Abstract
Background
Perioperative anaemia in relation to surgery is associated with adverse clinical outcomes. In an elective surgical setting, it is possible to optimize patients prior to surgery, often by iron supplementation with correction of anaemia. Possibilities for optimization prior to and during acute surgical procedures are limited. This review investigates whether iron treatment initiated perioperatively improves outcomes in patients undergoing major acute non-cardiac surgery.
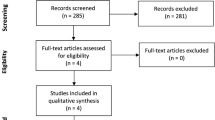
Method
This systematic review was performed using PubMed, EMBASE (Ovid) and Scopus to identify current evidence on iron supplementation in acute surgery. Primary outcomes were allogenic blood transfusion (ABT) rate and changes in haemoglobin. Secondary outcomes were postoperative mortality, length of stay (LOS), and postoperative complications. Iron was administered at latest within 24 h after end of surgery.
Results
Of the 5413 studies screened, four randomized controlled trials and nine observational cohort studies were included. Ten studies included patients with hip fractures. A meta-analysis of seven studies showed a risk reduction of transfusion (OR = 0.35 CI 95% (0.20–0.63), p = 0.0004, I2 = 66%). No influence on plasma haemoglobin was found. Postoperative mortality was reduced in the iron therapy group in a meta-analysis of four observational studies (OR 0.50 (CI 95% 0.26–0.96) p = 0.04). No effect was found on LOS, but a reduction in postoperative infection was seen in four studies.
Conclusions
This review examined perioperative iron therapy in acute major non-cardiac surgery. IV iron showed a lower 30-day mortality, a reduction in postoperative infections and a reduction in ABT largely due to the observational studies. The review primarily consisted of small observational studies and does not have the power to formally recommend this practice.





Similar content being viewed by others
References
Musallam KM et al (2011) Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet (London, England) 378:1396–1407
Lopes AM et al (2017) Postoperative haematocrit and outcome in critically ill surgical patients. Acta Med Port 30:555–560
Matsuyama T et al (2013) Risk factors for postoperative mortality and morbidities in emergency surgeries. J Anesth 27:838–843
Havens JM et al (2016) Explaining the excess morbidity of emergency general surgery: packed red blood cell and fresh frozen plasma transfusion practices are associated with major complications in nonmassively transfused patients. Am J Surg 211:656–663.e4
Muñoz M, Gómez-Ramírez S, Campos A (2014) Iron supplementation for perioperative anaemia in patient blood management. EMJ Rev 1:123–132
Lidder PG et al (2007) Pre-operative oral iron supplementation reduces blood transfusion in colorectal surgery—a prospective, randomised, controlled trial. Ann R Coll Surg Engl 89:418–421
Rogers BA, Cowie A, Alcock C, Rosson JW (2008) Identification and treatment of anaemia in patients awaiting hip replacement. Ann R Coll Surg Engl 90:504–507
Theusinger OM, Leyvraz P-F, Schanz U, Seifert B, Spahn DR (2007) Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology 107:923–927
Litton E, Xiao J, Ho KM (2013) Safety and efficacy of intravenous iron therapy in reducing requirement for allogeneic blood transfusion: systematic review and meta-analysis of randomised clinical trials. BMJ 347:f4822
Muñoz M et al (2009) Usefulness of the administration of intravenous iron sucrose for the correction of preoperative anemia in major surgery patients. Med Clin 132:303–306
Gonzalez-Porras JR et al (2009) An individualized pre-operative blood saving protocol can increase pre-operative haemoglobin levels and reduce the need for transfusion in elective total hip or knee arthroplasty. Transfus Med 19:35–42
Ingraham AM, Haas B, Cohen ME, Ko CY, Nathens AB (2012) Comparison of hospital performance in trauma vs emergency and elective general surgery: implications for acute care surgery quality improvement. Arch Surg 147:591–598
Vester-Andersen M et al (2014) Mortality and postoperative care pathways after emergency gastrointestinal surgery in 2904 patients: a population-based cohort study. Br J Anaesth 112:860–870
Havens JM et al (2015) The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg 78:306–311
Leal-Noval SR et al (2013) Spanish consensus statement on alternatives to allogeneic blood transfusion: the 2013 update of the ‘Seville document’. Blood Transfus 11:585–610
Beris P et al (2008) Perioperative anaemia management: consensus statement on the role of intravenous iron. Br J Anaesth 100:599–604
Torres S et al (2006) Intravenous iron following cardiac surgery does not increase the infection rate. Surg Infect (Larchmt) 7:361–366
Muñoz M et al (2013) Very-short-term perioperative intravenous iron administration and postoperative outcome in major orthopedic surgery: a pooled analysis of observational data from 2547 patients. Transfusion 54:289–299
Muñoz M et al (2014) Cost of post-operative intravenous iron therapy in total lower limb arthroplasty: a retrospective, matched cohort study. Blood Transfus 12:40–49
Jeong O, Park YK (2014) Effect of intravenous iron supplementation for acute postoperative anemia in patients undergoing gastrectomy for gastric carcinoma: a pilot study. Ann Surg Oncol 21:547–552
Titos-Arcos JC et al (2012) Is intravenous iron useful for reducing transfusions in surgically treated colorectal cancer patients? World J Surg 36:1893–1897. https://doi.org/10.1007/s00268-012-1589-x
Nagaraju SP, Cohn A, Akbari A, Davis JL, Zimmerman DL (2013) Heme iron polypeptide for the treatment of iron deficiency anemia in non-dialysis chronic kidney disease patients: a randomized controlled trial. BMC Nephrol 14:64
Giordano G et al (2011) Intravenous iron support vs oral liposomal iron support in patients with refractory anemia treated with Epo alpha. Monocentric prospective study. 11th Int Symp Myelodysplastic Syndr MDS Edinb U. K. 35:S137
Moher D et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
Higgins JPT et al (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013) The Newcastle–Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Prasad N, Rajamani V, Hullin D, Murray JM (2009) Post-operative anaemia in femoral neck fracture patients: does it need treatment? A single blinded prospective randomised controlled trial. Injury 40:1073–1076
Parker MJ (2010) Iron supplementation for anemia after hip fracture surgery. J Bone Jt Surg Am 92:265–269
Serrano-Trenas JA et al (2011) Role of perioperative intravenous iron therapy in elderly hip fracture patients: a single-center randomized controlled trial. Transfusion 51:97–104
Karkouti K et al (2006) Intravenous iron and recombinant erythropoietin for the treatment of postoperative anemia. Can J Anesth 53:11–19
Blanco Rubio N et al (2013) Hierro intravenoso preoperatorio como estrategia de ahorro de sangre en cirugía de fractura de cadera. Med Clin (Barc) 141:371–375
Izuel-Rami M et al (2005) Efectividad de distintas pautas de tratamiento de la anemia perioperatoria en pacientes ancianos con fractura de cadera. Farm Hosp 29:250–257
Cuenca Espiérrez J, Antonio García Erce J, Martínez Martín ÁA, Manuel Solano V, Javier Modrego Aranda F (2004) Seguridad y eficacia del hierro intravenoso en la anemia aguda por fractura trocantérea de cadera en el anciano. Med Clin (Barc) 123:281–285
Cuenca J et al (2005) Role of parenteral iron in the management of anaemia in the elderly patient undergoing displaced subcapital hip fracture repair: preliminary data. Arch Orthop Trauma Surg 125:342–347
Cuenca J et al (2004) Patients with pertrochanteric hip fracture may benefit from preoperative intravenous iron therapy: a pilot study. Transfusion 44:1447–1452
García-Erce JA et al (2005) Perioperative stimulation of erythropoiesis with intravenous iron and erythropoietin reduces transfusion requirements in patients with hip fracture. A prospective observational study. Vox Sang 88:235–243
Armand-Ugón R et al (2011) Efficacy of intravenous iron for treating postpartum anemia in low-resource african countries: a pilot study in Malawi. J Women’s Heal 20:123–127
Panarese A et al (2016) Can bloodless surgery be applied to every patient undergoing major abdominal surgical intervention? Arch Hell Med 33:826–830
Clevenger B, Kelleher A (2014) Hazards of blood transfusion in adults and children. Contin Educ Anaesth Crit Care Pain 14:112–118
Salpeter SR, Buckley JS, Chatterjee S (2014) Impact of more restrictive blood transfusion strategies on clinical outcomes: a meta-analysis and systematic review. Am J Med 127:124–131.e3
Avni T et al (2015) The safety of intravenous iron preparations: systematic review and meta-analysis. Mayo Clin Proc 90:12–23
Hallward G, Balani N, McCorkell S, Roxburgh J, Cornelius V (2016) The relationship between preoperative hemoglobin concentration, use of hospital resources, and outcomes in cardiac surgery. J Cardiothorac Vasc Anesth 30:901–908
Elhenawy AM, Meyer SR, Bagshaw SM, MacArthur RG, Carroll LJ (2015) Role of preoperative intravenous iron therapy to correct anemia before major surgery: study protocol for systematic review and meta-analysis. Syst Rev 4:29
Muñoz M et al (2017) International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 72:233–247
Huddart S, Peden C, Quiney N (2013) Emergency major abdominal surgery—‘the times they are a-changing’. Colorectal Dis 15:645–649
Foss NB, Kehlet H (2006) Hidden blood loss after surgery for hip fracture. J Bone Jt Surg Br 88:1053–1059
Baigrie RJ, Lamont PM, Kwiatkowski D, Dallman MJ, Morris PJ (1992) Systemic cytokine response after major surgery. Br J Surg 79:757–760
Prakash D (2012) Anemia in the ICU. Anemia of chronic disease versus anemia of acute illness. Crit Care Clin 28:333–343
Muñoz M et al (2018) An international consensus statement on the management of postoperative anaemia after major surgical procedures. Anaesthesia. https://doi.org/10.1111/anae.14358
Author information
Authors and Affiliations
Contributions
AS helped in study design, study selection, data collection, data analysis, data interpretation, drafting of manuscript, and critical revision. AAB helped in study selection and critical revision. SE contributed to study design, data interpretation, and critical revision. IG participated in data interpretation and critical revision. JB performed study design, data analysis, data interpretation, and critical revision.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Search strategy
(((((((((((((((((((Abdomen) OR abdominal) OR Surgery) OR Abdomen, Acute) OR Digestive System Surgical Procedures) OR General Surgery) OR Specialties, Surgical) OR ((Bloodless Medical and Surgical Procedures)))) OR Abdominal Cavity/surgery)) OR Blood Loss, Surgical)))) AND (((((((((Postoperative) OR Perioperative) OR Perioperative period) OR Postoperative care) OR Preoperative Care) OR Emergency) OR Emergencies)) OR acute))) AND ((((((((iron) OR Iron therapeutic) OR Iron administration) OR Ferric Compounds) OR Ferrous Compounds)) OR hematinics)))) AND (((((((((Perioperative outcomes) OR Postoperative complications) OR Long term outcomes) OR Short term outcomes) OR Mortality) OR Treatment outcome) OR Blood transfusion) OR Length of Stay))
Appendix 2
References | Prasad et al. [27] | Parker [28] | Karkouti et al. [30] | Serrano-Trenas et al. [29] |
|---|---|---|---|---|
Random sequence generation | Low | Low | Low | Low |
Allocation concealment | Low | Low | Low | Low |
Selective reporting | Unclear | Low | Unclear | Low |
Other bias | Low | Low | Unclear | Low |
Blinding of participants and personnel | Low | High | Low | Low |
Blinding of outcome assessment | Low | Unclear | Low | Low |
Incomplete outcome data | Low | Low | Low | Low |
Quality | High | Fair | High | High |
Appendix 3
References | Panarese et al. [38] | Blanco-Rubio et al. [31] | Izuel-Rami et al. [32] | Muñoz et al. [18] | Cuenca Espiérrez et al. [33] | Cuenca et al. [34] | Cuenca et al. [35] | Garcla-Erce et al. [36] | Armand-Ugón et al. [37] |
|---|---|---|---|---|---|---|---|---|---|
Selection (max 4) | * | *** | *** | **** | *** | ** | ** | *** | ** |
Comparability (max 2) | * | * | ** | * | |||||
Outcome (max 3) | ** | * | * | *** | *** | ** | ** | *** | ** |
Total (max 9) | *** | ***** | ***** | ******* | ****** | **** | **** | ******** | ***** |
Rights and permissions
About this article
Cite this article
Schack, A., Berkfors, A.A., Ekeloef, S. et al. The Effect of Perioperative Iron Therapy in Acute Major Non-cardiac Surgery on Allogenic Blood Transfusion and Postoperative Haemoglobin Levels: A Systematic Review and Meta-analysis. World J Surg 43, 1677–1691 (2019). https://doi.org/10.1007/s00268-019-04971-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-04971-7