Abstract
Background
Contemporary guidelines for managing PTC advise an approach wherein primary tumor and regional metastases (RM) are completely resected at first surgery and radioiodine remnant ablation (RRA) is restricted to high-risk patients, policies our group has long endorsed. To assess our therapeutic efficacy, we studied 190 children and 4242 adults consecutively treated during 1936–2015.
Subjects and methods
Mean follow-up durations for children and adults were 26.9 and 15.2 years, respectively. Bilateral lobar resection was performed in 86% of children and 88% of adults, followed by RRA in 30% of children and 29% of adults; neck nodes were excised in 86% of children and 66% of adults. Tumor recurrence (TR) and cause-specific mortality (CSM) details were taken from a computerized database.
Results
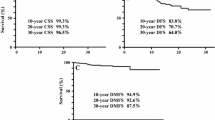
Children, when compared to adults, had larger primary tumors which more often were grossly invasive and incompletely resected. At presentation, children, as compared to adults, had more RM and distant metastases (DM). Thirty-year TR rates were no different in children than adults at any site. Thirty-year CSM rates were lower in children than adults (1.1 vs. 4.9%; p = 0.01). Comparing 1936–1975 (THEN) with 1976–2015 (NOW), 30-year CSM rates were similar in MACIS <6 children (p = 0.67) and adults (p = 0.08). However, MACIS <6 children and adults in 1976–2015 had significantly higher recurrence at local and regional, but not at distant, sites. MACIS 6+ adults, NOW, compared to THEN, had lower 30-year CSM rates (30 vs. 47%; p < 0.001), unassociated with decreased TR at any site.
Conclusions
Children, despite presenting with more extensive PTC when compared to adults, have postoperative recurrences at similar frequency, typically coexist with DM and die of PTC less often. Since 1976, both children and adults with MACIS <6 PTC have a <1% chance at 30 years of CSM; adults with higher MACIS scores (6 or more) have a 30-year CSM rate of 30%.













Similar content being viewed by others
References
Sitges-Serra A (2014) Low-risk papillary thyroid cancer: times are changing. Expert Rev Endocrinol Metab 9(1):9–18
Davies L, Morris LG, Haymart M et al (2015) AACE and ACE disease state clinical review: the increasing incidence of thyroid cancer. Endocr Pract 21(6):686–696
Vaccarella S, Franceschi S, Bray F et al (2016) Worldwide thyroid cancer epidemic? The increasing impact of overdiagnosis. N Engl J Med 375(7):614–617
Nixon IJ, Shah JP (2014) Well differentiated thyroid cancer: are we over treating our patients? EJSO 40:129–132
Hay ID, McConahey WM, Goellner JR (2002) Managing patients with papillary thyroid carcinoma: insights gained from the Mayo Clinic’s experience of treating 2,512 consecutive patients during 1940 through 2000. Trans Am Clin Climatol Assoc 113:241–260
Nixon IJ, Ganly I, Patel SG et al (2012) Changing trends in well differentiated thyroid carcinoma over eight decades. Int J Surg 10(10):618–623
Kiernan CM, Whiteside MA, Solorzano CC (2017) Cancer registries: can we improve the quality of thyroid cancer data? Ann Surg Oncol 24(5):1202–1207
Grant CS, Stulak JM, Thompson GB et al (2010) Risks and adequacy of an optimized surgical approach to the primary surgical management of papillary thyroid carcinoma treated during 1999–2006. World J Surg 34(6):1239–1246. doi:10.1007/s00268-009-0307-9
Onkendi EO, McKenzie TJ, Richards ML et al (2014) Reoperative experience with papillary thyroid cancer. World J Surg 38(3):645–652. doi:10.1007/s00268-013-2379-9
Zimmerman D, Hay ID, Gough IR et al (1988) Papillary thyroid carcinoma in children and adults: long-term follow-up of 1039 patients treated at one institution during three decades. Surgery 104:1157–1166
Hay ID, Gonzalez-Losada T, Reinalda MS et al (2010) Long-term outcome in 215 children and adolescents with papillary thyroid cancer treated during 1940 through 2008. World J Surg 34(6):1192–2002. doi:10.1007/s00268-009-0364-0
McConahey WM, Hay ID, Woolner LB et al (1986) Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy and outcome. Mayo Clin Proc 61:978–996
Hay ID (1990) Papillary thyroid carcinoma. Endo Metab Clin N Am 19(3):545–576
Hay ID, Thompson GB, Grant CS et al (2002) Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940–1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg 26:879–885. doi:10.1007/s00268-002-6612-1
Hay ID, Bergstralh EJ, Goellner JR et al (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1,779 patients surgically treated at one institution during 1940 through 1990. Surgery 114:1050–1058
Hay ID (2007) Management of patients with low-risk papillary thyroid carcinoma. Endocr Pract 13(3):521–533
Francis GL, Waguespack SG, Bauer AJ et al (2015) Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid 25(7):716–759
Haugen BR (2017) 2015 ATA management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer; what is new and what has changed? Cancer 123(3):372–381
Hay ID (2006) Selective use of radioactive iodine in the postoperative management of patients with papillary and follicular thyroid carcinoma. J Surg Oncol 94(8):692–700
Edge SB, Byrd DR, Compton CC et al (2010) AJCC cancer staging manual, 7th edn. Springer, New York, pp 67–74
Hay ID, Johnson TR, Thompson GB et al (2016) Minimal extrathyroidal extension in papillary thyroid carcinoma does not result in increased rates of either cause-specific mortality or postoperative tumor recurrence. Surgery 159(1):11–19
LiVolsi VA, Albores-Saavedra J, Asa SL (2004) Papillary thyroid carcinoma. In: DeLellis RA, Lloyd RV, Heitz PU, Eng C (eds) Pathology and genetics of tumours of endocrine organs: WHO classification of tumours. IARC Press, Lyon, pp 57–66
Grant CS (2015) Recurrence of papillary thyroid carcinoma after optimized surgery. Gland Surg 4:52–62
Carhill AA, Litofsky DR, Ross DS et al (2015) Long-term outcomes following therapy in differentiated thyroid carcinoma: NTCTCS registry analysis 1987–2012. J Clin Endocrinol Metab 100:3270–3279
Hay ID, Grant CS, Taylor WF et al (1987) Ipsilateral lobectomy versus bilateral lobar resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system. Surgery 102:1088–1094
Cady B (1997) Our AMES is true: how an old concept still hits the mark: or, risk group assignment points the arrow to rational therapy selection in differentiated thyroid cancer. Am J Surg 197:462–468
Cady B (1998) Papillary carcinoma of the thyroid gland: treatment based on risk group definition. Surg Clin N Am 7:633–644
Pemberton JJ (1928) Malignant disease of the thyroid gland: a clinical consideration. Ann Surg 87:369–377
Mazzaferri EL, Young RL, Oertel JE et al (1977) Papillary thyroid carcinoma: the impact of therapy in 576 patients. Medicine (Baltimore) 56:171–196
Lubitz CC, Kong CY, McMahon PM et al (2014) Annual financial impact of well-differentiated thyroid cancer care in the United States. Cancer 120:1345–1352
Cronan JJ (2008) Thyroid nodules; is it time to turn off the US machines? Radiology 247:602–604
Cady B (1978) Basic principles in surgical oncology. Presidential address. Arch Surgery 132:338–346
Porterfield JR, Cassivi SD, Wigle DA et al (2009) Thoracic metastatectomy for thyroid malignancies. Eur J Cardiothorac Surg 36:155–158
Lubitz CC, Sosa JA (2016) The changing landscape of papillary thyroid cancer: epidemiology, management, and the implications for patients. Cancer 122:3754–3759
Dominguez JM, Nilo F, Contreras T et al (2017) Neck sonography and suppressed thyroglobulin have high sensitivity for identifying persistent/recurrent disease with low-risk thyroid cancer treated with total thyroidectomy and radioactive iodine ablation, making stimulated thyroglobulin unnecessary. J Ultrasound Med. doi:10.1002/jum.14260 (Epub ahead of print)
Acknowledgements
The documentation from one institution of 70,000 patient-years of PTC experience has required the cooperation of many Mayo Clinic colleagues and the support of the lead author’s wife, Professor Eileen Hay. Dr. Hay is particularly indebted to the late Drs. McConahey, Taylor and Woolner for initiating the careful documentation of outcome in the 1946–1970 cohort of PTC patients. This present study was supported by generous financial contributions from the Dr. RF Emslander Professorship, Colin V. and Brenda Reed from Nashville, TN, and the William Stamps Farish Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hay, I.D., Johnson, T.R., Kaggal, S. et al. Papillary Thyroid Carcinoma (PTC) in Children and Adults: Comparison of Initial Presentation and Long-Term Postoperative Outcome in 4432 Patients Consecutively Treated at the Mayo Clinic During Eight Decades (1936–2015). World J Surg 42, 329–342 (2018). https://doi.org/10.1007/s00268-017-4279-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4279-x