Abstract
Background
Emergency laparotomy is a high-risk procedure with increased morbidity and mortality rates. The long-term outcomes are poorly investigated.The aim was to describe the frequency of chronic postsurgical pain (CPSP), pain-related functional impairment, to evaluate the gastrointestinal quality of life (QoL) and identify risk factors for CPSP after emergency laparotomy.
Method
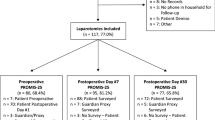
A questionnaire study was conducted from Copenhagen University Hospital Herlev. Population area: 435.000. Patients undergoing emergency midline laparotomy from May 2009–May 2013 and June 2014–November 2015 were included. The survey consisted of five parts exploring the extent of acute and chronic postsurgical pain. Pain-related functional impairment and quality of life were measured using the activity assessment scale and the gastrointestinal quality of life questionnaire, respectively. Primary outcomes were rates of CPSP and pain-related functional impairment. Gastrointestinal QoL was compared between patients with or without CPSP. Multivariate regression analysis was performed to estimate risk factors for CPSP.
Results
The primary emergency laparotomy population consisted of 1573 patients. A total of 605 patients were eligible for inclusion, and 440 patients completed the survey. Response rate: 73%. Median age was 69 years (range 18–95), 56.4% female. Median follow-up was 60 months (IQR 47). 19% (85/440) experienced CPSP and had low gastrointestinal QoL. We identified APSP OR 5.0 95%CI (2.4–10.5), p < 0.01 and age < 60 OR 2.1 95%CI (1.2–3.8), p = 0.01 as independent risk factors for CPSP. 45% (199/440) of all patients experienced moderate–severe functional impairment.
Conclusion
CPSP (19%) and low gastrointestinal QoL were common after emergency laparotomy and almost every second patient had moderate–severe functional impairment on long-term follow-up.


Similar content being viewed by others
References
Bruce J, Krukowski ZH (2006) Quality of life and chronic pain four years after gastrointestinal surgery. Dis Colon Rectum 49(9):1362–1370
Macrae WA (2001) Chronic pain after surgery. Br J Anaesth 87(1):88–98
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367(9522):1618–1625
Joshi GP, Kehlet H (2013) Procedure-specific pain management the road to improve postsurgical pain management? Anesthes 118(4):780–782
Bouras G, Marie Burns E, Howell A-M et al (2014) Systematic review of the impact of surgical harm on quality of life after general and gastrointestinal surgery. Ann Surg 260(6):975–983
Amemiya T, Oda K, Ando M et al (2007) Activities of daily living and quality of life of elderly patients after elective surgery for gastric and colorectal cancers. Ann Surg 246(2):222–228
Lawrence V, Hazuda H, Cornell J et al (2004) Functional independence after major abdominal surgery in the elderly. J Am Coll Surg 199(5):762–772
Al-Temimi MH, Griffee M, Enniss TM et al (2012) When is death inevitable after emergency laparotomy? analysis of the american college of surgeons national surgical quality improvement program database. ACS 215(4):503–511
Saunders DI, Murray D, Pichel AC et al (2012) Variations in mortality after emergency laparotomy: the first report of the UK emergency laparotomy network. Br J Anaesth 109(3):368–375
Tengberg LT, Cihoric M, Foss NB et al (2016) Complications after emergency laparotomy beyond the immediate postoperative period—a retrospective, observational cohort study of 1139 patients. Anaesth 72(3):309–316
Tolstrup MB, Watt SK, Gögenur I (2017) Morbidity and mortality rates after emergency abdominal surgery: an analysis of 4346 patients scheduled for emergency laparotomy or laparoscopy. Langenbecks Arch Surg 402(4):1–9
Tolstrup MB, Watt SK, Gögenur I (2017) Reduced rate of dehiscence after implementation of a standardized fascial closure technique in patients undergoing emergency laparotomy. Ann Surg 265(4):821–826
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol 20(4):250–280
Jeppesen M, Tolstrup MB, Gögenur I (2016) Chronic pain, quality of life, and functional impairment after surgery due to small bowel obstruction. World J Surg 40(9):2091–2097
Brandsborg B, Nikolajsen L, Hansen CT et al (2007) Risk factors for chronic pain after hysterectomy. Anesthes 106(5):1003–1012
Bennett MI, Smith BH, Torrance N et al (2005) The S-LANSS score for identifying pain of predominantly neuropathic origin: validation for use in clinical and postal research. J Pain 6(3):149–158
McCarthy M Jr, Jonasson O, Chang C-H et al (2005) Assessment of patient functional status after surgery. J Am Coll Surg 201(2):171–178
Aasvang EK, Gmaehle E, Hansen JB et al (2010) Predictive risk factors for persistent postherniotomy pain. Anesthes 112(4):957–969
Eypasch E, Williams JI, Wood-Dauphinee S et al (1995) Gastrointestinal quality of life index: development, validation and application of a new instrument. Br J Surg 82(2):216–222
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367(9522):1618–1625
VanDenKerkhof EG, Hopman WM, Reitsma ML et al (2012) Chronic pain, healthcare utilization, and quality of life following gastrointestinal surgery. Can J Anaesth 59(7):670–680
Boer KR, van Ruler O, Reitsma JB et al (2007) Health related quality of life six months following surgical treatment for secondary peritonitis—using the EQ-5D questionnaire. Health Qual Life Outcomes 5(1):35
Gupta A, Gandhi K, Viscusi ER (2011) Persistent postsurgical pain after abdominal surgery. YTRAP 15(3):140–146
Caumo W, Schmidt AP, Schneider CN et al (2002) Preoperative predictors of moderate to intense acute postoperative pain in patients undergoing abdominal surgery. Acta Anaesthesiol Scand 46(10):1265–1271
Perkins FM, Kehlet H (2000) Chronic pain as an outcome of surgery. Anesthes 93(4):1123–1133
Stiff G, Rhodes M, Kelly A et al (1994) Long-term pain: less common after laparoscopic than open cholecystectomy. Br J Surg 81(9):1368–1370
Baron R, Binder A, Wasner G (2010) Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol 9(8):807–819
Joris JL, Georges MJ, Medjahed K et al (2015) Prevalence, characteristics and risk factors of chronic postsurgical pain after laparoscopic colorectal surgery. Eur J Anaesthesiol 32(10):712–717
Gilron I, Vandenkerkhof E, Katz J et al (2017) Evaluating the association between acute and chronic pain after surgery. Clin J Pain J 33(7):588–594
Barber MD, Kenton K, Janz NK et al (2012) Validation of the activities assessment scale in women undergoing pelvic reconstructive surgery. Female Pelvic Med Reconstr Surg 18(4):205–210
Huddart S, Peden CJ, Swart M et al (2014) the ELPQuiC collaborator group. Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg 102(1):57–66
Tengberg LT, Bay-Nielsen M, Bisgaard T et al (2017) Multidisciplinary perioperative protocol in patients undergoing acute high-risk abdominal surgery. Br J Surg 104(4):463–471
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declares that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tolstrup, MB., Thorup, T. & Gögenur, I. Chronic Pain, Quality of Life and Functional Impairment After Emergency Laparotomy. World J Surg 43, 161–168 (2019). https://doi.org/10.1007/s00268-018-4778-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4778-4