Abstract
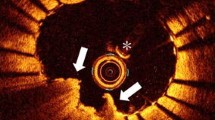
Optical coherence tomography (OCT) is able to identify thrombus. We detect the frequency of thrombus inside the guiding catheter by OCT and its relationship with clinical and procedural factors. We screened 77 patients who underwent OCT pullbacks. Only patients with visible guiding catheter were finally included (35) and divided into thrombus (21) or no-thrombus group (14). Patients within thrombus group were mostly males (100 vs. 71 %, p = 0.05), with acute coronary syndrome (76 vs. 36 %, p = 0.02) and received more frequently percutaneous coronary intervention (86 vs. 43 %, p = 0.01) as compared to other group. A second dose of heparin was more frequently administered in thrombus than in other group (86 vs. 50 %, p = 0.01). Time between first heparin administration and OCT pullback (41[28–57] vs. 20 min [10–32], p = 0.001), time elapsed from second heparin administration and OCT pullback (29 [19–48] vs. 16 min [12–22], p = 0.002) and total procedural time (47 [36–69] vs. 31 min [26–39], p = 0.005) were longer in thrombus compared to other group. At multivariate analysis, total procedural time and time between first heparin administration and OCT pullback were only predictors of intra-catheter thrombus (HR 0.6 [0.3–0.9], p = 0.03 and HR 1.9 [1.1–3.2], p = 0.02, respectively). Thrombus inside guiding catheter may be a frequent finding in long interventional procedure. Future studies are warranted to determine its clinical impact.



Similar content being viewed by others
References
Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, Hee MR, Flotte T, Gregory K, Puliafito CA (1991) Optical coherence tomography. Science 254:1178–1181
Bezerra HG, Costa MA, Guagliumi G, Rollins AM, Simon DI (2009) Intracoronary optical coherence tomography: a comprehensive review clinical and research applications. JACC Cardiovasc Interv 2:1035–1046
Kubo T, Akasaka T (2010) Optical coherence tomography imaging: current status and future perspectives : current and future developments in OCT. Cardiovasc Interv Ther 25:2–10
Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, Bouma B, Bruining N, Cho JM, Chowdhary S, Costa MA, de Silva R, Dijkstra J, Di Mario C, Dudek D, Falk E, Feldman MD, Fitzgerald P, Garcia-Garcia HM, Gonzalo N, Granada JF, Guagliumi G, Holm NR, Honda Y, Ikeno F, Kawasaki M, Kochman J, Koltowski L, Kubo T, Kume T, Kyono H, Lam CC, Lamouche G, Lee DP, Leon MB, Maehara A, Manfrini O, Mintz GS, Mizuno K, Morel MA, Nadkarni S, Okura H, Otake H, Pietrasik A, Prati F, Räber L, Radu MD, Rieber J, Riga M, Rollins A, Rosenberg M, Sirbu V, Serruys PW, Shimada K, Shinke T, Shite J, Siegel E, Sonoda S, Suter M, Takarada S, Tanaka A, Terashima M, Thim T, Uemura S, Ughi GJ, van Beusekom HM, van der Steen AF, van Es GA, van Soest G, Virmani R, Waxman S, Weissman NJ, Weisz G, International Working Group for Intravascular Optical Coherence Tomography (IWG-IVOCT) (2012) Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies. J Am Coll Cardiol 59:1058–1072
Jang IK, Tearney GJ, MacNeill B, Takano M, Moselewski F, Iftima N, Shishkov M, Houser S, Aretz HT, Halpern EF, Bouma BE (2005) In vivo characterization of coronary atherosclerotic plaque by use of optical coherence tomography. Circulation 111:1551–1555
Gonzalo N, Serruys PW, Barlis P, Ligthart J, Garcia-Garcia HM, Regar E (2010) Multi-modality intra-coronary plaque characterization: a pilot study. Int J Cardiol 138:32–39
Motoyama S, Sarai M, Harigaya H, Anno H, Inoue K, Hara T, Naruse H, Ishii J, Hishida H, Wong ND, Virmani R, Kondo T, Ozaki Y, Narula J (2009) Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol 54:49–57
Kubo T, Imanishi T, Takarada S, Kuroi A, Ueno S, Yamano T, Tanimoto T, Matsuo Y, Masho T, Kitabata H, Tsuda K, Tomobuchi Y, Akasaka T (2007) Assessment of culprit lesion morphology in acute myocardial infarction: ability of optical coherence tomography compared with intravascular ultrasound and coronary angioscopy. J Am Coll Cardiol 50:933–939
Ozaki Y, Okumura M, Ismail TF, Motoyama S, Naruse H, Hattori K, Kawai H, Sarai M, Takagi Y, Ishii J, Anno H, Virmani R, Serruys PW, Narula J (2011) Coronary CT angiographic characteristics of culprit lesions in acute coronary syndromes not related to plaque rupture as defined by optical coherence tomography and angioscopy. Eur Heart J 32:2814–2823
Eeckhout E, Serruys PW, Wijns W, Vahanian A, van Sambeek M, De Palma R (eds) (2012) PCR–EAPCI textbook of percutaneous interventional cardiovascular medicine. Europa Publications, London
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46
Vetrovec GW, Cowley MJ, Overton H, Richardson DW (1981) Intracoronary thrombus in syndromes of unstable myocardial ischemia. Am Heart J 102:1202–1208
Holmes DR Jr, Hartzler GO, Smith HC, Fuster V (1981) Coronary artery thrombosis in patients with unstable angina. Br Heart J 45:411–416
Ellis SG, Roubin GS, King SB, Douglas JS Jr, Weintraub WS, Thomas RG, Cox WR (1988) Angiographic and clinical predictors of acute closure after native vessel coronary angioplasty. Circulation 77:372–379
Singh M, Reeder GS, Ohman EM, Mathew V, Hillegass WB, Anderson RD, Gallup DS, Garratt KN, Holmes DR Jr (2001) Does the presence of thrombus seen on a coronary angiogram affect the outcome after percutaneous coronary angioplasty? An Angiographic Trials Pool data experience. J Am Coll Cardiol 38:624–630
Kirtane AJ, Sandhu P, Mehran R, McEntegart M, Cristea E, Brener SJ, Xu K, Fahy M, Généreux P, Wessler JD, Stone GW (2014) Association between intraprocedural thrombotic events and adverse outcomes after primary percutaneous coronary intervention for st-segment elevation myocardial infarction (a harmonizing outcomes with revascularization and stents in acute myocardial infarction [HORIZONS-AMI] substudy). Am J Cardiol 113:36–43
McEntegart MB, Kirtane AJ, Cristea E, Brener S, Mehran R, Fahy M, Moses JW, Stone GW (2012) Intraprocedural thrombotic events during percutaneous coronary intervention in patients with non-ST-segment elevation acute coronary syndromes are associated with adverse outcomes: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol 59:1745–1751
Otake H, Shite J, Ako J, Hinke T, Tanino Y, Ogasawara D, Sawada T, Miyoshi N, Kato H, Koo BK, Honda Y, Fitzgerald PJ, Hirata K (2012) Local determinants of thrombus formation following sirolimus-eluting stent implantation assessed by optical coherence tomography. JACC Cardiovasc Interv 2:459–466
Awata M, Kotani J, Uematsu M, Morozumi T, Watanabe T, Onishi T, Iida O, Sera F, Nanto S, Hori M, Nagata S (2007) Serial angioscopic evidence of incomplete neointimal coverage after sirolimus-eluting stent implantation: comparison with bare-metal stents. Circulation 116:910–916
Kotani J, Awata M, Nanto S, Uematsu M, Oshima F, Minamiguchi H, Mintz GS, Nagata S (2006) Incomplete neointimal coverage of sirolimus-eluting stents: angioscopic findings. J Am Coll Cardiol 47:2108–2111
Takano M, Ohba T, Inami S, Seimiya K, Sakai S, Mizuno K (2006) Angioscopic differences in neointimal coverage and in persistence of thrombus between sirolimus-eluting stents and bare metal stents after a 6-month implantation. Eur Heart J 27:2189–2195
Howe Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators, Yusuf S, Mehta SR, Chrolavicius S, Afzal R, Pogue J, Granger CB, Budaj A, Peters RJ, Bassand JP, Wallentin L, Joyner C, Fox KA (2006) Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med 354:1464–1476
Waksman R, Bertrand O, Driesman M, Gruberg L, Rossi J, Mehta S, Swymelar S, Dvir D, Xue Z, Torguson R (2013) Bivalirudin versus unfractionated heparin during percutaneous coronary intervention in patients with non-ST-segment elevation acute coronary syndrome initially treated with fondaparinux: results from an international, multicenter, randomized pilot study (SWITCH III). J Interv Cardiol 26:107–113
Spaulding C, Lefevre T, Funck F, Thébault B, Chauveau M, Ben Hamda K, Chalet Y, Monségu H, Tsocanakis O, Py A, Guillard N, Weber S (1996) Left radial approach for coronary angiography: results of a prospective study. Cathet Cardiovasc Diagn 39:365–370
Bernat I, Bertrand OF, Rokyta R, Kacer M, Pesek J, Koza J, Smid M, Bruhova H, Sterbakova G, Stepankova L, Costerousse O (2011) Efficacy and safety of transient ulnar artery compression to recanalize acute radial artery occlusion after transradial catheterization. Am J Cardiol 107:1698–1701
Cavusoglu E, Lakhani M, Marmur JD (2005) The activated clotting time (ACT) can be used to monitor enoxaparin and dalteparin after intravenous administration. J Invasive Cardiol 17:416–421
De Swart CA, Nijmeyer B, Roelofs JM, Sixma JJ (1982) Kinetics of intravenously administered heparin in normal humans. Blood 60:1251–1258
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The authors state that this study have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scalone, G., Brugaletta, S., Garcia-Garcia, H.M. et al. Frequency and predictors of thrombus inside the guiding catheter during interventional procedures: an optical coherence tomography study. Int J Cardiovasc Imaging 31, 239–246 (2015). https://doi.org/10.1007/s10554-014-0544-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-014-0544-3