Abstract
Background
Morbid obesity is usually accompanied by both subcutaneous and visceral fat accumulation. Fat can mimic an air bag, absorbing the force of a collision. We hypothesized that morbid obesity is mechanically protective for hollow viscus organs in blunt abdominal trauma (BAT).
Methods
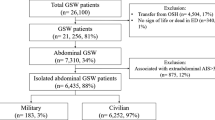
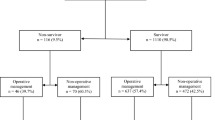
The National Trauma Data Bank (NTDB) was queried for BAT patients from 2013 to 2015. We looked at the rate of gastrointestinal (GI) tract injuries in all BAT patients with different BMIs. A subset analysis of BAT patients with operative GI tract injuries was performed to evaluate the need for abdominal operation. Multivariate analyses were carried out to identify factors independently associated with increased GI tract injuries and associated abdominal operations.
Results
A total of 100,459 BAT patients were evaluated in the NTDB. Patients with GI tract injury had a lower proportion of morbidly obese patients [body weight index (BMI) ≥ 40 kg/m2)] (3.7% vs. 4.2%, p = 0.015) and instead had more underweight patients (BMI < 18.5) (5.9% vs. 5.0%, p < 0.001). The risk of GI tract injury decreased 11.6% independently in morbidly obese patients and increased 15.7% in underweight patients. Of the patients with GI tract injuries (N = 11,467), patients who needed a GI operation had a significantly lower proportion of morbidly obese patients (3.2% vs. 5.3%, p < 0.001). The risk of abdominal operation for GI tract injury decreased 57.3% independently in morbidly obese patients. Compared with underweight patients, morbidly obese patients had significantly less GI tract injury (6.0% vs. 13.3%, p < 0.001) and associated abdominal operation rates (65.2% vs. 73.3%, p < 0.001).
Conclusion
Obesity is protective in BAT. This translates into lower rates of GI tract injury and operation in morbidly obese patients. In contrast, underweight patients appear to suffer a higher rate of GI tract injury and associated GI operations.


Similar content being viewed by others
References
World Health Organization (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:1–253
Berghofer A, Pischon T, Reinhold T et al (2008) Obesity prevalence from a European perspective: a systematic review. BMC Public Health 8:200
Calle EE, Thun MJ, Petrelli JM et al (1999) Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med 341:1097
Haslam DW, James WP (2005) Obesity. Lancet 366:209–1197
Schwimmer JB, Burwinkle TM, Varni JW (2003) Health-related quality of life of severely obese children and adolescents. JAMA 289:1813–1819
Bège T, Lelong B, Francon D et al (2009) Impact of obesity on short-term results of laparoscopic rectal cancer resection. Surg Endosc 23:4–1460
Chen CL, Shore AD, Johns R et al (2011) The impact of obesity on breast surgery complications. Plast Reconstr Surg 128:395e–402e
Drenick EJ, Bale GS, Seltzer F et al (1980) Excessive mortality and causes of death in morbidly obese men. JAMA 243:443–445
Krishna SG, Hinton A, Oza V et al (2015) Morbid obesity is associated with adverse clinical outcomes in acute pancreatitis: a propensity-matched study. Am J Gastroenterol 110:19–1608
Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC (2004) Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol 43:44–1439
Niedziela J, Hudzik B, Niedziela N et al (2014) The obesity paradox in acute coronary syndrome: a meta-analysis. Eur J Epidemiol 29:12–801
Romero-Corral A, Montori VM, Somers VK et al (2006) Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet 368:78–666
Yusuf S, Hawken S, Ounpuu S et al (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364:52–937
Razay G, Vreugdenhil A, Wilcock G (2006) Obesity, abdominal obesity and Alzheimer disease. Dement Geriatr Cogn Disord 22:6–173
Cameron AJ, Zimmet PZ (2008) Expanding evidence for the multiple dangers of epidemic abdominal obesity. Circulation 117:6–1624
Gendall KA, Raniga S, Kennedy R, Frizelle FA (2007) The impact of obesity on outcome after major colorectal surgery. Dis Colon Rectum 50:37–2223
Scheidbach H, Benedix F, Hügel O et al (2008) Laparoscopic approach to colorectal procedures in the obese patient: risk factor or benefit? Obes Surg 18:66–70
Glance LG, Li Y, Osler TM et al (2014) Impact of obesity on mortality and complications in trauma patients. Ann Surg 259:81–576
Dhungel V, Liao J, Raut H et al (2015) Obesity delays functional recovery in trauma patients. J Surg Res 193:20–415
Ditillo M, Pandit V, Rhee P et al (2014) Morbid obesity predisposes trauma patients to worse outcomes: a national trauma data bank analysis. J Trauma Acute Care Surg 76:9–176
Watts DD, Fakhry SM (2003) East multi-institutional hollow viscus injury research group incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the east multi-institutional trial. J Trauma 54:289–294
Hughes TM, Elton C, Hitos K et al (2002) Intra-abdominal gastrointestinal tract injuries following blunt trauma: the experience of an Australian trauma centre. Injury 33:26–617
Bège T, Chaumoître K, Léone M et al (2014) Blunt bowel and mesenteric injuries detected on CT scan: who is really eligible for surgery? Eur J Trauma Emerg Surg 40:75–81
Vucenik I, Stains JP (2012) Obesity and cancer risk: evidence, mechanisms, and recommendations. Ann N Y Acad Sci 1271:37–43
World Health Organization (1995) Physical status: the use and interpretation of anthropometry. World Health Organization; 1995 WHO Technical Report Series. Geneva
Carbone F, La Rocca C, De Candia P et al (2016) Metabolic control of immune tolerance in health and autoimmunity. Semin Immunol 28:491–504
Harpsøe MC, Nielsen NM, Friis-Møller N et al (2016) Body mass index and risk of infections among women in the Danish National Birth Cohort. Am J Epidemiol 183:17–1008
Phung DT, Wang Z, Rutherford S et al (2013) Body mass index and risk of pneumonia: a systematic review and meta-analysis. Obes Rev 14:839–857
Grundy SM, Neeland IJ, Turer AT, Vega GL (2013) Waist circumference as measure of abdominal fat compartments. J Obes 2013:454285
Berentzen TL, Ängquist L, Kotronen A et al (2012) Waist circumference adjusted for body mass index and intra-abdominal fat mass. PLoS ONE 7:e32213
Author information
Authors and Affiliations
Contributions
Author contribution
Bokhari, Fu and Bajani contributed to study conception and design. Fu contributed to acquisition of data. Bokhari, Fu, Welsh, Bajani, Starr, Messer, Dennis, Kaminsky, Mis, Schlanser and Poulakidas analyzed and interpreted the data. Bokhari, Fu and Bajani drafted the manuscript. Bokhari, Fu and Bajani critically revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no commercial associations or sources of support that might pose a conflict of interest.
Rights and permissions
About this article
Cite this article
Fu, CY., Bajani, F., Butler, C. et al. Morbid Obesity’s Silver Lining: An Armor for Hollow Viscus in Blunt Abdominal Trauma. World J Surg 43, 1007–1013 (2019). https://doi.org/10.1007/s00268-018-4872-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4872-7