Abstract
Background
Despite curative resection, hepatocellular carcinoma (HCC) has a high probability of recurrence. We validated the potential role of liver resection (LR) for recurrent HCC.
Methods
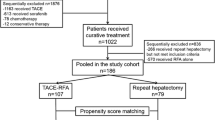
Patients with intrahepatic recurrence with up to three lesions were included. We compared survival times of patients undergoing their first LR to those of patients undergoing repeated LR. Then, survival times of the patients who had undergone LR and transcatheter chemoembolization (TACE) for recurrent HCC after propensity score matching were compared.
Results
After a median follow-up period of 3.1 years (range, 0.2–16.3), median overall survival times were 6.5 years (95% CI 6.0–7.0), 5.7 years (5.2–6.2), and 5.1 years (4.9–7.3) for the first LR (n = 1234), second LR (n = 273), and third LR (n = 90) groups, respectively. Severe complications frequently occurred in the first LR group (p = 0.059). Operative times were significantly longer for the third LR group (p = 0.012). After the first recurrence, median survival times after one-to-one pair matching were 5.7 years (95% CI 4.5–6.5) and 3.1 years (2.1–3.8) for the second LR group (n = 146) and TACE group (n = 146), respectively (p < 0.001). The median survival time of the third LR group (n = 41) (6.2 years; 95% CI 3.7–NA) was also longer than that of TACE group (n = 41) (3.4 years; 1.8–4.5; p = 0.010) after the second recurrence.
Conclusions
Repeated LR for recurrent HCC is the procedure of choice if there are three or fewer tumors.



Similar content being viewed by others
References
Midorikawa Y, Takayama T, Higaki T et al (2016) Early hepatocellular carcinoma as a signaling lesion for subsequent malignancy. Jpn J Clin Oncol 46:1102–1107
Yagi R, Midorikawa Y, Moriguchi M et al (2018) Liver resection for recurrent hepatocellular carcinoma to improve survivability: a proposal of indication criteria. Surgery 163:1250–1256
Yamagishi S, Midorikawa Y, Nakayama H et al (2019) Liver resection for recurrent hepatocellular carcinoma after radiofrequency ablation therapy. Hepatol Res 49:432–440
Mise Y, Hasegawa K, Shindoh J et al (2015) The feasibility of third or more repeat hepatectomy for recurrent hepatocellular carcinoma. Ann Surg 262:347–357
Roayaie S, Bassi D, Tarchi P et al (2011) Second hepatic resection for recurrent hepatocellular cancer: a Western experience. J Hepatol 55:346–350
Wu CC, Cheng SB, Yeh DC et al (2009) Second and third hepatectomies for recurrent hepatocellular carcinoma are justified. Br J Surg 96:1049–1057
Yamashita Y, Shirabe K, Tsuijita E et al (2013) Third or more repeat hepatectomy for recurrent hepatocellular carcinoma. Surgery 154:1038–1045
Yoh T, Seo S, Taura K et al (2019) Surgery for recurrent hepatocellular carcinoma: achieving long-term survival. Ann Surg. https://doi.org/10.1097/sla.0000000000003358
Faber W, Seehofer D, Neuhaus P et al (2011) Repeated liver resection for recurrent hepatocellular carcinoma. J Gastroenterol Hepatol 26:1189–1194
Choi JW, Park JY, Ahn SH et al (2009) Efficacy and safety of transarterial chemoembolization in recurrent hepatocellular carcinoma after curative surgical resection. Am J Clin Oncol 32:564–569
Zu QQ, Liu S, Zhou CG et al (2015) Chemoembolization of recurrent hepatoma after curative resection: prognostic factors. AJR Am J Roentgenol 204:1322–1328
Chan AC, Poon RT, Cheung TT et al (2012) Survival analysis of re-resection versus radiofrequency ablation for intrahepatic recurrence after hepatectomy for hepatocellular carcinoma. World J Surg 36:151–156. https://doi.org/10.1007/s00268-011-1323-0
Song KD, Lim HK, Rhim H et al (2015) Repeated hepatic resection versus radiofrequency ablation for recurrent hepatocellular carcinoma after hepatic resection: a propensity score matching study. Radiology 275:599–608
Chan AC, Chan SC, Chok KS et al (2013) Treatment strategy for recurrent hepatocellular carcinoma: salvage transplantation, repeated resection, or radiofrequency ablation? Liver Transpl 19:411–419
Shan Y, Huang L, Xia Q (2017) Salvage liver transplantation leads to poorer outcome in hepatocellular carcinoma compared with primary liver transplantation. Sci Rep 7:44652
Liang HH, Chen MS, Peng ZW et al (2008) Percutaneous radiofrequency ablation versus repeat hepatectomy for recurrent hepatocellular carcinoma: a retrospective study. Ann Surg Oncol 15:3484–3493
Sekhon JS (2011) Multivariate and propensity score matching software with automated balance optimization: the matching package for R. J Stat Softw 42:1–52
Kokudo N, Hasegawa K, Akahane M et al (2015) Evidence-based clinical practice guidelines for hepatocellular carcinoma: the Japan Society of Hepatology 2013 update (3rd JSH-HCC Guidelines). Hepatol Res 45:123–127
Takayama T, Makuuchi M, Kubota K et al (2001) Randomized comparison of ultrasonic vs clamp transection of the liver. Arch Surg 136:922–928
Yamazaki S, Takayama T, Moriguchi M et al (2012) Criteria for drain removal following liver resection. Br J Surg 99:1584–1590
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Aramaki O, Takayama T, Higaki T et al (2014) Decreased blood loss reduces postoperative complications in resection for hepatocellular carcinoma. J Hepatobiliary Pancreat Sci 21:585–591
Midorikawa Y, Takayama T, Shimada K et al (2013) Marginal survival benefit in the treatment of early hepatocellular carcinoma. J Hepatol 58:306–311
Makuuchi M, Kosuge T, Takayama T et al (1993) Surgery for small liver cancers. Semin Surg Oncol 9:298–304
The San-in Group of Liver Surgery (1997) Long-term oral administration of branched chain amino acids after curative resection of hepatocellular carcinoma: a prospective randomized trial. Br J Surg 84:1525–1531
Harimoto N, Yoshizumi T, Inokuchi S et al (2018) Prognostic significance of preoperative controlling nutritional status (CONUT) score in patients undergoing hepatic resection for hepatocellular carcinoma: a multi-institutional study. Ann Surg Oncol 25:3316–3323
Dahabreh IJ, Sheldrick RC, Paulus JK et al (2012) Do observational studies using propensity score methods agree with randomized trials? A systematic comparison of studies on acute coronary syndromes. Eur Heart J 33:1893–1901
Shimizu A, Hasegawa K, Masuda K et al (2018) Efficacy of hyaluronic acid/carboxymethyl cellulose-based bioresorbable membranes in reducing perihepatic adhesion formation: a prospective cohort study. Dig Surg 35:95–103
Ichida A, Hasegawa K, Takayama T et al (2016) Randomized clinical trial comparing two vessel-sealing devices with crush clamping during liver transection. Br J Surg 103:1795–1803
Chen MS, Li JQ, Zheng Y et al (2006) A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 243:321–328
Feng K, Yan J, Li X et al (2012) A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 57:794–802
Huang J, Yan L, Cheng Z et al (2010) A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg 252:903–912
Xu XL, Liu XD, Liang M et al (2018) Radiofrequency ablation versus hepatic resection for small hepatocellular carcinoma: systematic review of randomized controlled trials with meta-analysis and trial sequential analysis. Radiology 287:461–472
Taura K, Ikai I, Hatano E et al (2006) Implication of frequent local ablation therapy for intrahepatic recurrence in prolonged survival of patients with hepatocellular carcinoma undergoing hepatic resection: an analysis of 610 patients over 16 years old. Ann Surg 244:265–273
Fields TD, Philips P, Scoggins CR et al (2017) Multi-disciplinary concurrent management of recurrent hepatocellular therapy is superior to sequential therapy. World J Surg 41:1331–1339. https://doi.org/10.1007/s00268-016-3844-z
Funding
This research was supported by AMED under Grant Number JP18hk0102049 and a Grants-in-aid of the 106th Annual Congress of JSS Memorial Surgical Research Fund, Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Midorikawa, Y., Takayama, T., Moriguchi, M. et al. Liver Resection Versus Embolization for Recurrent Hepatocellular Carcinoma. World J Surg 44, 232–240 (2020). https://doi.org/10.1007/s00268-019-05225-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05225-2