Abstract
Background
For patients undergoing abdominal surgery, multimodal prehabilitation, including nutrition and exercise interventions, aims to optimize their preoperative physical and physiological capacity. This meta-analysis aims to explore the impact of multimodal prehabilitation on surgical and functional outcomes of abdominal surgery.
Methods
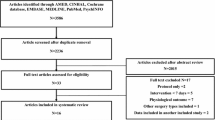
Medline, Embase and CENTRAL were searched for articles about multimodal prehabilitation in major abdominal surgery. Primary outcomes were postoperative complications with a Clavien–Dindo score ≥3, and functional outcomes, measured by the 6-Minute Walking Test (6MWT). Secondary outcome measures included the quality-of-life measures. Pooled risk ratio (RR) and 95% confidence interval (CI) were estimated, with DerSimonian and Laird random effects used to account for heterogeneity.
Results
Twenty-five studies were included, analysing 4,210 patients across 13 trials and 12 observational studies. Patients undergoing prehabilitation had significantly fewer overall complications (RR = 0.879, 95% CI 0.781–0.989, p = 0.034). There were no significant differences in the rates of wound infection, anastomotic leak and duration of hospitalization. The 6MWT improved preoperatively in patients undergoing prehabilitation (SMD = 33.174, 95% CI 12.674–53.673, p = 0.005), but there were no significant differences in the 6MWT at 4 weeks (SMD = 30.342, 95% CI − 2.707–63.391, p = 0.066) and 8 weeks (SMD = 24.563, 95% CI − 6.77–55.900, p = 0.104) postoperatively.
Conclusions
As preoperative patient optimization shifts towards an interdisciplinary approach, evidence from this meta-analysis shows that multimodal prehabilitation improves the preoperative functional capacity and reduces postoperative complication rates, suggesting its potential in effectively optimizing the abdominal surgery patient. However, there is a large degree of heterogenicity between the prehabilitation interventions between included articles; hence results should be interpreted with caution.




Similar content being viewed by others
References
Kirchhoff P, Clavien PA, Hahnloser D (2010) Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg 4(1):5. https://doi.org/10.1186/1754-9493-4-5
Ahmad T, Bouwman RA, Grigoras I, Aldecoa C, Hofer C, Hoeft A, do Nascimento Jr. P (2016) Global patient outcomes after elective surgery: prospective cohort study in 27 low-, middle- and high-income countries. Br J Anaesth 117(5):601–609. https://doi.org/10.1093/bja/aew316
Hewitt J, Long S, Carter B, Bach S, McCarthy K, Clegg A (2018) The prevalence of frailty and its association with clinical outcomes in general surgery: a systematic review and meta-analysis. Age Ageing 47(6):793–800. https://doi.org/10.1093/ageing/afy110
Gillick MR, Serrell NA, Gillick LS (1982) Adverse consequences of hospitalization in the elderly. Soc Sci Med 16(10):1033–1038. https://doi.org/10.1016/0277-9536(82)90175-7
Hanna K, Ditillo M, Joseph B (2019) The role of frailty and prehabilitation in surgery. Curr Opin Crit Care 25(6):717–722. https://doi.org/10.1097/mcc.0000000000000669
Norris CM, Close JCT (2020) Prehabilitation for the frailty syndrome: improving outcomes for our most vulnerable patients. Anesth Analg 130(6):1524–1533
Le Roy B, Selvy M, Slim K (2016) The concept of prehabilitation: What the surgeon needs to know? J Visc Surg 153(2):109–112. https://doi.org/10.1016/j.jviscsurg.2016.01.001
Warps AK, de Neree tot Babberich MPM, Dekker E, Wouters MWJM, Dekker JWT, Tollenaar RAEM et al (2021) Interhospital referral of colorectal cancer patients: a dutch population-based study. Int J Colorectal Dis 36(7):1443–1453. https://doi.org/10.1007/s00384-021-03881-2
Wang Y, Liu Z, Shan F, Ying X, Zhang Y, Li S et al (2020) Optimal timing to surgery after neoadjuvant chemotherapy for locally advanced gastric cancer. Front 10:613988. https://doi.org/10.3389/fonc.2020.613988
Banugo P, Amoako D (2017) Prehabilitation. BJA Educ 17(12):401–405. https://doi.org/10.1093/bjaed/mkx032
Daniels SL, Lee MJ, George J, Kerr K, Moug S, Wilson TR et al (2020) Prehabilitation in elective abdominal cancer surgery in older patients: systematic review and meta-analysis. BJS Open. https://doi.org/10.1002/bjs5.50347
Lambert J, Hayes L, Keegan T, Subar D, Gaffney C (2020) The impact of prehabilitation on patient outcomes in hepatobiliary, colorectal, and upper gastrointestinal cancer surgery: a PRISMA-accordant meta-analysis. Ann Surg. https://doi.org/10.1097/SLA.0000000000004527
Hughes MJ, Hackney RJ, Lamb PJ, Wigmore SJ, Christopher Deans DA, Skipworth RJE (2019) Prehabilitation before major abdominal surgery: a systematic review and meta-analysis. World J Surg 43(7):1661–1668. https://doi.org/10.1007/s00268-019-04950-y
Bruns ERJ, Argillander TE, Van Den Heuvel B, Buskens CJ, Van Duijvendijk P, Winkels RM et al (2018) Oral nutrition as a form of pre-operative enhancement in patients undergoing surgery for colorectal cancer: a systematic review. Surg Infect (Larchmt) 19(1):1–10. https://doi.org/10.1089/sur.2017.143
Carli F, Brown R, Kennepohl S (2012) Prehabilitation to enhance postoperative recovery for an octogenarian following robotic-assisted hysterectomy with endometrial cancer. Can J Anesth 59(8):779–784. https://doi.org/10.1007/s12630-012-9734-4
Carli F, Silver JK, Feldman LS, McKee A, Gilman S, Gillis C et al (2017) Surgical prehabilitation in patients with cancer: state-of-the-science and recommendations for future research from a panel of subject matter experts. Phys Med Rehabil Clin N Am 28(1):49–64. https://doi.org/10.1016/j.pmr.2016.09.002
Moyer R, Ikert K, Long K, Marsh J (2017) The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: a systematic review and meta-analysis. JBJS Rev 5(12):e2. https://doi.org/10.2106/jbjs.Rvw.17.00015
Marmelo F, Rocha V, Moreira-Gonçalves D (2018) The impact of prehabilitation on post-surgical complications in patients undergoing non-urgent cardiovascular surgical intervention: systematic review and meta-analysis. Eur J Prev Cardiol 25(4):404–417. https://doi.org/10.1177/2047487317752373
Wang L, Lee M, Zhang Z, Moodie J, Cheng D, Martin J (2016) Does preoperative rehabilitation for patients planning to undergo joint replacement surgery improve outcomes? A systematic review and meta-analysis of randomised controlled trials. BMJ Open 6(2):e009857. https://doi.org/10.1136/bmjopen-2015-009857
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14(1):135. https://doi.org/10.1186/1471-2288-14-135
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5(1):13. https://doi.org/10.1186/1471-2288-5-13
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Pecorelli N, Fiore JF Jr, Gillis C, Awasthi R, Mappin-Kasirer B, Niculiseanu P et al (2016) The six-minute walk test as a measure of postoperative recovery after colorectal resection: further examination of its measurement properties. Surg Endosc 30(6):2199–2206. https://doi.org/10.1007/s00464-015-4478-1
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Wells G, Shea B, O'connell DL, Peterson J, Welch, Losos M, et al. (2014) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses
McGuinness LA, Higgins JPT (2021) Risk-of-bias visualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 12(1):55–61. https://doi.org/10.1002/jrsm.1411
Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A et al (2014) Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 121(5):937–947. https://doi.org/10.1097/ALN.0000000000000393
Minnella EM, Bousquet-Dion G, Awasthi R, Scheede-Bergdahl C, Carli F (2017) Multimodal prehabilitation improves functional capacity before and after colorectal surgery for cancer: a five-year research experience. Acta Oncol 56(2):295–300. https://doi.org/10.1080/0284186X.2016.1268268
Bousquet-Dion G, Awasthi R, Loiselle S, Minnella EM, Agnihotram RV, Bergdahl A et al (2018) Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta oncologica (Stockholm, Sweden) 57(6):849–859. https://doi.org/10.1080/0284186X.2017.1423180
Minnella EM, Awasthi R, Bousquet-Dion G, Ferreira V, Austin B, Audi C et al (2019) Multimodal prehabilitation to enhance functional capacity following radical cystectomy: a randomized controlled trial. Eur Urol Focus. https://doi.org/10.1016/j.euf.2019.05.016
Carli F, Bousquet-Dion G, Awasthi R, Elsherbini N, Liberman S, Boutros M et al (2020) Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: a randomized clinical trial. JAMA Surg 155(3):233–242. https://doi.org/10.1001/jamasurg.2019.5474
Minnella EM, Ferreira V, Awasthi R, Charlebois P, Stein B, Liberman AS et al (2020) Effect of two different pre-operative exercise training regimens before colorectal surgery on functional capacity: a randomised controlled trial. Eur J Anaesthesiol 37(11):969–978. https://doi.org/10.1097/EJA.0000000000001215
Barberan-Garcia A, Ubré M, Roca J, Lacy AM, Burgos F, Risco R et al (2018) Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg 267(1):50–56. https://doi.org/10.1097/SLA.0000000000002293
Ausania F, Senra P, Meléndez R, Caballeiro R, Ouviña R, Casal-Núñez E (2019) Prehabilitation in patients undergoing pancreaticoduodenectomy: a randomized controlled trial. Revista espanola de enfermedades digestivas: organo oficial de la Sociedad Espanola de Patologia Digestiva 111(8):603–608. https://doi.org/10.17235/reed.2019.6182/2019
Mora López L, Pallisera Llovera A, Serra-Aracil X, Serra Pla S, Lucas Guerrero V, Rebasa P et al (2020) A single-center prospective observational study on the effect of trimodal prehabilitation in colorectal surgery. Cirugia espanola 98(10):605–611. https://doi.org/10.1016/j.ciresp.2020.03.023
Lopez-Rodriguez-Arias F, Sanchez-Guillen L, Aranaz-Ostariz V, Triguero-Canovas D, Lario-Perez S, Barber-Valles X et al (2021) Effect of home-based prehabilitation in an enhanced recovery after surgery program for patients undergoing colorectal cancer surgery during the COVID-19 pandemic. Support Care Cancer 29(12):7785–7791. https://doi.org/10.1007/s00520-021-06343-1
Souwer ETD, Bastiaannet E, de Bruijn S, Breugom AJ, van den Bos F, Portielje JEA et al (2018) Comprehensive multidisciplinary care program for elderly colorectal cancer patients: “From prehabilitation to independence.” Eur J Surg Oncol 44(12):1894–1900. https://doi.org/10.1016/j.ejso.2018.08.028
Janssen TL, Steyerberg EW, Langenberg JCM, de Lepper C, Wielders D, Seerden TCJ et al (2019) Multimodal prehabilitation to reduce the incidence of delirium and other adverse events in elderly patients undergoing elective major abdominal surgery: an uncontrolled before-and-after study. PLoS ONE [Electronic Resource] 14(6):e0218152. https://doi.org/10.1371/journal.pone.0218152
van Rooijen SJ, Molenaar CJL, Schep G, van Lieshout R, Beijer S, Dubbers R et al (2019) Making patients fit for surgery: introducing a four pillar multimodal prehabilitation program in colorectal cancer. Am J Phys Med Rehabil 98(10):888–896. https://doi.org/10.1097/PHM.0000000000001221
Chia CL, Mantoo SK, Tan KY (2016) “Start to finish trans-institutional transdisciplinary care”: a novel approach improves colorectal surgical results in frail elderly patients. Colorectal Dis 18(1):O43-50. https://doi.org/10.1111/codi.13166
Wang B, Shelat VG, Chow JJL, Huey TCW, Low JK, Woon WWL et al (2020) Prehabilitation program improves outcomes of patients undergoing elective liver resection. J Surg Res 251:119–125. https://doi.org/10.1016/j.jss.2020.01.009
Koh FH, Loh CH, Tan WJ, Ho LML, Yen D, Chua JMW et al (2021) Structured presurgery prehabilitation for aged patients undergoing elective surgery significantly improves surgical outcomes and reduces cost: a nonrandomized sequential comparative prospective cohort study. Nutr Clin Pract 03:03. https://doi.org/10.1002/ncp.10787
Pang NQ, Tan YX, Samuel M, Tan KK, Bonney GK, Yi H et al (2022) Multimodal prehabilitation in older adults before major abdominal surgery: a systematic review and meta-analysis. Langenbecks Arch Surg 02:02. https://doi.org/10.1007/s00423-022-02479-8
Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS et al (2013) Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc 27(4):1072–1082. https://doi.org/10.1007/s00464-012-2560-5
Howard R, Yin YS, McCandless L, Wang S, Englesbe M, Machado-Aranda D (2019) Taking control of your surgery: impact of a prehabilitation program on major abdominal surgery. J Am Coll Surg 228(1):72–80. https://doi.org/10.1016/j.jamcollsurg.2018.09.018
Kaibori M, Ishizaki M, Matsui K, Nakatake R, Yoshiuchi S, Kimura Y et al (2013) Perioperative exercise for chronic liver injury patients with hepatocellular carcinoma undergoing hepatectomy. Am J Surg 206(2):202–209. https://doi.org/10.1016/j.amjsurg.2012.07.035
Nakajima H, Yokoyama Y, Inoue T, Nagaya M, Mizuno Y, Kadono I et al (2019) Clinical benefit of preoperative exercise and nutritional therapy for patients undergoing hepato-pancreato-biliary surgeries for malignancy. Ann Surg Oncol 26(1):264–272. https://doi.org/10.1245/s10434-018-6943-2
Fulop A, Lakatos L, Susztak N, Szijarto A, Banky B (2020) The effect of trimodal prehabilitation on the physical and psychological health of patients undergoing colorectal surgery: a randomised clinical trial. Anaesthesia. https://doi.org/10.1111/anae.15215
Jensen BT, Petersen AK, Jensen JB, Laustsen S, Borre M (2014) Efficacy of a multiprofessional rehabilitation programme in radical cystectomy pathways: a prospective randomized controlled trial. Scand J Urol 49(2):133–141. https://doi.org/10.3109/21681805.2014.967810
Waller E, Sutton P, Rahman S, Allen J, Saxton J, Aziz O (2021) Prehabilitation with wearables versus standard of care before major abdominal cancer surgery: a randomised controlled pilot study (trial registration: NCT04047524). Surg Endosc 15:15. https://doi.org/10.1007/s00464-021-08365-6
Pang NQ, He SS, Foo JQX, Koh NHY, Yuen TW, Liew MN et al (2021) Multimodal prehabilitation before major abdominal surgery: a retrospective study. Ann Acad Med Singap 50(12):892–902. https://doi.org/10.47102/annals-acadmedsg.2021264
de Klerk M, van Dalen DH, Nahar-van Venrooij LMW, Meijerink W, Verdaasdonk EGG (2021) A multimodal prehabilitation program in high-risk patients undergoing elective resection for colorectal cancer: a retrospective cohort study. Eur J Surg Oncol 47(11):2849–2856. https://doi.org/10.1016/j.ejso.2021.05.033
Abeles A, Kwasnicki RM, Darzi A (2017) Enhanced recovery after surgery: current research insights and future direction. World J Gastrointest Surg 9(2):37–45. https://doi.org/10.4240/wjgs.v9.i2.37
Gillis C, Buhler K, Bresee L, Carli F, Gramlich L, Culos-Reed N et al (2018) Effects of nutritional prehabilitation, with and without exercise, on outcomes of patients who undergo colorectal surgery: a systematic review and meta-analysis. Gastroenterology 155(2):391-410.e4. https://doi.org/10.1053/j.gastro.2018.05.012
Moran J, Guinan E, McCormick P, Larkin J, Mockler D, Hussey J et al (2016) The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery 160(5):1189–1201. https://doi.org/10.1016/j.surg.2016.05.014
Valkenet K, van de Port IG, Dronkers JJ, de Vries WR, Lindeman E, Backx FJ (2011) The effects of preoperative exercise therapy on postoperative outcome: a systematic review. Clin Rehabil 25(2):99–111. https://doi.org/10.1177/0269215510380830
Gupta D, Vashi PG, Lammersfeld CA, Braun DP (2011) Role of nutritional status in predicting the length of stay in cancer: a systematic review of the epidemiological literature. Ann Nutr Metab 59(2–4):96–106. https://doi.org/10.1159/000332914
van der Kroft G, Janssen-Heijnen MLG, van Berlo CLH, Konsten JLM (2015) Evaluation of nutritional status as an independent predictor of post-operative complications and morbidity after gastro-intestinal surgery. Clin Nutr ESPEN 10(4):e129–e133. https://doi.org/10.1016/j.clnesp.2015.05.005
Kwag S-J, Kim J-G, Kang W-K, Lee J-K, Oh S-T (2014) The nutritional risk is a independent factor for postoperative morbidity in surgery for colorectal cancer. Ann 86(4):206–211. https://doi.org/10.4174/astr.2014.86.4.206
Kanda M, Fujii T, Kodera Y, Nagai S, Takeda S, Nakao A (2011) Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg 98(2):268–274. https://doi.org/10.1002/bjs.7305
Piraux E, Caty G, Reychler G (2018) Effects of preoperative combined aerobic and resistance exercise training in cancer patients undergoing tumour resection surgery: a systematic review of randomised trials. Surg Oncol 27(3):584–594. https://doi.org/10.1016/j.suronc.2018.07.007
Moran J, Guinan E, McCormick P, Larkin J, Mockler D, Hussey J et al (2016) The ability of prehabilitation to influence postoperative outcome in intra-abdominalsurgery: a systematic review and metaanalysis. Anaesthesia 71:30. https://doi.org/10.1111/anae.13637
Solway S, Brooks D, Lacasse Y, Thomas S (2001) A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest 119(1):256–270. https://doi.org/10.1378/chest.119.1.256
Waterland JL, McCourt O, Edbrooke L, Granger CL, Ismail H, Riedel B et al (2021) Efficacy of prehabilitation including exercise on postoperative outcomes following abdominal cancer surgery: a systematic review and meta-analysis. Front Surg 8(55):628848. https://doi.org/10.3389/fsurg.2021.628848
Gillis C, Wischmeyer PE (2019) Pre-operative nutrition and the elective surgical patient: Why, how and what? Anaesthesia 74(S1):27–35. https://doi.org/10.1111/anae.14506
Carli F (2015) Physiologic considerations of enhanced recovery after surgery (ERAS) programs: implications of the stress response. Can J Anesth/J Can d’anesthésie 62(2):110–119. https://doi.org/10.1007/s12630-014-0264-0
Santa Mina D, Sellers D, Au D, Alibhai SMH, Clarke H, Cuthbertson BH et al (2021) A pragmatic non-randomized trial of prehabilitation prior to cancer surgery: study protocol and COVID-19-related adaptations. Front Oncol 11(389):629207. https://doi.org/10.3389/fonc.2021.629207
Moore J, Merchant Z, Rowlinson K, McEwan K, Evison M, Faulkner G et al (2021) Implementing a system-wide cancer prehabilitation programme: the journey of greater manchester’s “Prehab4cancer.” Eur J Surg Oncol 47(3):524–532. https://doi.org/10.1016/j.ejso.2020.04.042
Gillis C, Carli F (2021) Patients with poor functional walking capacity experience significantly more medical complications post-colorectal surgery than those with higher functional walking capacity. Eur J Surg Oncol 47(5):1230–1231. https://doi.org/10.1016/j.ejso.2021.02.023
Older PO, Levett DZH (2017) Cardiopulmonary exercise testing and surgery. Ann Am Thorac Soc 14(1):S74–S83. https://doi.org/10.1513/AnnalsATS.201610-780FR
Galata C, Busse L, Birgin E, Weiß C, Hardt J, Reißfelder C et al (2020) Role of albumin as a nutritional and prognostic marker in elective intestinal surgery. Can J Gastroenterol Hepatol 2020:7028216. https://doi.org/10.1155/2020/7028216
Hijazi Y, Gondal U, Aziz O (2017) A systematic review of prehabilitation programs in abdominal cancer surgery. Int J Surg 39:156–162. https://doi.org/10.1016/j.ijsu.2017.01.111
Acknowledgements
We would like to thank Ms Annelissa Chin from Yong Loo Lin School of Medicine, Medical Library, for advising us with the search strategy for this meta-analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jain, S.R., Kandarpa, V.L., Yaow, C.Y.L. et al. The Role and Effect of Multimodal Prehabilitation Before Major Abdominal Surgery: A Systemic Review and Meta-Analysis. World J Surg 47, 86–102 (2023). https://doi.org/10.1007/s00268-022-06761-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06761-0