Abstract
Purpose
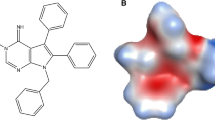
Dasatinib (BMS-354825), a potent oral multi-targeted kinase inhibitor against SRC and BCR-ABL, has recently been approved for the treatment of chronic myelogenous leukaemia (CML) in imatinib-acquired resistance and intolerance. In vitro and in vivo studies were conducted to characterize the pharmacokinetics and metabolism of dasatinib in mouse, rat, dog, and monkey. Possible mechanisms contributing to the incomplete oral bioavailability of dasatinib in animals were investigated.
Methods
Metabolic stability of dasatinib was measured after incubation with liver microsomes (either NADPH- or UDPGA-fortified) and isolated hepatocytes obtained from mouse, rat, dog, monkey, and human. In all cases, substrate depletion over time was measured, and appropriate scaling factors were used to predict in vivo clearance. Pharmacokinetics of dasatinib were determined in mice, rats, dogs, and monkeys after administration of single intravenous or oral doses. In addition, the routes of excretion were investigated after administration of dasatinib to bile duct cannulated (BDC) rats. Absorption and first-pass metabolism were evaluated as possible reasons for the incomplete oral bioavailability using various in vitro and in vivo models like Caco-2 cells, P-glycoprotein (P-gp) knockout mice, and intra-portal dosing in rats.
Results
In vivo systemic plasma clearance values of dasatinib were 62, 26, 25, and 34 ml/min/kg in mouse, rat, dog, and monkey, respectively. Scaling of in vitro hepatocyte and liver microsomal data gave reasonably good predictions of in vivo clearances across all species. Percent distribution in blood cells ranged from 43% in mouse to 57% in dog. Dasatinib showed high volumes of distribution (>3 l/kg) and high serum protein binding values (>90%) in all four species tested. Oral bioavailability of dasatinib ranged from 14% in the mouse to 34% in the dog. In rats, bioavailability after an intraportal dose was comparable to that after intra-arterial administration. In BDC rats, less than 15% of an intravenous dose was excreted unchanged in urine, bile, and the gastrointestinal tract, suggesting that dasatinib is cleared primarily via metabolism. Dasatinib has high intrinsic permeability in Caco-2 cells, however, the efflux ratio was approximately two-fold indicating that it may be a substrate for an intestinal efflux transporter. However, in vivo studies in P-gp knockout mice versus wild-type mice showed no difference in the amount of dasatinib remaining unabsorbed in the gastrointestinal tract, suggesting that P-gp may not be responsible for the incomplete bioavailability.
Conclusions
Dasatinib shows intermediate clearance in mouse, rat, dog, and monkey, and distributes extensively in those species. Oxidative metabolism appears to be the predominant clearance pathway. The incomplete oral bioavailability may be due to both incomplete absorption and high first-pass metabolism. However, the efflux transporter, P-glycoprotein does not appear to be limiting oral absorption.






Similar content being viewed by others
References
Sawyers CL (1999) Chronic myeloid leukemia. N Engl J Med 340:1330–1340
Daley GQ, Van Etten RA, Baltimore D (1990) Induction of chromic myelogenous leukaemia in mice by the P210 bcr/abl gene of the Philadelphia chromosome. Science 247:824–830
Drucker BJ, Talpaz M, Resta DJ et al (2001) Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med 344:1031–1037
Gorre ME, Mohammed M, Ellwood K et al (2004) Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplication. Science 293:876–880
Lombardo LJ, Lee FY, Chen P et al (2004) Discovery of N-(2-chloro-6-methyl- phenyl)-2-(6-(4-(2-hydroxyethyl)-piperazin-1-yl)-2-methylpyrimidin-4-ylamino) thiazole -5-carboxamide (BMS-354825), a dual Src/Abl kinase inhibitor with potent antitumor activity in preclinical assays. J Med Chem 47:6658–6661
Tokarski JS, Newitt JA, Chang CYJ et al (2006) The structure of dasatinib (BMS-354825) bound to activated ABL kinase domain elucidates its inhibitory activity against imatinib-resistant ABL mutants. Cancer Res 66:5790–5797
Shah NP, Tran C, Lee FY, Chen P, Norris D, Sawyers C (2004) Overriding imatinib resistance with a novel ABL kinase inhibitor. Science 305:399–401
Talpaz M, Shah NP, Kantarjian H et al (2006) Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med 354:2531–2541
Frame MC (2002) Src in cancer: deregulation and consequences for cell behaviour. Biochim Biophys Acta 1602:114–130
Berry MN, Edwards AM, Barritt GJ (1991) Isolated hepatocytes preparation, properties and applications in laboratory techniques in biochemistry and molecular biology. Elsevier, Amsterdam
Gibaldi M, Perrier D (1982) (eds) Pharmacokinetics, 2nd edn. Marcel-Dekker, New York
Boxenbaum H (1982) Interspecies scaling, allometry, physiological time, and the ground plan of pharmacokinetics. J Pharmacokinet Biopharm 10:201–227
Mordenti J, Chappell W (1989) The use of interspecies scaling in toxicokinetics. In: Avram Y, Skelley J, Batra VK (eds) Toxicokinetics and drug development. Pergamon, New York
Houston JB, Carlile DJ (1997) Prediction of hepatic clearance from microsomes, hepatocytes, and liver slices. Drug Metab Rev 29:891–922
Davies B, Morris T (1993) Physiological parameters in laboratory animals and humans. Pharm Res 10:1093–1095
Luo FR, Yang Z, Camuso A, Smykla R, McGlinchey K, Fager K, Flefleh C, Castaneda S, Inigo I, Kan D, Wen ML, Kramer R, Blackwood-Chirchir A, Lee FY (2006) Dasatinib (BMS-354825) pharmacokinetics and pharmacodynamic biomarkers in animal models predict optimal clinical exposure. Clin Cancer Res 12:7180–86
Tanigawara Y (2000) Role of P-glycoprotein in drug disposition. Ther Drug Monit 22:137–140
Acknowledgments
The assistance of the Technical Support Unit in animal maintenance, dosing, and sample collection, Christian Caporuscio, Bogdan Sleczka, and Georgia Cornelius in LC/MS/MS analysis, and the MAP Knowledge Centers in conducting some of the in vitro experiments is greatly appreciated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kamath, A.V., Wang, J., Lee, F.Y. et al. Preclinical pharmacokinetics and in vitro metabolism of dasatinib (BMS-354825): a potent oral multi-targeted kinase inhibitor against SRC and BCR-ABL. Cancer Chemother Pharmacol 61, 365–376 (2008). https://doi.org/10.1007/s00280-007-0478-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-007-0478-8