Abstract
Purpose
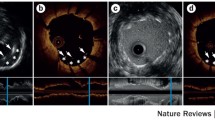
The implantation of flow diverters requires administration of dual anti-platelet therapy, posing the potential for complications. The p48MW HPC (phenox, Bochüm, Germany) hydrophilic-coated flow diverting stent is designed to be anti-thrombotic, thus opening the potential for single anti-platelet therapy. We deploy a novel intravascular high-resolution imaging technique, high-frequency optical coherence tomography (HF-OCT), to study in an animal model the acute thrombus formation on coated p48MW devices versus uncoated control devices.
Methods
Three pigs were implanted with 4 flow diverters each, two test hydrophilic-coated devices, and two control uncoated devices (p48MW). Each pig was treated with a different anti-platelet regime: no anti-platelet therapy, aspirin only, aspirin and clopidogrel. Twenty minutes after the flow diverter was implanted, an HF-OCT data set was acquired. Acute clot formed on the flow diverter at each covered side branch was measured from the HF-OCT slices. Factors considered to be important were the device type (pHPC versus bare metal), aspirin, clopidogrel, and vessel location. A linear model was constructed from the significant factors.
Results
Both coating (p < 0.001) and aspirin (p = 0.003) were significantly related to reduction in clot burden, leading to an approximate 100-fold and 50-fold reduction in clot, respectively.
Conclusions
This study shows the power of HF-OCT not only in the detection of clot but also the quantification of clot burden. In an animal model, the pHPC-coated p48MW significantly reduced acute thrombus formation over jailed side branches as compared to the bare metal p48MW that was nearly eliminated when combined with aspirin administration.


Similar content being viewed by others
Notes
The anesthesiological protocol can be found in the online supplement of the article.
References
Lylyk P, et al. Endovascular reconstruction of intracranial arteries by stent placement and combined techniques. J Neurosurg. 2002;97(6):1306–13.
Piotin M, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010;41(1):110–5.
Wakhloo AK, et al. Closed-cell stent for coil embolization of intracranial aneurysms: clinical and angiographic results. AJNR Am J Neuroradiol. 2012;33(9):1651–6.
Becske T, et al. Long-term clinical and angiographic outcomes following pipeline embolization device treatment of complex internal carotid artery aneurysms: five-year results of the pipeline for uncoilable or failed aneurysms trial. Neurosurgery. 2017;80(1):40–8.
Adeeb N, et al. Use of platelet function testing before pipeline embolization device placement: a multicenter cohort study. Stroke. 2017;48(5):1322–30.
Podlasek A, et al. Outcome of intracranial flow diversion according to the antiplatelet regimen used: a systematic review and meta-analysis. J Neurointerv Surg. 2020;12(2):148–55.
Kan P, et al. Expanding indications for flow diverters: ruptured aneurysms, blister aneurysms, and dissecting aneurysms. Neurosurgery. 2020;86(Supplement_1):S96–S103.
Cutlip DE, et al. Thrombotic complications associated with early and late nonadherence to dual antiplatelet therapy. JACC Cardiovasc Interv. 2015;8(3):404–10.
Rajah G, Narayanan S, Rangel-Castilla L. Update on flow diverters for the endovascular management of cerebral aneurysms. Neurosurg Focus. 2017;42(6):E2.
Shapiro M, et al. Stent-supported aneurysm coiling: a literature survey of treatment and follow-up. AJNR Am J Neuroradiol. 2012;33(1):159–63.
Daou B, et al. P2Y12 reaction units: effect on hemorrhagic and thromboembolic complications in patients with cerebral aneurysms treated with the pipeline embolization device. Neurosurgery. 2016;78(1):27–33.
Sousa JE, et al. Sirolimus-eluting stent for the treatment of in-stent restenosis: a quantitative coronary angiography and three-dimensional intravascular ultrasound study. Circulation. 2003;107(1):24–7.
Sousa JE, et al. Two-year angiographic and intravascular ultrasound follow-up after implantation of sirolimus-eluting stents in human coronary arteries. Circulation. 2003;107(3):381–3.
Sousa JE, et al. Use of rapamycin-impregnated stents in coronary arteries. Transplant Proc. 2003;35(3 Suppl):165S–70S.
Dola J, et al. Results of PCI with drug-eluting stents in an all-comer population depending on vessel diameter. J Clin Med. 2020;9(2):524.
Youn YJ, et al. Randomized comparison of everolimus- and zotarolimus-eluting coronary stents with biolimus-eluting stents in all-comer patients. Circ Cardiovasc Interv. 2020;13(3):e008525.
Pasarikovski CR, et al. Pipeline embolisation device with shield technology for the treatment of ruptured intracranial aneurysm. Neuroradiol J. 2019;32(3):189–92.
Trivelato FP, et al. Safety and effectiveness of the pipeline flex embolization device with shield technology for the treatment of intracranial aneurysms: midterm results from a multicenter study. Neurosurgery. 2019. https://doi.org/10.1093/neuros/nyz356.
Marosfoi M, et al. Acute thrombus formation on phosphorilcholine surface modified flow diverters. J Neurointerv Surg. 2018;10(4):406–11.
Matsuda Y, et al. Preliminary outcomes of single antiplatelet therapy for surface-modified flow diverters in an animal model: analysis of neointimal development and thrombus formation using OCT. J Neurointerv Surg. 2019;11(1):74–9.
King RM, et al. Communicating malapposition of flow diverters assessed with optical coherence tomography correlates with delayed aneurysm occlusion. J Neurointerv Surg. 2018;10(7):693–7.
Gounis MJ, et al. Intravascular optical coherence tomography for neurointerventional surgery. Stroke, 2018: p. STROKEAHA118022315.
Lenz-Habijan T, et al. Hydrophilic stent coating inhibits platelet adhesion on stent surfaces: initial results in vitro. Cardiovasc Intervent Radiol. 2018;41(11):1779–855.
Bhatt DL, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354(16):1706–17.
Donadini MP, Bellesini M, Squizzato A. Aspirin plus clopidogrel vs aspirin alone for preventing cardiovascular events among patients at high risk for cardiovascular events. JAMA. 2018;320(6):593–4.
Martinez Moreno R, et al. In vivo canine study of three different coatings applied to p64 flow-diverter stents: initial biocompatibility study. Eur Radiol Exp. 2019;3(1):3.
Funding
This study was funded by phenox and the Massachusetts Life Sciences Center Bits-to-Bytes program.
Author information
Authors and Affiliations
Contributions
RMK performed the experiments, analyzed and interpreted the data, wrote the manuscript, and approved the final manuscript. ETL performed the experiments, analyzed the data, and approved the final manuscript. CMR performed the experiments and approved the final manuscript. GJU performed the experiments, interpreted the data, revised the manuscript, and approved the final manuscript. HH designed the study, revised the manuscript, and approved the final manuscript. ASP designed the study, revised the manuscript, and approved the final manuscript. MJG designed the study, designed and performed the experiments, analyzed and interpreted the data, drafted the manuscript, approved the final manuscript, and agrees to be accountable for the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Conflict of interest
Robert M. King, Erin T. Langan, Chris M. Raskett declare that they have no conflicts of interest. Giovanni J. Ughi declares he is an employee of Gentuity LLC and holds stock. Hans Henkes declares he is a founder of phenox GmbH. Ajit S. Puri declares he has been a consultant for Stryker, Cerenovus, Medtronic, Cerevasc, and Microvention; holds stock in InNeuroCo; and has received research support from National Institutes of Health (NIH). Matthew J. Gounis declares he has been a consultant on a fee-per-hour basis for Cerenovus, Imperative Care, phenox, Medtronic Neurovascular, Route 92 Medical, Stryker Neurovascular; holds stock in Imperative Care and Neurogami; and has received research support from the National Institutes of Health (NIH), the United States – Israel Binational Science Foundation, Anaconda, ApicBio, Axovant, Cerenovus, Cook Medical, Gentuity, Imperative Care, InNeuroCo, Magneto, MicroVention, Medtronic Neurovascular, MIVI Neurosciences, Neuravi, Neurogami, Philips Healthcare, Rapid Medical, Route 92 Medical, Stryker Neurovascular, Syntheon, and the Wyss Institute.
Ethical Approval
All procedures performed in this study were in accordance with ethical standards of the Institutional Animal Care and Use Committee (IACUC).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
King, R.M., Langan, E.T., Ughi, G.J. et al. Acute Thrombus Burden on Coated Flow Diverters Assessed by High Frequency Optical Coherence Tomography. Cardiovasc Intervent Radiol 43, 1218–1223 (2020). https://doi.org/10.1007/s00270-020-02482-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02482-w