Abstract
Objectives
Our aim in this pilot study was to identify potential predictors of chronic post-surgical pain (CPSP) and other outcomes to consider for inclusion in future prospective studies of CPSP following abdominal gastrointestinal surgery.
Methods
We followed 76 surgical patients during this prospective single-centre cohort study. Pain characteristics, health-related quality of life (HRQOL), and healthcare utilization were assessed preoperatively, at six weeks postoperatively, and at six months postoperatively. Statistical analyses included descriptive statistics and repeated measures analysis of variance.
Results
Prior to surgery, 42% of patients reported no pain, 18% reported remote pain, and 33% reported pain at the surgical site. Six months after surgery, 29% of patients with preoperative remote pain and 35% of patients with preoperative pain at the surgical site reported CPSP. Pain-related interference declined from the preoperative to postoperative period; however, six months after surgery almost one-third of participants continued to report pain-related interference with mood (28%), sleep (30%), and enjoyment of life (30%). Consistent with studies of other surgical procedures, measures of anxiety and depression were associated with an increased risk of CPSP. During the six months following surgery, 12% of patients visited the Emergency Department, 15% visited non-traditional providers, and 9.2% visited a walk-in clinic for pain. Compared with Canadian norms, HRQOL was poorer in all domains preoperatively, in all domains but mental health six weeks postoperatively, and in most domains six months postoperatively.
Conclusion
This feasibility study provides a template for future studies of CPSP following gastrointestinal surgery. Results suggest a substantial burden of persistent pain, healthcare utilization, and decreased HRQOL. Larger-scale studies that are similarly designed will serve to identify predictors of CPSP in this surgical population.
Résumé
Objectifs
Cette étude pilote a cherché à identifier d’éventuels éléments prédictifs de la douleur chronique post chirurgicale (CPSP) et d’autres résultats à inclure dans des études prospectives futures sur la CPSP après chirurgie digestive abdominale.
Méthodes
Cette étude de cohorte prospective a suivi 76 patients chirurgicaux dans un seul centre. Les caractéristiques de la douleur, la qualité de vie liée à la santé (HRQoL) et l’utilisation des soins de santé ont été évalués avant la chirurgie et à six semaines et à six mois après la chirurgie. Les analyses statistiques ont inclus des statistiques descriptives et une ANOVA pour mesures répétées.
Résultats
Avant la chirurgie, 42 % des patients n’ont signalé aucune douleur, 18 % une douleur à distance et 33 % une douleur au niveau du site chirurgical. Six mois après l’intervention, 29 % des patients ayant eu une douleur préopératoire à distance et 35 % de ceux ayant eu une douleur préopératoire au niveau du site chirurgical ont signalé une CPSP. Les perturbations liées à la douleur ont diminué entre la période préopératoire et la période postopératoire; toutefois, six mois après la chirurgie, presque un tiers des patients continuaient à signaler une interférence liée à la douleur sur l’humeur (28 %), le sommeil (30 %) et la joie de vivre (30 %). En accord avec des études portant sur d’autres interventions chirurgicales, les mesures de l’anxiété et de la dépression étaient associées à un plus grand risque de CPSP. Au cours des six mois suivant l’intervention chirurgicale, 12 % des patients sont allés au service des urgences, 15 % ont consulté des praticiens non traditionnels et 9,2 % sont allés dans une clinique de la douleur sans rendez-vous. En préopératoire, la HRQoL a été inférieure aux normes canadiennes dans tous les domaines, à l’exception de la santé mentale six semaines après l’intervention et de la majorité des domaines à six mois après chirurgie.
Conclusion
Cette étude de faisabilité procure un modèle pour de futures études de la CPSP après chirurgie digestive. Les résultats suggèrent une morbidité substantielle liée à la douleur persistante, l’utilisation des soins de santé et la baisse de l’HRQoL. Des études à plus grande échelle, utilisant le même plan, serviront à identifier les éléments prédictifs dans cette population chirurgicale.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic post-surgical pain (CPSP), defined as pain persisting for at least three to six months after surgery, is increasingly being recognized as a frequent outcome after routine surgery, with reported prevalence ranging from 10-50%.1-3 However, few studies on CPSP have assessed other outcomes, such as health-related quality of life (HRQOL), a broad multidimensional concept of self-reported physical and mental health4 and pain-related healthcare use. Regardless of type of surgical procedure, various biopsychosocial factors have been recognized to contribute to CPSP. Pre-existing pain has emerged as a potential predictor of CPSP; however, few studies have identified the influence of the location of preoperative pain (i.e., at or remote to the surgical condition/site) on the risk of CPSP. We recently reported both preoperative pain at the surgical site and remote pain as predictors of CPSP in women who underwent gynecological surgery.5 While conditions associated with a higher incidence of CPSP have attracted more interest (e.g., thoracotomy, limb amputation),6,7 all surgical procedures may lead to CPSP and may also be associated with the various contributory factors. Accordingly, we chose to address abdominal surgical procedures in this pilot study because: 1) these procedures are quite common (approximately 35% of surgeries performed in North America each year);8 2) these abdominal procedures may be associated with the same spectrum of potential contributors to CPSP as many other surgical procedures; and 3) CPSP after abdominal surgery has, thus far, received very little attention.
Thus, the purpose of this pilot study was to examine pain-related predictors and outcomes to be considered for inclusion in future prospective studies examining CPSP-related outcomes following abdominal gastrointestinal surgical procedures. The objectives were: 1) to describe the prevalence and incidence of pain from the preoperative period to the six-month postoperative period; 2) to examine the influence of preoperative and early postoperative characteristics on CPSP six months after surgery; 3) to describe pain-related healthcare utilization and medication use over this time period; and 4) to describe HRQOL from preoperatively to six months postoperatively and compare HRQOL with age- and sex-matched normative data.9
Methods
Ethics approval for this study was obtained from Queen’s University Health Sciences and the Affiliated Teaching Hospital’s Research Ethics Board. Guidelines for Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) were used to report the findings of this study.10
Study design
This prospective observational cohort study was conducted at the Kingston General Hospital, an acute care facility in Southeastern Ontario, Canada. A convenience sample of men and women scheduled for major abdominal general surgery was recruited preoperatively and followed for six months after surgery. Recruitment took place from January to November 2009. Participants were recruited in the week leading up to surgery and written informed consent was obtained. Prior to surgery, the participants answered web-based or paper questionnaires (participant preference) at home or in the Same Day Admission Centre. At the six-week and six-month follow-up, patients who answered the electronic questionnaires were sent an e-mail reminder and, if necessary, were telephoned asking them to complete the questionnaires. Patients who answered the paper questionnaires at follow-up were sent a questionnaire package at six-weeks and six-months. Non-responders were given a telephone reminder, and additional questionnaires were mailed as necessary. The date and format of data collection were recorded. The research assistant collected intraoperative and postoperative information from the patient record.
Sample
English-speaking men and women aged ≥ 18 yr and scheduled for elective general surgery were recruited to participate in the study. Subjects were excluded if they were currently enrolled in another study related to their surgery, if they had been diagnosed with Alzheimer’s disease or another form of cognitive impairment (as indicated in their medical record), or if they had a language barrier affecting their ability to complete the questionnaires.
Outcome variables
The study time line and measurement tools are outlined in Fig. 1. Since this was an exploratory pilot study, no single primary outcome measure was designated. The three pain-related outcome variables we explored in this study were CPSP, healthcare utilization for pain, and HRQOL.
Chronic post-surgical pain was defined using the criteria proposed by Macrae and Davies: pain must be present for a duration of at least two months; pain must develop after surgery; other causes of pain must be excluded; and the possibility that the pain is a continuation from a pre-existing problem must be explored.1 Chronic post-surgical pain was measured six months after surgery using the pain severity subscale of the Brief Pain Inventory – Short Form (BPI-SF).11,12 The first question of the BPI-SF was modified to reference surgical pain: “Have you had pain today that you believe is related to your surgery?” The pain severity subscale was divided into two categories: no pain (0/10) vs any pain (> 0/10) and none/mild pain (≤ 3/10) or moderate/severe pain (> 3/10).
Healthcare utilization (HCU) for pain was measured using questions in the BPI related to medication use and questions derived from questions in the Canadian Community Health Survey related to the number of visits to healthcare practitioners.13 Postoperatively, participants were sent home with a daily diary to record ratings of average, worst, and nocturnal pain (on a numeric rating scale [NRS] of 0-10)14 as well as medication and HCU.
Health-related quality of life was measured at three intervals (preoperatively, at six weeks postoperatively, and at six months postoperatively) using the SF-36®. The SF-36 is one of the most widely used and psychometrically sound instruments for measuring HRQOL.Footnote 1 , 15 The survey measures eight aspects of HRQOL: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. The domains are scored from 0-100, with 100 representing the best possible state of health. Two summary scores, the physical component summary (PCS) and the mental component summary (MCS), can also be derived. The PCS and MCS are standardized to a mean of 50, with a score > 50 representing better than average functioning and a score < 50 indicating poorer than average functioning.A, Footnote 2 A difference of five points in domain scores and a difference of two-three points in summary scores are considered clinically meaningful.A,B Health-related quality of life was compared with Canadian normative data, which are based on 9,423 participants sampled from nine areas in Canada (nine cities and a 50 km radius around each city to account for rural populations) and standardized to the Canadian population using census data.9 This provided an opportunity to compare the scores of the study population with their age- and sex-matched peers to assess burden of illness.9
Independent variables
Demographic variables included age, marital status, education level, and employment status. Age was analyzed as a continuous variable. Marital status, education level, and employment status (married/not married; ≤ high school diploma/> high school diploma; employed/not employed) were dichotomized.
Psychological variables included diagnosis of depression (from chart), depressive symptoms, state and trait anxiety, pain catastrophizing, and somatization (questionnaires). Depressive symptom status was measured using the Centre for Epidemiological Studies – Depression Scale.16 Depressive symptoms were classified as moderate/high based on a score ≥ 16/60. The State Trait Anxiety Inventory was used to measure state and trait anxiety.17 Scores were categorized into low (< 45) and high (≥ 45) anxiety. Pain catastrophizing was assessed using the two-item version of the pain catastrophizing scale.18 The two-item scale has been shown to have very strong correlation (R > .90) with the original Pain Catastrophizing Scale.19 Scores for the two-items were averaged to obtain a score ranging from 0-6. Due to the relatively low frequency of catastrophizing, it was classified as present (≥ 1/6) vs absent (0/6). Somatization was measured with the seven symptom screening test.20 Due to the low frequency of this event, somatization was categorized into present (≥ 1/7) or absent (0/7).
Preoperative clinical variables abstracted from the patient record included current smoking status (no/yes); body mass index (BMI) (underweight/normal [≤ 24.9 kg·m−2], overweight [≥ 25 to ≤ 29.9 kg·m−2], or obese [≥ 30 kg·m−2]); number of months from diagnosis to surgery (median); history of diabetes mellitus, hypertension, or osteoarthritis; previous abdominal surgery (no/yes); and American Society of Anesthesiologists’ physical status (I/II vs III/IV). Preoperative malignancy status was obtained from the hospital’s administrative database and was classified as not malignant or probably/definitely malignant.
Perioperative variables captured from the operating room record and patient chart included surgical procedure (large bowel, small bowel, and other general surgery), abdominal incision (no/yes), surgical approach (midline, subcostal, or other), suture material (staples vs absorbable or non-absorbable), anesthetic technique (general vs block [spinal/epidural] ± general), blood loss (mL), and operating time (minutes). Surgery complications (e.g., hematoma, infection) (yes/no) were reported by the participants six months after surgery.
Pain history included preoperative pain and opioid use. Detailed information was captured on preoperative pain status, including pain intensity, interference with function, and site of pain. Data were captured from the brief pain inventory-long form (BPI-LF) completed by the patient.11,21 The BPI-LF is similar to the short form but captures more detailed pain information, including pain quality, and the long form references pain over the past week rather than over the past 24 hr. Preoperative pain was categorized into no pain, pain related to surgical condition, or pain unrelated to surgical condition (remote). Pain was also characterized based on the 11 sensory and four affective descriptors from the BPI-LF. Pain scores captured from the patient record included highest pain scores (NRS 0-10) in the postanesthesia care unit (PACU) and on the post-surgical hospital ward, and discharge pain scores in the PACU and on the ward. Participants were also asked to “Please rate where you think your pain level will be one week (and six weeks) following surgery by circling one number on the scale of 0 to 10.” Preoperative opioid use was captured from the BPI-LF. Consumption of opioids and other analgesic treatments was captured from the question asking “What treatments or medications are you receiving for pain?”
Statistical analysis
Demographic, psychological, clinical, intraoperative, and pain history variables were summarized using frequencies, percentages, means (standard deviation), or medians [interquartile range]. Chronic post-surgical pain and HCU were summarized using frequencies and percentages, and bivariable analysis was conducted using the Chi square statistic. Repeated measures analysis of variance (ANOVA) was used for the HRQOL data to assess the within-subject change over time. The pairwise comparisons provided by the repeated measures ANOVA were used to examine the following data: preoperative to six-week postoperative, preoperative to six-month postoperative, and six-week to six-month postoperative. Each patient was assigned the HRQOL scores and standard deviations appropriate for his or her age, and paired Student’s t tests were then used to assess differences in HRQOL between the sample and the age-matched normative data at each of the three time points. To assess the influence of non-response, Student’s t tests for independent samples were used to examine baseline differences in HRQOL between those who completed the questionnaires and those who were lost to follow-up. All statistical analyses were completed using IBM SPSS® v19.0 (IBM Corporation, Chicago, IL, USA).
Results
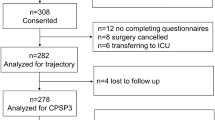
One hundred twenty-five patients awaiting general surgery were approached to participate in this study, 76 (61%) patients completed the preoperative questionnaires, and 71 (57%) completed the six-month follow-up questionnaires (Fig. 2). Baseline demographic and clinical variables are summarized in Table 1. The mean age (standard deviation) of study participants was 58 (14) yr and the majority were diagnosed with cancer. Due to small cell frequencies, surgical procedures were grouped into large bowel (63%), small bowel (9.2%), and other (28%). Seventy-two percent (55/76) underwent a midline abdominal incision. No surgical complications, such as infection or hematoma, were noted in the patient charts.
Pain characteristics
Prior to surgery, 42% (32/76) of patients reported no pain (NRS 0/10), 18% (14/76) reported other pain (remote to surgical site), and 33% (25/76) reported pain at the surgical site. Upon discharge from hospital, 47% (35/75) reported pain, with 13% (9/75) reporting moderate to severe pain. Six months after surgery, 3.1% (1/32) of patients with no preoperative pain, 29% (4/14) of patients with remote pain, and 35% (8/23) of patients with preoperative pain at the surgical site reported CPSP. Pain-related interference declined from the preoperative to the postoperative period; however, six months after surgery, pain interfered with mood in 28% (21/71) of respondents, with sleep in 30% (23/71) of respondents, and with enjoyment of life in 30% (23/71) of respondents (Table 2).
Potential predictors of CPSP for investigation in future studies
Several baseline characteristics more than doubled the risk of CPSP in bivariable analysis (preoperative pain and being female were the strongest predictors); however, only those with cell frequencies n ≥ 5 are reported in Table 3. Osteoarthritis, preoperative depressive symptoms, anxiety, and a high expectation of pain after surgery also increased the risk of CPSP. Other potential risk factors, such as moderate to severe acute postoperative pain, were not statistically significant predictors of CPSP, although 11% (6/57) of participants with none/mild acute pain reported CPSP compared with 29% (4/14) of participants with moderate to severe acute pain.
Healthcare utilization and medication use
Pain-related healthcare utilization and medications for pain in the year prior and six months following surgery are outlined in Table 2. In the year preceding surgery, 32% of participants visited the Emergency Department for pain and 13% visited a walk-in clinic. In the six months following surgery, 12% visited the Emergency Department and 9.2% visited a walk-in clinic.
Nine percent (9/76) reported taking strong opioids (e.g., morphine, hydromorphone) and 9% reported taking weak opioids (e.g., codeine) for pain in the year prior to surgery (Table 2). The proportion taking any opioids six months after surgery was < 7% (results not reported due to small cell frequencies).
Health-related quality of life
Health-related quality of life domain and summary scores (mean and standard error) for the preoperative period and the six-week and six-month postoperative periods are shown in Fig. 3. Higher scores represent better function and less pain. There were statistically significant within-subject changes over the three time points for the physical functioning, role-physical, bodily pain, and social functioning domains, and the PCS (P ≤ 0.01 for all). From preoperatively to six weeks postoperatively, there were decreases in the mean scores for physical function (−9.6; 95% confidence interval [CI] −15.4 to −3.8; P = 0.002), role-physical (−19.8; 95% CI −27.5 to −12.0; P < 0.001), and the PCS (−5.4; 95% CI −7.8 to −3.1; P < 0.001). From six weeks to six months postoperatively, there were improvements in the mean scores for physical functioning (11.6; 95% CI 5.6 to 17.6; P < 0.001), role-physical (24.9; 95% CI 17.8 to 32.1; P < 0.001), bodily pain (13.7; 95% CI 6.9 to 20.6; P < 0.001), social functioning (11.7; 95% CI 4.9 to 18.6; P = 0.001), role-emotional (7.6; 95% CI 1.4 to 13.7; P = 0.016), and the PCS (6.6; 95% CI 4.1 to 9.1; P < 0.001).
Based on Student’s t tests for independent samples examining baseline differences between the two groups, there were no differences in preoperative HRQOL between participants who completed the six-month follow-up questionnaires and those who were lost to follow-up.
The preoperative, six-week postoperative, and six-month postoperative HRQOL (bars) are compared with the Canadian normative data (line) in Fig. 3. Preoperatively, all eight domains and both the PCS and MCS scores were lower in the surgical cohort compared with Canadian norms. At six weeks postoperatively, the surgical cohort continued to report poorer HRQOL compared with Canadian norms, with the exception of mental health. Although scores did improve by six months, five domains and the two component summaries remained lower than the normative data. These differences in mean values were significant for physical functioning (−12.5; 95% CI −19.4 to −5.6; P = 0.001), role-physical (−15.4; 95% CI −22.8 to −8.0; P < 0.001), general health (−13.1; 95% CI −18.6 to −7.5; P < 0.001), vitality (−11.2; 95% CI −16.9 to −5.6; P < 0.001), social functioning (−12.8; 95% CI −19.4 to −6.3; P < 0.001), and both the PCS (−4.4; 95% CI −7.2 to −1.5; P = 0.003) and the MCS (−2.8; 95% CI −5.2 to −0.3; P = 0.027).
Discussion
During this pilot study, we followed a cohort of 76 patients from the preoperative period to six months after general surgery. Our purpose was to describe pain-related outcomes and potential predictors of CPSP for consideration in future prospective studies. The incidence of CPSP was very low in patients with no preoperative pain; however, 29% of patients reporting pain remote to the surgical site preoperatively and 35% of patients with preoperative pain at the surgical site reported CPSP six months after surgery. Furthermore, in approximately one-third of the participants, pain continued to interfere with mood, sleep, and enjoyment of life six months after surgery. A Swedish study reported slightly lower rates with ~30% reporting some form of pain or discomfort and ~6% reporting pain-related interference in daily activities.22 The lower rates may be related to the longer follow-up period of 24-36 months in the Swedish study, and the sample was limited to hernia surgery whereas the majority in our sample underwent bowel surgery.
Our findings also support the current evidence on the role of psychological factors on increasing the risk of CPSP. There was an increased risk of CPSP if patients reported preoperative depressive symptoms or anxiety. There are several review papers that report the role of depression and anxiety as an important predictor of CPSP; however, when the general surgery population is included, the focus of the majority is on hernia repair.6,7
There is a paucity of research examining HRQOL after general surgery. In our study, we compared HRQOL between the three time points (preoperatively, six weeks postoperatively, and six months postoperatively) and compared these with the general Canadian population. Health-related quality of life generally improved by six months after surgery. These findings are supported by our previous study in women undergoing gynecological surgery where all domains (except general health) and the two component scores improved six months after surgery.23 Other reports have shown differences in HRQOL (social functioning, mental health, and pain) between those with and without chronic pain24 and reduced HRQOL after several types of surgery, including inguinal hernia repair.3,25 Compared with age- and sex-matched norms in the general population, we found that the general surgery cohort experienced lower levels of HRQOL (physical functioning, role-physical, general health, vitality, social functioning, and the PCS and MCS), and these scores remained well below Canadian norms six months after surgery. This is contrary to findings in our previous study where six months after gynecological surgery HRQOL was close to that seen in the general population, and for some domains, it was significantly higher (bodily pain, role-emotional, mental health).23
Finally, we found pain-related HCU and medication use preoperatively and at six weeks and six months postoperatively. While intentional visits to a family doctor or specialist are expected during these periods, unintentional visits cause undue strain on the healthcare system, the patient, and the family. In our study, approximately one-third of patients visited the Emergency Department for pain in the year prior to surgery, and 12% of patients visited the Emergency Department for pain in the six months following surgery. Before surgery, 43% of patients reported taking medications for pain relief, and although the percentage decreased postoperatively, those taking medication for pain at six weeks and at six months were 34% and 28%, respectively.
Strengths and limitations
The prospective nature of this pilot study allowed us to generate preliminary estimates of the prevalence of preoperative pain and the incidence and potential risk factors for CPSP. In addition, there were minimal missing data for participants who completed the study. A further strength of this study is the evaluation of pain-related outcomes often not assessed in studies of CPSP (i.e., HRQOL, HCU, and medication use). The main limitation of our study is the small sample size and the limited ability to interpret the findings beyond descriptive and preliminary predictive analysis; however, the intent was to generate hypotheses for future studies rather than test specific hypotheses. This is a single-centre study and there were challenges in patient recruitment. We could not examine the effect of non-response as we did not seek consent to access information on individuals who refused to participate. Nevertheless, there was minimal loss to follow-up, and there were similar baseline characteristics between participants who completed the questionnaires and those who did not. A final limitation is the lack of corroborative evidence (e.g., clinical examination) regarding the presence of CPSP six months after surgery.
Clinical implications and future research
The results of this preliminary research cannot be easily generalized to the clinical setting due to the small sample size. Nevertheless, this study offers a useful template and supports the framework proposed for future studies exploring the etiology and outcomes of CPSP.26 This study provides 1) the incidence of CPSP to inform sample size estimates for planned large scale investigations, 2) preliminary analyses of common associations (e.g., relationship between preoperative pain and CPSP), and 3) feasibility of study design. Further analysis on larger samples is required to gain insight into outcomes beyond the simple measurement of pain (e.g., HRQOL and healthcare utilization related to CPSP).
Notes
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey - Manual and Interpretation Guide. Boston: The Health Institute, New England Medical Centre; 1993.
Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User's Manual. Boston: The Health Institute, New England Medical Centre; 1994.
References
Macrae WA, Davies HT. Chronic postsurgical pain. In: Crombie IK, Croft PR, Linton SJ, SeResche L, Von Korff M, editors. Epidemiology of Pain. Seattle: IASP Press; 1999. p. 125-42.
Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth 2008; 101: 77-86.
Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet 2006; 367: 1618-25.
U.S. Department of Health and Human Services; Centers for Disease Control and Prevention. Measuring Healthy Days: Population Assessment of Health-Related Quality of Life. Atlanta, Georgia: Centers for Disease Control and Prevention; November 2000. Available from URL: http://www.cdc.gov/hrqol/pdfs/mhd.pdf (accessed April 2012).
VanDenKerkhof EG, Hopman WM, Goldstein DH, et al. Impact of perioperative pain intensity, pain qualities, and opioid use on chronic pain after surgery: a prospective cohort study. Reg Anesth Pain Med 2012; 37: 19-27.
Hinrichs-Rocker A, Schulz K, Jarvinen I, Lefering R, Simanski C, Neugebauer EA. Psychosocial predictors and correlates for chronic post-surgical pain (CPSP) - a systematic review. Eur J Pain 2009; 13: 719-30.
Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother 2009; 9: 723-44.
Urbach DR, Stukel TA, Croxford R, MacCallum NL. Analysis of Current Research Related to the Impact of Low-Volume Procedure/Surgery and Care on Outcomes of Care. Toronto: Institute of Clinical Evaluative Sciences; ©2005 Canadian Institute for Health Information. Available from URL: http://secure.cihi.ca/cihiweb/en/downloads/Lit_Review2005_e.pdf (accessed April 2012).
Hopman WM, Towheed T, Anastassiades T, et al. Canadian normative data for the SF-36 health survey. Canadian Multicentre Osteoporosis Study Research Group. CMAJ 2000; 163: 265-71.
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61: 344-9.
Cleeland CS. Pain assessment in cancer. In: Osoba D, editor. Effect of Cancer on Quality of Life. Boca Raton: CRC Press; 1991 .
Mendoza TR, Chen C, Brugger A, et al. The utility and validity of the modified brief pain inventory in a multiple-dose postoperative analgesic trial. Clin J Pain 2004; 20: 357-62.
Statistics Canada. Canadian Community Health Survey (CCHS): Annual Component - 2010 Questionnaire. Ottawa: Statistics Canada; 2010. Available from URL: file:///C:/DOCUME~1/Carolyn/LOCALS~1/Temp/3226_D7_T9_V8-eng.htm (accessed April 2012).
Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain 1986; 27: 117-26.
Ware JE, Kosinski M, Dewey JE. How to Score Version 2 of the SF-36 Health Survey (standard and acute forms). Lincoln, RI: QualityMetric Incorporated; 2000 .
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement 1977; 1: 385-401.
Carr E, Brockbank K, Allen S, Strike P. Patterns and frequency of anxiety in women undergoing gynaecological surgery. J Clin Nurs 2006; 15: 341-52.
Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess 1995; 7: 524-32.
Jensen MP, Keefe FJ, Lefebvre JC, Romano JM, Turner JA. One- and two-item measures of pain beliefs and coping strategies. Pain 2003; 104: 453-69.
Kroenke K, Spitzer RL, deGruy FV III, Swindle R. A symptom checklist to screen for somatoform disorders in primary care. Psychosomatics 1998; 39: 263-72.
Cleeland CS, Ryan KM. Pain assessment: global use of the brief pain inventory. Ann Acad Med Singapore 1994; 23: 129-38.
Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U. Risk factors for long-term pain after hernia surgery. Ann Surg 2006; 244: 212-9.
Reitsma ML, Vandenkerkhof EG, Johnston SL, Hopman WM. Does health-related quality of life improve in women following gynaecological surgery? J Obstet Gynaecol Can 2011; 33: 1241-7.
Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC. Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 2001; 88: 1122-6.
Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 2005; 95: 69-76.
VanDenKerkhof EG, Peters ML, Bruce J. Chronic pain after surgery: time for standardization? A framework to establish core risk factor and outcome domains for epidemiological studies. Clin J Pain; in press.
Acknowledgements
We acknowledge the larger Canadian Institutes of Health Research (CIHR) investigative team for their contributions to the original study: Dr. Tanveer Towheed, Dr. Margaret Harrison, Dr. Miu Lam, and Dr. Patricia McGrath, as well as the research nurses, Debbie Shore and Elizabeth Orr and research associate James Medd. The original CIHR-funded CPSP study focused on gynecological surgery 5 and provided the methodological template for the abdominal surgery pilot study presented here.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Elizabeth VanDenKerkhof and Wilma Hopman contributed substantially to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data; drafting the article, and revising the article critically for important intellectual content. Rosemary Wilson contributed substantially to the conception and design of the manuscript. Paul Belliveau and Rosemary Wilson contributed substantially to the acquisition of data. Michelle Reitsma and David Goldstein also contributed to the acquisition of data. Michelle Reitsma contributed to the analysis of data. Paul Belliveau, Rosemary Wilson, and Ian Gilron contributed substantially to the interpretation of data. David Goldstein also contributed to the interpretation of data. Michelle Reitsma contributed to drafting the article. Paul Belliveau, Rosemary Wilson, and Ian Gilron contributed substantially to revising the article critically for important intellectual content. David Goldstein also contributed to revising the article critically for important intellectual content.
Rights and permissions
About this article
Cite this article
VanDenKerkhof, E.G., Hopman, W.M., Reitsma, M.L. et al. Chronic pain, healthcare utilization, and quality of life following gastrointestinal surgery. Can J Anesth/J Can Anesth 59, 670–680 (2012). https://doi.org/10.1007/s12630-012-9712-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-012-9712-x