are one of the most prominent vaccines to be used here and most recent research has focused on the main marker antigens of M. tuberculosis such as PPE44, HSPX, ESAT-6 and CFP-10 for designing these vaccines [23, 28]. This paper investigated the role and performance of these antigens in designing vaccines against TB.
Selection of the Antigens
Several studies have demonstrated that secretory and immunogenic proteins of M. tuberculosis, such as RV2660c, RV1813c, PPE42, PepA, PPE18, EspD, EspC, EspF, EspR, Ag85, RV2608, Rv3619, RV1813, RV3620, PPE44, HSPX, ESAT-6 and CFP-10 play a key role in the pathogenesis of M. tuberculosis [21, 24, 28]. Furthermore, the activation of T-cells by these antigens suggests the suitability of these antigens as candidates for vaccine production against M. tuberculosis. Some of these antigens are used alone or in combination to develop subunit vaccines. Although a number of these vaccines are currently being evaluated in clinical trials, investigation for producing new vaccines is useful against this pathogen. Therefore, in this study, we have tried to evaluate these antigens (PPE44, HSPX, ESAT-6 and CFP-10) as far as possible.
An Overview of Antigens
PPE44 is one of the important antigens in vaccination of MTB. This protein is a member of PPE (Pro-Pro-Glu) protein family which is unique to mycobacteria. Named after the conserved proline (P) and glutamic acid (E) residues in their n‐terminal domains, these proteins are suggested to perform wide‐ranging roles in virulence and immune modulation [29, 30]. PPE44 with the Pro-Pro-Glu epitope at the n-terminus of the protein that is exclusively detectable by MHC I and MHC II and its nucleotide sequence found only in MTB complex (MTBC) defined this protein as a potential candidate agent for MTB vaccination [31].
Another protein that is suitable for candidate subunit vaccines is heat shock protein X (HSPX). Under the stress condition such as nutrient scarcity, the presence of nitric oxide and hypoxia and during the lag phase the produced HSPX can reach to 25% of the total bacterial protein [32]. This protein is able to escape from the host innate immune system by increasing the stability of the proteins. On the other hand, the cells overexpressing this gene grow more slowly than wild-type cells and are less susceptible to autolysis following saturation of the culture in vitro, suggesting that HSPX may slow down the growth rate of M. tuberculosis in culture and contribute to the spread of TB during macrophage infection [33, 34]. Due to the properties of HSPX to activate both cellular and humoral immune responses and strong induction of Th1 cytokines such as TNF-α and IFN-γ [35, 36], this protein is a good candidate for vaccination against M. tuberculosis.
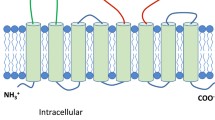
The 6-kDa early-secreted antigenic target (ESAT-6) of M. tuberculosis is one of the important antigens presented in this study. This protein was first identified as a potent T-cell antigen and now is recognized as a pore-forming toxin that is essential for virulence of M. tuberculosis. ESAT-6 is secreted through the ESX-1 secretion system (Type VII) of M. tuberculosis. It has been implicated in mediating mycobacterial cytosolic translocation within the host macrophages by rupturing the phagosomal membranes. ESAT-6 is an abundantly secreted protein of M. tuberculosis which considered as an important virulence factor, deactivation of which results in lower virulence of MBT. ESAT-6 alone or in complex with its chaperone culture filtrate protein-10 (CFP-10), is known to modulate host immune responses. ESAT-6/ESAT-6: CFP-10 can enter the endoplasmic reticulum (ER) where it dissociates Beta-2 microglobulin (β2M) from pMHC-I complexes to inhibit cell surface expression of MHC-I-β2M complexes, resulting in downregulation of class I-mediated antigen presentation [37, 38]. The other secreted antigen that is important in vaccination of M. tuberculosis is Cyan Fluorescent Protein-10 (CFP-10). This protein forms a 1:1 heterodimeric complex with ESAT-6. CFP-10 has been described as a chaperone protein for ESAT-6. The ESAT-6: CFP-10 complex activates the human neutrophils and transiently induces the release of Ca2+ [39, 40].
The ESAT-6 and CFP-10 are expressed by ESXA (RV3875) and ESXB (RV3874) genes, respectively. The genes encoding these proteins are adjacent to each other and are located in the RD1 (Region of Difference1) locus [5, 21].
The ESX family in M. tuberculosis consists of 23 members and based on high sequence homology divided into three distinct subfamilies. The ESX protein contain about 100 amino acids [41] and are potently recognized by both CD4+ and CD8+ that are very attractive target against TB. In addition, as ESAT-6 and CFP-10 seem to be essential for the growth and pathogenicity of M. tuberculosis and since some of these proteins are omitted in BCG, therefore, this vaccine has low efficacy in immunization of animals and humans. As, immunizations with a single ESX antigen preparation have been inadequate for controlling TB, many studies have described that levels of protection and pathogen-specific cellular immunity can be enhanced by combining ESX antigens with other TB-associated antigens [41, 42]. The RD1 locus is a 9.5-Kbp molecular weight region of the M. tuberculosis genome consisting of nine genes (RV3871-RV3879) encoding protective antigens or virulence antigens of the bacterium [5, 21, 43]. The complex of these proteins is degraded in the acidic pH of the macrophage phagosome and then each of these proteins is coupled to the phagosomal membrane causing lysis. Consequently, it appears that these proteins trigger the entry of bacteria from the phagosome into the cytosol and eventually to CD8+ T-cells [22, 44].
In addition to ESAT-6 and CFP-10, several studies have demonstrated that other secretory proteins, such as PPE44 and HSPX play a key role in the pathogenesis of M. tuberculosis and are also involved in activation of T-cells, suggesting the suitability of these antigens as candidates for vaccine preparation.
To increase and stimulate the response of T-cells, several subunit vaccines against M. tuberculosis have been studied and developed [23]. The advantages of subunit vaccines are their safeness, having well-known protein components, their ability to be standardized and the applicability of the protective antigens of M. tuberculosis, leading to the increased response of T-cells. Thus, the increase of the antigen diversity in subunit vaccines enhances the vaccine performance against TB, it must also ensure that the selected antigens are detected by T-cells in different human populations [45].
PPE44 Members and their Role
The PPE family has 69 members with conserved n-terminal and variable c-terminal. PE44 is a member of the MTB PPE proteins that has consecutive repeated sequences [46]. This family contains approximately 10% of the MTB genome [47]. The comparative genomic assay reveals that the PPE protein is largely restricted to Mycobacterium genus [48], particularly in virulent species of Mycobacterium (TB, M. bovis, M. ulcerans, M. marinum and M. canis), playing a unique role in the virulence-associated sequence and the survival of Mycobacterium. Based on the number of repetitions of C regions, the PPE family can be divided into four subfamilies:
-
1
The PPE-SV family has 24 members containing the conventional motifs of GLY-XX-SER and XX-TRP between 300 and 350 positions.
-
2
The PPE-MPRT family has a repeated sequence of ASN-X-GLY-X-GLY-ASN-X-GLY and a repeated sequence of GCCGGTGTTG in the C-terminal separated by 5 bp spacers.
-
3
The PPE-PPW family has 44 conserved amino acids with a conserved sequence of GLY-Phe-GLY-X-TR and X-XPRO-X-X-TRP in the C-terminal [49].
-
4
The fourth subfamily has 12 members, which has a low consistency in the C-terminal region.
It should be noted that the c-terminal region of PPE has 225 amino acids. The PPE-MPRT protein, which is similar to the PE-PGRS gene, contains a motif in n-terminal and an amino acid serine A/B for hydrolysis [50]. These hydrolyses are required for cell protection and to make cell walls impermeable and to enhance the virulence of the bacteria. Each type of PPE has a specific alpha helix or random coil [51]. PPE family proteins have played an important role in the development of antigenic diversity. Immunoassays on PPE almost showed the same response as purified protein derivative (PPD) to patients’ cell lines [52].
Nowadays, new sciences such as systems biology are very influential in designing and developing different purposes. One of the methods of systems biology is to find the protein–protein network (PPI) which can be useful for anticipating the role of the targeted protein in biology such as determining the biomarker, subunit vaccine, cancers and etc. In the PPI network, one of the proteins that are extremely important and can interact with other proteins in the network is PPE. Understanding the function of this protein is very important in the development of the new vaccine such as subunit vaccines [53]. PPE44 is a member of the M. tuberculosis PPE family that has interaction with ten members of this family (Fig. 2).
Protein–protein networks between PPE44 and PPE families analyzed with STRING database (https://string-db.org)
The Mechanism of the Secretion and Molecular Structure of PPE Genes
Proving the existence of a large family of PE/PPE proteins was an important discovery in the molecular biology. PE/PPE family genes are commonly considered as a gene complex and have important effects on each other since they are cell surface components [54, 55]. Studies have shown that PE and PPE genes are transmitted as part of the ESX gene secretion system (the details will be discussed later). Further evidence is available to determine the PPE position, the composition of amino acids and their sequences, indicating the composition of amino acids, which will help to predict their position on the cell surface [52].
Pajon et al. predicted that the beta proteins in the MTB genome included forty PPE proteins with a beta structure [56]. Beta proteins (beta-barrel or beta-sheet) are a group of surface proteins harbored in the outer membrane of bacteria. They are creating a channel by forming anti-parallel beta strands which cover all over the outer membrane. These proteins have various functions such as transport of ions, enzymes, siderophores and structural proteins and mediating flux of metabolites. As they play an essential role in the bacterial virulence, it would be of great interest to use them for the development of the vaccines [56, 57]. These observations support the hypothesis that PPE proteins associated with PE proteins are possibly translated on the cell surface. The following section in this study regarding evolutionary genetic topics noted that the evolution of PPE genes and associated genes such as PE was in regions proximate to ESX [58].
Genes such as PPE68 are located in an area within the ESX-1 region [59]. The PPE68 protein in M. tuberculosis has been reported to be strongly associated with the cell wall [52, 60].
Additionally, research on PPE68 reported its confrontation with the ESX1 secretion system [60, 61]. Other studies suggested that PPE68 acts as an ESX-1 regulator [62] and the ESX-1 has the potential role in the secretion of ESX-5; moreover, the presence of PE/PPE and the secretion of PPE by ESX-5 is demonstrated, while some believe that PPE is used by the ESX secretion system [63, 64]. The complex structure of PPE demonstrates the potential role of this compound in signal transduction and the PPE protein in this set has structural homology with the serine chemoreceptor [65]. These findings reveal the possible role of the PPE protein and its associated gene, PE, in host immunity and signaling [66].
PPE Immunity Review
The PPE protein and its accompanying gene, PE, are important factors in virulence enhancement and a possible source of antigenic variation. PPE can be the first line of defense against TB owing to their role in the immune system and their ability to modulate macrophages function. Macrophages have a set of antimicrobial mechanisms trying to defend against the microbial agents by producing IFN-γ and TNF-α, nitrogen, reactive oxygen mediators and cytokines [67]. Although macrophages activate T-cells against TB to control and eliminate the infection, they can also serve as the main host cell for TB growth and survival [68, 69]. When macrophages infected with TB, some cytokines such as TNF-α, IL-12 family, IL-6, IL-1α/β, and IL-10 are secreted which are important to control MTB infection. Some proteins secreted by MTB such as CFP-10 and ESAT6, SecA 1/2 proteins and the eukaryotic like serine/threonine protein kinase G (PknG) interfere with macrophage apoptosis and phagosomal maturation. A few days after escaping from macrophages, MTB begins to multiply to spread the infection. Some studies have demonstrated that region of difference 1 (RD1) and ESAT-6 in the MTB are required to escape from phagocytosis [70, 71].
It has not yet been clarified that this PPE protein is directly related to the proliferation and intracellular survival of TB or virulence enhancement by impairing the function of the immune system via macrophages [72]. Another report showed that the inactivation of PPE46 can weaken M. tuberculosis in the body [73]. Moreover, a different study showed that the PPE gene deletion caused impairment of MTB growth in macrophages [72].
Various studies reinforce the view that PE/PPE genes contribute to the survival of MTB. After conducting several studies by analyzing the proteasome and considering the microarray results, Brosch et al. revealed the MTB response to nutritional stress [74]. Studies on four PPE members 24 h after infection have indicated that the presence of these proteins is necessary to maintain the long-term survival of bacteria under nutritional stress [61].
In addition, Dillon et al. indicated that the PPE protein of the RV1196 gene during the infection was better expressed in rats vaccinated with RV1196 DNA vaccine and had better function to control TB [75].
In another study, the PPE44 protein expressed by the RV2770C gene was subcutaneously or intravenously injected into BALB/C mice previously vaccinated with the BCG vaccine. The results demonstrated that the PPE44 gene-induced Th2 immune responses and IgG1 and IgG2 immunoglobulin as well as delayed sensitivity responses developed [76].
Some studies indicate that the PPE18 (RV1196) similar to PPD triggers the T-cell response which in turn stimulates T helper cells and macrophages to produce IL-10 and IL-12, respectively [73].
Other studies have revealed that PPE44 and PPE18 sometimes trigger the response of Th2 cells under certain conditions expressing IL-10, 1L-12 cytokines by modulating the levels of macrophages. The evidence refers to their role in enhancing virulence. The genes encoding polymorphic PPE proteins have been demonstrated to cause extensive antigenic changes in Mycobacterium [73, 77]. The frequency of variation in these proteins is very high which help them to escape from the immune system [78].
Heat shock protein X (HSPX) or M. tuberculosis α-Crystallin is a protein with a molecular weight of 36.1 kDa encoded by the RV2031c gene [79]. It acts as an important antigen in the latent phase of M. tuberculosis and is expressed mainly by non-replicating bacilli. HSPX keeps the bacteria alive in the latent period of the disease as well as infection and is able to induce stronger immune responses in patients with latent TB [79].
HSPX, known as M. tuberculosis alpha-crystalline, is a protein with high immunogenicity that is a potent stimulant for Th1 responses in individuals exposed to TB [79]. This protein acts as a molecular chaperone similar to its human analog. Furthermore, the high production of this protein in hypoxia and microaerophilic conditions suggests that it also plays a role in developing TB granuloma [80]. Molecular chaperons have different functions in bacteria, including proper folding of newly synthesized proteins, protein transitions and inhibition of aggregation during thermal shock, degradation and reduction of aggregated proteins and recovery of the proteins that are damaged or have inappropriate folding due to stresses. Therefore, molecular chaperones play a pivotal role in proteome control by interacting, stabilizing and remodeling various proteins [81].
HSPX protein is expressed only in M. tuberculosis and is extremely important in the pathogenesis of bacteria. In vitro studies show that HSPX is expressed in hypoxia, causing bacterial stability inside the macrophages. Recently, efforts have been made to produce a vaccine containing this antigen. For example, Roupe V et al. investigated the efficiency of DNA vaccines encoding RV1733c, RV1738, RV2029c, RV2031c HSPX, RV2032 (acg), RV2626c, RV2627c and RV2628 proteins. This vaccine was injected into BALB/c and B6D2 (F1) mice. The results indicated the development of strong humoral and cell-mediated immune (CMI) responses to TB in all antigens except for RV1738. In addition, the strongest CMI response (the production of IFN-γ, IL-2) was related to RV2031c (HSPX) and RV2626c antigens. These findings suggest that latent phase proteins of M. tuberculosis can also be used as antigens to produce the DNA vaccine against TB [82].
Role of HSPX in Immunization
Yuan et al. designed DNA vaccine expressing the fusion protein of Ag85B-ESAT-6-HSPX and studied its performance in mice. In this study, the multi-dose vaccine was injected into BALB/C mice. Two weeks after the last injection, the concentration of IgG, IgG1 and IgG2a antibodies was measured via ELISA. The level of specific anti-HSPX IgG antibodies and the IgG2a/IgG1 ratio were significantly higher than those of antibodies of other proteins. The activation of Th1 cell (CD4+ and CD8+ T-cells) responses suggest that the increased production of IFN-γ and TNF-α is owing to activation of protective cell-mediated immunity [83].
In addition, in another study, recombinant rBCG strains expressing HSPX and HSPX DNA vaccine were injected into mice and guinea pigs through the prime-boost technique. Immunological assessments demonstrated that the levels of IL-12, TGFβ, IL-10 cytokines were elevated and the microbial load in the lung was reduced [84].
It has been proven that the mycobacterial infection induces CD4+ and CD8+ T-cells responses. CD8+ T-cells are activated by peptides presented by Major Histocompatibility Complex-I (MHC-I) on the surface of infected cells [85].
Shi et al. conducted one study on the recombinant vaccine expressing the HSPX protein (rBCG). According to their findings, HSPX protein epitopes in patients with TB are detected by CD4+ and CD8+ T-cells. Furthermore, mice immunized with the DNA vaccine containing HSPX had a strong Th1 immune response induced by this antigen. They suggested that immune responses against HSPX antigen were effective in controlling the M. tuberculosis infection [80]. In addition, Shi et al. in another survey detected the anti-HSPX antibodies in 77% of patients with chronic tuberculosis [86, 87]. They surveyed the HSPX antigen and its epitopes finding that the HSPX gene deletion reduced the virulence of the pathogenic strain of M. tuberculosis. They reported that attenuated strains, including strains reducing HSPX expression, could be used as anti-tuberculosis vaccines. According to their studies, HSPX (16.3 kDa) is a potentially important component ensuring the survival of M. tuberculosis in the latent phase of human infection [86].
In another study, Yuan et al. evaluated the immunogenic and protective effects of the fusion protein of Ag85B: ESAT-6: HSPX in mice. They found that the vaccine containing the mentioned recombinant proteins was a strong stimulant of humoral immune responses and acted as a strong T-cell inducer. They also measured IgG levels using ELISA two weeks after the last immunization of mice and observed that antibody level was significantly higher in the vaccine group than in other groups. To evaluate cell-mediated immunity, the frequency of CD4+ and CD8+ T-cell in peripheral blood and γδ T-cells was investigated two weeks after the last immunization. Their findings demonstrated that immunization of mice with fusion protein significantly induced CD4+ and CD8+ T-cells. Furthermore, an assessment of M. tuberculosis colony counts in the spleen of different groups of mice revealed that recombinant proteins induced Th1 response and inhibited the growth and proliferation of M. tuberculosis compared to BCG [83].
Martinus et al. conducted one study to evaluate the protective effect of Ag85A and HSPX on controlling TB progression. They concluded that Ag85A and HSPX antigens were able to induce IFN-γ which is the main cytokine in the development of immunity against TB. They stated that when the combination of the two above-mentioned antigens in mice was applied, the IFN-γ response was stronger than the sole antigens. They found that the combination of these antigens significantly reduced the bacterial count in the lung and spleen of the mouse. Therefore, Ag85A and HSPX are suitable candidates for vaccine production [88].
Further, Niu et al. developed and evaluated a multi-stage subunit vaccine consisted of Mtb10.4: HSPX. According to their reports, the obtained recombinant protein is able to induce higher levels of immune response. To evaluate the immunogenic effect, they injected each molecule with an emulsified adjuvant to the mice, showing that the IFN-γ and IL-17 production levels are much higher than the levels when BCG is used. To evaluate the humoral immune response, they measured the serum level of IgG antibodies against HSPX by ELISA and the IgG level was much higher than that of the BCG vaccine [89].
HSPX (HSP16.3( and its Role in Vaccine Design
HSPX (or the HSP16.3) is a latency-related antigen for multistage vaccines. Small heat shock proteins (sHSPs) are one of the five families of proteins acting as a molecular chaperone. sHSPs possess a universally conserved alpha-crystallin domain, hence, also known as the alpha-crystallin family. HSPs, play a key role in handling damaged proteins or intracellular protein accumulation and their association with virulence of bacteria, including M. tuberculosis, has been studied. Expression of many of them increases under stress conditions in TB disease. The role of HSP in the introduction of antigen is to activate lymphocytes and macrophages [90]. The virulence of M. tuberculosis depends on several genes using the macrophage system and its modification for its successful survival. Therefore, the use of HSPs can be important to treat TB [46] and HSPX is one of the most prominent HSPs in this case. HSPX in TB was primarily identified as 14-kDa and 16-kDa antigens and then classified as a molecular chaperone known as alpha-crystalline. These small HSPs prevent the accumulation and denaturation of proteins and wrong folding under stress conditions [90].
Later, Cunningham et al. investigated and reported the major role of this HSP in MTB. They stated that HSPX was able to produce a strong CMI response and delayed-type hypersensitivity (DTH) in mice and guinea pigs [90, 91]. HSPX is produced as the dominant protein in the stationary and latent phases of TB infection and in response to the increased stress [83]. These proteins are one of the most important antigens expressed by granulomas which stimulate the immune responses. HSPX is a heat-sensitive intramembrane protein expressed under the control of the transcription factor SigH. This transcription factor is responsible for some genes produced in response to heat or oxidative shock. Studies have indicated that the HSPX gene is the most important gene expressed in the latent form of the bacteria. Therefore, it is called the hypoxia reporter gene (HRG). There is a serological test using an antibody to detect the latent form of the bacterium against this protein. Accordingly, subunit vaccines appear to be suitable to be used against the latent form of the disease [33].
ESAT-6 and CFP-10 Antigens
The M. tuberculosis strain H37Rv genome comprises 4,411,529 base pairs including about 4000 genes and approximately 3900 proteins that are isolated from the bacterial culture supernatant [92]. This genome consists of 36 regions of differences RDs (region of differences) [1, 2] and among these regions, the RD1 locus plays a key role in the virulence of the bacterium. Although, this region of the gene is present in the pathogenic strains of M. tuberculosis and M. bovis, it has been deleted in the BCG vaccine strain. The RD1 locus is a 25.3-Kbp molecular weight region of the M. tuberculosis genome consisting of nine genes (RV3871-RV3879) encoding protective antigens or virulence antigens of the bacterium [14].
One of the proteins encoded by the RD1 region but the early secretory antigenic target-6 (ESAT-6) and CFP-10 are encoded by the RV3875 (ESXA) gene and the RV3874 (ESXB) gene, respectively (Fig. 3). These two genes form a heterodimer complex with a ratio of 1: 1 [93].
On the other hand, a number of studies suggest that the secretory proteins of ESAT-6 and CFP-10 play a crucial role in the pathogenesis of M. tuberculosis. Furthermore, the activation of T-cells by these antigens proves their suitability for the vaccine [79].
The CFP-10 activates and aggregates cytotoxic T lymphocytes and extends the granuloma tissue in humans and mice infected with M. tuberculosis [83].
The secretory proteins of ESAT-6 and CFP-10 are produced only in the early stages of TB infection. Deletion of genes encoding secretory proteins of the pathogenic strains is proven to reduce bacterial virulence [80]. To date, more than 20 different immunodominant antigens have been identified in M. tuberculosis. The use of recombinant protein viruses and viral vector vaccines induces relative protections against TB [81].
Recently, several immunogenic regions of CFP-10 have been identified in humans. Specifically, CFP-10 peptides are capable of stimulating and producing IFN-γ, resulting in the activation of cytotoxic T-cells. The CD4+ T-cell plays a crucial role in developing immune responses against TB in humans. Moreover, the use of appropriate antigens from M. tuberculosis causing proper protective responses, leads to a better understanding of designing an optimal vaccine against TB [69, 70]. The human immune response against TB depends on several factors of which the Th1 response is of great importance. Moreover, it is essential to stimulate and produce IFN-γ [81].
Several studies indicate that M. tuberculosis expresses different proteins during different stages of infection that are specific to each stage. In fact, the immune system of people with active TB may identify and respond to antigens specific for the acute phase of infection and those infected with latent TB can identify and respond to latent antigens of M. tuberculosis. For example, ESAT-6 and CFP-10 proteins are accurately detected in individuals with active TB. Accordingly, it is desirable to use multi-stage latent acute phase antigens in designing a vaccine against TB [5]. Additionally, the results of recent studies suggest that new TB vaccines should contain proliferating bacteria and latency-associated multi-stage antigens [81]. Okkels et al. reported that the secretory proteins of ESAT-6 and CFP-10 were capable of producing cytotoxic T-cells in response to IFN-γ production. They also stated that the main immunogenic antigen was related to the M. tuberculosis detected by T-cells in individuals infected with TB. Recent studies have reported that several immunogenic regions of the CFP-10 antigen are identified for humans. For example, CFP-10 peptides are capable of stimulating and producing IFN-γ and activating cytotoxic T-cells [60]. This study did not respond to some questions posed by researchers including, do inflammatory reactions cause damage to the living creature owing to the cytotoxic T-cells stimulated by IFN-γ production? Does the inflammatory effect prevent the sustained effect of the vaccine?
Maue et al. demonstrated that administration of ESAT-6: CFP-10 DNA vaccine induced an effective immune response in calves infected with M. bovis. This study showed that administration of the BCG vaccine together with ESAT-6: CFP-10 DNA vaccine induced more severe immune responses compared to BCG alone [94]. The researcher suggested that the presence of ESAT-6: CFP-10 as a booster can be combined with BCG to increase the responsiveness of immune mediators in the body.
The current research team also examined the protective and immunoglobulin effects of a DNA vaccine expressing CFP-10 in mice. The results of this study proved that the CFP-10 protein stimulated cytotoxic T lymphocytes. In addition, this vaccine is able to prevent the proliferation of M. tuberculosis in the lung and spleen [94].
Kamath et al. reported that the secretory protein of CFP-10 was able to stimulate T lymphocytes. They also stated that some CFP-10 epitopes were capable of stimulating and producing IFN-γ and activating cytotoxic T-cells [81]. The effects of these antigens on the stimulation of B-lymphocytes need to be addressed in this paper.
Dietrich et al. showed that vaccination with the ESAT-6: Ag85B fusion protein induced highly effective immune responses. This effect has been studied in animal and non-human primate models. This fusion molecule is also effective even as a DNA vaccine. Intranasal administration of the Ag85B: ESAT-6 combination vaccine with LTK63 mucosal adjuvant was also tested. Vaccination with LTK63/Ag85B: ESAT-6 resulted in a strong Th1 response, followed by IFN-γ secretion from TCD+4 cells and thus sustained protection against TB infection [95].
Moradi et al. evaluated the protective effect and immunogenic activity of novel recombinant fusion protein from M. tuberculosis consisting of ESAT-6 and the short domain of the c-terminus of the HSP70 thermal shock protein after its expression in the mouse model. The results showed that the level of IFN-γ and titer of specific antibodies in the fusion protein was higher than that in ESAT-6 alone. Therefore, this fusion protein (E6H70c) was suggested as a candidate for vaccine preparation [96]. CFP-10 and ESAT-6 proteins are produced only in the early stages of TB infection. It is proven that deletion of the relevant genes in pathogenic strains reduces bacterial virulence.
Conclusion
Most researchers declare that complete eradication of TB is only possible with an effective vaccine, particularly in developing countries with a high incidence of TB and limited financial resources to access the treatment. During the past two decades, the research budget to develop TB vaccine has quadrupled up to over half a billion dollars. Based on the results of various studies, recombinant proteins and DNA vaccines have immunodominant characteristics and are capable of inducing a long-term immunological memory. To evaluate the immune response and protective efficacy of subunit vaccines based on PPE44, HSPX, ESAT-6 and CFP-10 several studies have been carried out. Table 2 demonstrated the results of these studies.
Various studies on recombinant vaccines against TB have demonstrated that PPE44, HSPX, ESAT-6 and CFP-10 antigens can generally play a role in the following items:
-
1.
It has the ability to induce a Th1 lymphocytes-mediated immune response, which is an important criterion to evaluate the efficacy of vaccines against TB.
-
2.
In designing a subunit vaccine against TB, it is important to select an immunodominant antigen that can provide appropriate protective immune responses.
-
3.
It causes a protective immune response in animal cells during conducting various studies, such as vaccination with Mycobacterium smegmatis (M. smegmatis) and DNA vaccines containing PPE44, HSPX, ESAT-6 and CFP-10 antigens.
-
4.
Studies have indicated that the levels of immune mediators such as INF and IL-12 in mice vaccinated with these antigens are significantly higher than those in other compared groups.
-
5.
Activation of the immune system by the mentioned antigens demonstrates that there is always a Th1 protective response accompanied by a response with a lower level induced by Th2. This low level response is reported in various studies that can prevent immunopathological effects of a potent protective CMI system. Furthermore, it may create balance in the immune system after eliminating the infection.
-
6.
Studies have demonstrated that the use of these antigens along with BCG is highly effective in boosting the immunological memory of BCG, suggesting the use of these recombinant proteins to enhance the efficacy of BCG.
-
7.
Based on recent reports and studies conducted on animal models, it has been found that IFN-α is produced from Th1 cells; as a result, these antigens are the most important and effective protection against M. tuberculosis. The produced IFN activates macrophages to kill and eliminate the reproducing bacteria. The production of IL-12 by macrophages and dendritic cells plays a major role in the differentiation of intact T-cells to Th1 lymphocytes. Therefore, increasing the diversity of antigens in subunit vaccines leads to improved efficacy of the vaccine against TB, ensuring that selected antigens will be identified by T-cells of different human populations. Among these, ESAT-6, CFP-10, HSPX and PPE antigens have been employed as the major antigens for subunit vaccines in various studies. Various articles confirm that these antigens have been able to apply their own anti-tuberculosis effectiveness in designing new vaccines. It is hoped that in the near future, these antigens will play a role as subunit vaccines in the different phases of clinical trials to achieve a vaccine with long-term viability. Findings from this review article provide an avenue for future researchers interested in vaccine development against TB
References
Aagaard C, Dietrich J, Doherty M, Andersen P (2009) TB vaccines: current status and future perspectives. Immunol Cell Biol 87(4):279–286
Parida SK, Kaufmann SH (2010) Novel tuberculosis vaccines on the horizon. Curr Opin Immunol 22(3):374–384
Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, Mwaba P et al (2021) Global tuberculosis report 2020–reflections on the global TB burden, treatment and prevention efforts. Int J Infect Dis 113:S7–S12
Farzam B, Fooladi AAI, Izadi M, Hossaini HM, Feizabadi MM (2015) Comparison of cyp141 and IS6110 for detection of Mycobacterium tuberculosis from clinical specimens by PCR. J Infect Public Health 8(1):32–36
Guinn KM, Hickey MJ, Mathur SK, Zakel KL, Grotzke JE, Lewinsohn DM et al (2004) Individual RD1-region genes are required for export of ESAT-6/CFP-10 and for virulence of Mycobacterium tuberculosis. Mol Microbiol 51(2):359–370
Gupta A, Kaul A, Tsolaki AG, Kishore U, Bhakta S (2012) Mycobacterium tuberculosis: immune evasion, latency and reactivation. Immunobiology 217(3):363–374
Beard C (2003) The role of vaccines and vaccination. Avian Dis 47:293–305
Roth JA, Henderson LM (2001) New technology for improved vaccine safety and efficacy. Vet Clin North Am 17(3):585–597
Coler RN, Day TA, Ellis R, Piazza FM, Beckmann AM, Vergara J et al (2018) The TLR-4 agonist adjuvant, GLA-SE, improves magnitude and quality of immune responses elicited by the ID93 tuberculosis vaccine: first-in-human trial. NPJ Vaccines. https://doi.org/10.1038/s41541-018-0057-5
Nieuwenhuizen NE, Kulkarni PS, Shaligram U, Cotton MF, Rentsch CA, Eisele B et al (2017) The recombinant bacille calmette-guérin vaccine VPM1002: ready for clinical efficacy testing. Front Immunol 8:1147
Mahboobi M, Sedighian H, Malekara E, Khalili S, Rahbar MR, Zanoos KA et al (2020) Harnessing an integrative in silico approach to engage highly immunogenic peptides in an antigen design against epsilon toxin (ETX) of clostridium perfringens. Int J Pept Res Ther 27(2):1019–1026
Mahboobi M, Sedighian H, Hedayati CHM, Bambai B, Esmaeil Soofian S, Amani J (2017) Applying bioinformatic tools for modeling and modifying type ii e. Coli l-asparginase to present a better therapeutic agent/drug for acute lymphoblastic leukemia. Int J Cancer Manag 3:10
Moghadam ZM, Halabian R, Sedighian H, Behzadi E, Amani J, Fooladi AAI (2019) Designing and analyzing the structure of DT-STXB fusion protein as an anti-tumor agent: an in silico approach. Iran J Pathol 14(4):305
Shah P, Mistry J, Reche PA, Gatherer D, Flower DR (2018) In silico design of Mycobacterium tuberculosis epitope ensemble vaccines. Mol Immunol 97:56–62
Shahbaaz M, Nkaule A, Christoffels A (2019) Designing novel possible kinase inhibitor derivatives as therapeutics against Mycobacterium tuberculosis: an in silico study. Sci Rep 9(1):1–12
Williams A, Arnold B, Gwynne-Jones DP (2019) Mycobacterium bovis infection of total hip arthroplasty after intravesicular bacillus calmette-guérin. Arthroplast Today 5(4):416–420
Sable SB, Posey JE, Scriba TJ (2019) Tuberculosis vaccine development: progress in clinical evaluation. Clin Microbiol Rev. https://doi.org/10.1128/CMR.00100-19
Hoft DF, Blazevic A, Selimovic A, Turan A, Tennant J, Abate G et al (2016) Safety and immunogenicity of the recombinant BCG vaccine AERAS-422 in healthy BCG-naïve adults: a randomized, active-controlled, first-in-human phase 1 trial. EBioMedicine 7:278–286
Spertini F, Audran R, Chakour R, Karoui O, Steiner-Monard V, Thierry A-C et al (2015) Safety of human immunisation with a live-attenuated Mycobacterium tuberculosis vaccine: a randomised, double-blind, controlled phase I trial. Lancet Respir Med 3(12):953–962
Nemes E, Geldenhuys H, Rozot V, Rutkowski KT, Ratangee F, Bilek N et al (2018) Prevention of M. tuberculosis infection with H4: IC31 vaccine or BCG revaccination. N Engl J Med 379(2):138–49
Van Der Meeren O, Hatherill M, Nduba V, Wilkinson RJ, Muyoyeta M, Van Brakel E et al (2018) Phase 2b controlled trial of M72/AS01E vaccine to prevent tuberculosis. N Engl J Med 379(17):1621–1634
Tameris MD, Hatherill M, Landry BS, Scriba TJ, Snowden MA, Lockhart S et al (2013) Safety and efficacy of MVA85A, a new tuberculosis vaccine, in infants previously vaccinated with BCG: a randomised, placebo-controlled phase 2b trial. The Lancet 381(9871):1021–1028
Duthie MS, Coler RN, Laurance JD, Sampaio LH, Oliveira RM, Sousa ALM et al (2014) Protection against Mycobacterium leprae infection by the ID83/GLA-SE and ID93/GLA-SE vaccines developed for tuberculosis. Infect Immun 82(9):3979–3985
Vekemans J, O’Brien KL, Farrar J (2019) Tuberculosis vaccines: rising opportunities. PLoS Med 16(4):e1002791
Abel B, Tameris M, Mansoor N, Gelderbloem S, Hughes J, Abrahams D et al (2010) The novel tuberculosis vaccine, AERAS-402, induces robust and polyfunctional CD4+ and CD8+ T cells in adults. Am J Respir Crit Care Med 181(12):1407–1417
Munk ME, Kern P, Kaufmann S (1997) Human CD30+ cells are induced by Mycobacterium tuberculosis and present in tuberculosis lesions. Int Immunol 9(5):713–720
Arrigucci R, Lakehal K, Vir P, Handler D, Davidow A, Herrera R et al (2018) Active tuberculosis is characterized by highly differentiated effector memory Th1 cells. Front Immunol 9:2127
Keikha M, Karbalaei M (2019) Can multi-stage recombinant fusion proteins be considered as reliable vaccines against tuberculosis? a letter to the editor. Mod Care J. https://doi.org/10.5812/modernc.91493
Mukhopadhyay S, Balaji KN (2011) The PE and PPE proteins of Mycobacterium tuberculosis. Tuberculosis 91(5):441–447
Wang Q, Boshoff HI, Harrison JR, Ray PC, Green SR, Wyatt PG et al (2020) PE/PPE proteins mediate nutrient transport across the outer membrane of Mycobacterium tuberculosis. Science 367(6482):1147–1151
Bonanni D, Rindi L, Lari N, Garzelli C (2005) Immunogenicity of mycobacterial PPE44 (Rv2770c) in Mycobacterium bovis BCG-infected mice. J Med Microbiol 54(5):443–448
Yousefi-Avarvand A, Tafaghodi M, Soleimanpour S, Khademi F (2018) HspX protein as a candidate vaccine against Mycobacterium tuberculosis: an overview. Front Biol 13(4):293–296
Taylor JL, Wieczorek A, Keyser AR, Grover A, Flinkstrom R, Karls RK et al (2012) HspX-mediated protection against tuberculosis depends on its chaperoning of a mycobacterial molecule. Immunol Cell Biol 90(10):945–954
Wang X, Zhang J, Liang J, Zhang Y, Teng X, Yuan X et al (2015) Protection against Mycobacterium tuberculosis infection offered by a new multistage subunit vaccine correlates with increased number of IFN-γ+ IL-2+ CD4+ and IFN-γ+ CD8+ T cells. PLoS ONE 10(3):e0122560
Rabahi MF, Junqueira-Kipnis AP, Dos Reis MCG, Oelemann W, Conde MB (2007) Humoral response to HspX and GlcB to previous and recent infection by Mycobacterium tuberculosis. BMC Infect Dis 7(1):1–9
Marongiu L, Donini M, Toffali L, Zenaro E, Dusi S (2013) ESAT-6 and HspX improve the effectiveness of BCG to induce human dendritic cells-dependent Th1 and NK cells activation. PLoS ONE 8(10):e75684
Refai A, Gritli S, Barbouche M-R, Essafi M (2018) Mycobacterium tuberculosis virulent factor ESAT-6 drives macrophage differentiation toward the pro-inflammatory M1 phenotype and subsequently switches it to the anti-inflammatory M2 phenotype. Front Cell Infect Microbiol 8:327
Harboe M, Oettinger T, Wiker HG, Rosenkrands I, Andersen P (1996) Evidence for occurrence of the ESAT-6 protein in Mycobacterium tuberculosis and virulent Mycobacterium bovis and for its absence in Mycobacterium bovis BCG. Infect Immun 64(1):16–22
Namvarpour M, Tebianian M, Mansouri R, Ebrahimi SM, Kashkooli S (2019) Comparison of different immunization routes on the immune responses induced by Mycobacterium tuberculosis ESAT-6/CFP-10 recombinant protein. Biologicals 59:6–11
Dillon DC, Alderson MR, Day CH, Bement T, Campos-Neto A, Skeiky YA et al (2000) Molecular and immunological characterization of Mycobacterium tuberculosis CFP-10, an immunodiagnostic antigen missing in Mycobacterium bovis BCG. J Clin Microbiol 38(9):3285–3290
Villarreal DO, Walters J, Laddy DJ, Yan J, Weiner DB (2014) Multivalent TB vaccines targeting the esx gene family generate potent and broad cell-mediated immune responses superior to BCG. Hum Vaccin Immunother 10(8):2188–2198
Bottai D, Brosch R (2009) Mycobacterial PE, PPE and ESX clusters: novel insights into the secretion of these most unusual protein families. Mol Microbiol 73(3):325–328
Leroux-Roels I, Forgus S, De Boever F, Clement F, Demoitié M-A, Mettens P et al (2013) Improved CD4+ T cell responses to Mycobacterium tuberculosis in PPD-negative adults by M72/AS01 as compared to the M72/AS02 and Mtb72F/AS02 tuberculosis candidate vaccine formulations: a randomized trial. Vaccine 31(17):2196–2206
Ndiaye BP, Thienemann F, Ota M, Landry BS, Camara M, Dièye S et al (2015) Safety, immunogenicity, and efficacy of the candidate tuberculosis vaccine MVA85A in healthy adults infected with HIV-1: a randomised, placebo-controlled, phase 2 trial. Lancet Respir Med 3(3):190–200
Russo G, Pappalardo F, Juarez MA, Pennisi M, Cardona PJ, Coler R et al (2019) Evaluation of the efficacy of RUTI and ID93/GLA-SE vaccines in tuberculosis treatment: in silico trial through UISS-TB simulator. arXiv preprint arXiv:191100325
Dey B, Jain R, Khera A, Gupta UD, Katoch V, Ramanathan V et al (2011) Latency antigen α-crystallin based vaccination imparts a robust protection against TB by modulating the dynamics of pulmonary cytokines. PLoS ONE 6(4):e18773
Chakhaiyar P, Nagalakshmi Y, Aruna B, Murthy KJ, Katoch VM, Hasnain SE (2004) Regions of high antigenicity within the hypothetical PPE major polymorphic tandem repeat open-reading frame, Rv2608, show a differential humoral response and a low T cell response in various categories of patients with tuberculosis. J Infect Dis 190(7):1237–1244
Li W, Deng W, Xie J (2019) Expression and regulatory networks of Mycobacterium tuberculosis PE/PPE family antigens. J Cell Physiol 234(6):7742–7751
Rodo MJ, Rozot V, Nemes E, Dintwe O, Hatherill M, Little F et al (2019) A comparison of antigen-specific T cell responses induced by six novel tuberculosis vaccine candidates. PLoS Pathog 15(3):e1007643
Ahmad J, Farhana A, Pancsa R, Arora SK, Srinivasan A, Tyagi AK et al (2018) Contrasting function of structured N-terminal and unstructured C-terminal segments of Mycobacterium tuberculosis PPE37 protein. MBio 9(1):e01712-e1717
Gordon SV, Brosch R, Billault A, Garnier T, Eiglmeier K, Cole ST (1999) Identification of variable regions in the genomes of tubercle bacilli using bacterial artificial chromosome arrays. Mol Microbiol 32(3):643–655
Van Pittius NCG, Sampson SL, Lee H, Kim Y, Van Helden PD, Warren RM (2006) Evolution and expansion of the Mycobacterium tuberculosis PE and PPE multigene families and their association with the duplication of the ESAT-6 (esx) gene cluster regions. BMC Evol Biol 6(1):95
Russo G, Reche P, Pennisi M, Pappalardo F (2020) The combination of artificial intelligence and systems biology for intelligent vaccine design. Expert Opin Drug Discov 15(11):1267–1281
De Jonge MI, Pehau-Arnaudet G, Fretz MM, Romain F, Bottai D, Brodin P et al (2007) ESAT-6 from Mycobacterium tuberculosis dissociates from its putative chaperone CFP-10 under acidic conditions and exhibits membrane-lysing activity. J Bacteriol 189(16):6028–6034
Scherrer S, Landolt P, Friedel U, Stephan R (2019) Distribution and expression of esat-6 and cfp-10 in non-tuberculous mycobacteria isolated from lymph nodes of slaughtered cattle in Switzerland. J Vet Diagn Invest 31(2):217–221
Pajon R, Yero D, Lage A, Llanes A, Borroto C (2006) Computational identification of beta-barrel outer-membrane proteins in Mycobacterium tuberculosis predicted proteomes as putative vaccine candidates. Tuberculosis 86(3–4):290–302
Singh NK, Goodman A, Walter P, Helms V, Hayat S (1814) 2011 TMBHMM: a frequency profile based HMM for predicting the topology of transmembrane beta barrel proteins and the exposure status of transmembrane residues. Biochim et Biophys Acta 5:664–70
Barker LF, Brennan MJ, Rosenstein PK, Sadoff JC (2009) Tuberculosis vaccine research: the impact of immunology. Curr Opin Immunol 21(3):331–338
Aguilo N, Gonzalo-Asensio J, Alvarez-Arguedas S, Marinova D, Gomez AB, Uranga S et al (2017) Reactogenicity to major tuberculosis antigens absent in BCG is linked to improved protection against Mycobacterium tuberculosis. Nat Commun 8:16085
Okkels LM, Andersen P (2004) Protein-protein interactions of proteins from the ESAT-6 family of Mycobacterium tuberculosis. J Bacteriol 186(8):2487–2491
Lamichhane G, Zignol M, Blades NJ, Geiman DE, Dougherty A, Grosset J et al (2003) A postgenomic method for predicting essential genes at subsaturation levels of mutagenesis: application to Mycobacterium tuberculosis. Proc Natl Acad Sci USA 100(12):7213–7218
Skeiky YA, Ovendale PJ, Jen S, Alderson MR, Dillon DC, Smith S et al (2000) T cell expression cloning of a Mycobacterium tuberculosis gene encoding a protective antigen associated with the early control of infection. J Immunol 165(12):7140–7149
Goldstone RM, Goonesekera SD, Bloom BR, Sampson SL (2009) The transcriptional regulator Rv0485 modulates the expression of a pe and ppe gene pair and is required for Mycobacterium tuberculosis virulence. Infect Immun 77(10):4654–4667
Shah S, Briken V (2016) Modular organization of the ESX-5 secretion system in Mycobacterium tuberculosis. Front Cell Infect Microbiol 6:49
Balaji KN, Goyal G, Narayana Y, Srinivas M, Chaturvedi R, Mohammad S (2007) Apoptosis triggered by Rv1818c, a PE family gene from Mycobacterium tuberculosis is regulated by mitochondrial intermediates in T cells. Microbes Infect 9(3):271–281
Tundup S, Akhter Y, Thiagarajan D, Hasnain SE (2006) Clusters of PE and PPE genes of Mycobacterium tuberculosis are organized in operons: evidence that PE Rv2431c is co-transcribed with PPE Rv2430c and their gene products interact with each other. FEBS Lett 580(5):1285–1293
Worku S, Hoft D (2003) Differential effects of control and antigen-specific T cells on intracellular mycobacterial growth. Infect Immun 71(4):1763–1773
Ramakrishnan L, Federspiel NA, Falkow S (2000) Granuloma-specific expression of Mycobacterium virulence proteins from the glycine-rich PE-PGRS family. Science 288(5470):1436–1439
Basu S, Pathak SK, Banerjee A, Pathak S, Bhattacharyya A, Yang Z et al (2007) Execution of macrophage apoptosis by PE_PGRS33 of Mycobacterium tuberculosis is mediated by Toll-like receptor 2-dependent release of tumor necrosis factor-α. J Biol Chem 282(2):1039–1050
Stamm LM, Morisaki JH, Gao L-Y, Jeng RL, McDonald KL, Roth R et al (2003) Mycobacterium marinum escapes from phagosomes and is propelled by actin-based motility. J Exp Med 198(9):1361–1368
Guirado E, Schlesinger LS, Kaplan G (2013) Macrophages in tuberculosis: friend or foe. Semin Immunopathol 35(5):563–583
Bansal K, Elluru SR, Narayana Y, Chaturvedi R, Patil SA, Kaveri SV et al (2010) PE_PGRS antigens of Mycobacterium tuberculosis induce maturation and activation of human dendritic cells. J Immunol 184(7):3495–3504
Nair S, Ramaswamy PA, Ghosh S, Joshi DC, Pathak N, Siddiqui I et al (2009) The PPE18 of Mycobacterium tuberculosis interacts with TLR2 and activates IL-10 induction in macrophage. J Immunol 183(10):6269–6281
Brosch R, Gordon SV, Marmiesse M, Brodin P, Buchrieser C, Eiglmeier K et al (2002) A new evolutionary scenario for the Mycobacterium tuberculosis complex. Proc Natl Acad Sci USA 99(6):3684–3689
Dillon DC, Alderson MR, Day CH, Lewinsohn DM, Coler R, Bement T et al (1999) Molecular characterization and human t-cell responses to a member of a novel Mycobacterium tuberculosis mtb39Gene family. Infect Immun 67(6):2941–2950
Mahairas GG, Sabo PJ, Hickey MJ, Singh DC, Stover CK (1996) Molecular analysis of genetic differences between Mycobacterium bovis BCG and virulent M. bovis. J Bacteriol 178(5):1274–82
Takatori H, Nakajima H, Hirose K, Kagami S-i, Tamachi T, Suto A et al (2005) Indispensable role of Stat5a in Stat6-independent Th2 cell differentiation and allergic airway inflammation. J Immunol 174(6):3734–40
Manca C, Tsenova L, Freeman S, Barczak AK, Tovey M, Murray PJ et al (2005) Hypervirulent M. tuberculosis W/Beijing strains upregulate type I IFNs and increase expression of negative regulators of the Jak-Stat pathway. J Interferon Cytokine Res 25(11):694–701
Brodin P, Rosenkrands I, Andersen P, Cole ST, Brosch R (2004) ESAT-6 proteins: protective antigens and virulence factors? Trends Microbiol 12(11):500–508
Shi C, Wang X, Zhang H, Xu Z, Li Y, Yuan L (2007) Immune responses and protective efficacy induced by 85B antigen and early secreted antigenic target-6 kDa antigen fusion protein secreted by recombinant bacille Calmette-Guérin. Acta Biochim Biophys Sin 39(4):290–296
Kamath AB, Woodworth J, Xiong X, Taylor C, Weng Y, Behar SM (2004) Cytolytic CD8+ T cells recognizing CFP10 are recruited to the lung after Mycobacterium tuberculosis infection. J Exp Med 200(11):1479–1489
Roupie V, Romano M, Zhang L, Korf H, Lin MY, Franken KL et al (2007) Immunogenicity of eight dormancy regulon-encoded proteins of Mycobacterium tuberculosis in DNA-vaccinated and tuberculosis-infected mice. Infect Immun 75(2):941–949
Yuan W, Dong N, Zhang L, Liu J, Lin S, Xiang Z et al (2012) Immunogenicity and protective efficacy of a tuberculosis DNA vaccine expressing a fusion protein of Ag85B-Esat6-HspX in mice. Vaccine 30(14):2490–2497
Jeon B-Y, Kim S-C, Eum S-Y, Cho S-N (2011) The immunity and protective effects of antigen 85A and heat-shock protein X against progressive tuberculosis. Microbes Infect 13(3):284–290
Romano M, Aryan E, Korf H, Bruffaerts N, Franken C, Ottenhoff T et al (2012) Potential of Mycobacterium tuberculosis resuscitation-promoting factors as antigens in novel tuberculosis sub-unit vaccines. Microbes Infect 14(1):86–95
Shi C, Zhang H, Zhang T, Wang X, Bai B, Zhao Y et al (2009) New alternative vaccine component against Mycobacterium tuberculosis-heat shock protein 16.3 or its T-cell epitope. Scand J Immunol. 70(5):465–474
Shi C, Chen L, Chen Z, Zhang Y, Zhou Z, Lu J et al (2010) Enhanced protection against tuberculosis by vaccination with recombinant BCG over-expressing HspX protein. Vaccine 28(32):5237–5244
De Sousa EM, da Costa AC, Trentini MM, de Araujo Filho JA, Kipnis A, Junqueira-Kipnis AP (2012) Immunogenicity of a fusion protein containing immunodominant epitopes of Ag85C, MPT51, and HspX from Mycobacterium tuberculosis in mice and active TB infection. PLoS ONE 7(10):e47781
Niu H, Hu L, Li Q, Da Z, Wang B, Tang K et al (2011) Construction and evaluation of a multistage Mycobacterium tuberculosis subunit vaccine candidate Mtb10. 4–HspX. Vaccine 29(51):9451–9458
Wieczorek AE, Troudt JL, Knabenbauer P, Taylor J, Pavlicek RL, Karls R et al (2014) HspX vaccination and role in virulence in the guinea pig model of tuberculosis. Pathog Dis 71(3):315–325
Cunningham AF, Spreadbury CL (1998) Mycobacterial stationary phase induced by low oxygen tension: cell wall thickening and localization of the 16-kilodalton α-crystallin homolog. J Bacteriol 180(4):801–808
Cole S, Brosch R, Parkhill J, Garnier T, Churcher C, Harris D et al (1998) Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 396(6707):190
Tyagi AK, Nangpal P, Satchidanandam V (2011) Development of vaccines against tuberculosis. Tuberculosis 91(5):469–478
Maue AC, Waters WR, Palmer MV, Nonnecke BJ, Minion FC, Brown WC et al (2007) An ESAT-6: CFP10 DNA vaccine administered in conjunction with Mycobacterium bovis BCG confers protection to cattle challenged with virulent M. bovis. Vaccine 25(24):4735–46
Dietrich J, Lundberg CV, Andersen P (2006) TB vaccine strategies—what is needed to solve a complex problem? Tuberculosis 86(3–4):163–168
Moradi B, Sankian M, Amini Y, Meshkat Z (2016) Construction of a novel DNA vaccine candidate encoding an HspX-PPE44-EsxV fusion antigen of Mycobacterium tuberculosis. Rep Biochem Mol Biol 4(2):89
Romano M, Rindi L, Korf H, Bonanni D, Adnet P-Y, Jurion F et al (2008) Immunogenicity and protective efficacy of tuberculosis subunit vaccines expressing PPE44 (Rv2770c). Vaccine 26(48):6053–6063
Li Q, Yu H, Zhang Y, Wang B, Jiang W, Da Z et al (2011) Immunogenicity and protective efficacy of a fusion protein vaccine consisting of antigen Ag85B and HspX against Mycobacterium tuberculosis infection in mice. Scand J Immunol 73(6):568–576
Tebianian M, Hoseini AZ, Ebrahimi SM, Memarnejadian A, Mokarram AR, Mahdavi M et al (2011) Cloning, expression, and immunogenicity of novel fusion protein of Mycobacterium tuberculosis based on ESAT-6 and truncated C-terminal fragment of HSP70. Biologicals 39(3):143–148
Zhang H, Peng P, Miao S, Zhao Y, Mao F, Wang L et al (2010) Recombinant Mycobacterium smegmatis expressing an ESAT6-CFP10 fusion protein induces anti-mycobacterial immune responses and protects against Mycobacterium tuberculosis challenge in mice. Scand J Immunol 72(4):349–357
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or nonprofit sectors.
Author information
Authors and Affiliations
Contributions
AV, AAI and AK designed the study. AV, HS, MM and EGM wrote the manuscript. HS and EB revised the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical Approval
This is a review articles and it does not contain any with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valizadeh, A., imani Fooladi, A.A., Sedighian, H. et al. Evaluating the Performance of PPE44, HSPX, ESAT-6 and CFP-10 Factors in Tuberculosis Subunit Vaccines. Curr Microbiol 79, 260 (2022). https://doi.org/10.1007/s00284-022-02949-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00284-022-02949-8