Abstract
Background
Intense disease surveillance and frequent lymph node metastases (LNMs) in papillary thyroid cancer (PTC) have resulted in increased locoregional recurrences. We examined the safety and efficacy of an optimized surgical approach including preoperative ultrasonograpy (US), bilateral thyroidectomy, routine compartment VI dissection, and lateral neck dissection for LNM.
Methods
During 1999–2006, a total of 420 patients underwent optimized primary surgery; 291(69%) females, median age 46 years; follow-up 98%, median 4.4 years. Patients were reviewed for tumor characteristics, pattern of LNM, staging, and outcomes.
Results
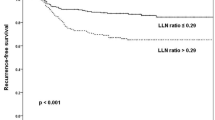
Total or near-total thyroidectomy was performed in 212 (51%) and 208 (49%) patients, respectively. Tumors were multicentric, 40% (average 1.7 cm); were bilateral, 30%; and showed extrathyroidal extension, 17%. Overall, 223 (53%) patients had LNMs: 213 (51%) were central and 85 (20%) were lateral jugular. pTNM staging: I, 258 (61%); II, 35 (8%); III, 88 (21%); IV, 39 (9%). AGES (age, grade, extension, and size—thyroid tumor; and MACIS (metastasis, age, completeness of resection, invasion, and size) prognostic scores were low risk in 362 (86%) and 352 (84%), respectively. Relapse developed in 57 (14%) patients: LNM in 44, soft tissue local recurrence (LR) in 5, distant metastases (DM) in 8. Hypoparathyroidism occurred in 5 (1.2%) patients and 1 had unintentional laryngeal nerve damage. Relapse with LNM occurred in previously operated fields in 19 (5%) patients, 11(3%) from disease virulence (LR or DM), preoperative false-negative (FN) US in 12 (3%), and combination of FN-US and recurrence in the operated field in 5 (1%) patients.
Conclusions
Recurrence was limited to 5% of patients when the extent of disease was accurately defined and potentially curable. This optimized surgical strategy is relatively safe.
Similar content being viewed by others
References
Hay ID, Grant CS, Taylor WF et al (1987) Ipsilateral lobectomy versus bilateral lobar resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system. Surgery 102:1088–1095
Hay I, Thompson G, Grant C et al (2002) Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940–1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg 26:879–885
Cady B, Rossi R (1988) An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery 104:947–953
American Thyroid Association Guidelines Task Force (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:1–33
Thyroid Carcinoma Task Force (2001) AACE/AAES medical/surgical guidelines for clinical practice: management of thyroid carcinoma—American Association of Clinical Endocrinologists, American College of Endocrinology. Endocr Pract 7:203–220
Bilimoria K, Bentrem D, Ko C et al (2007) Extent of surgery affects survival for papillary thyroid cancer. Ann Surg 246:275–384
Anonymous (2007) Thyroid carcinoma. In: NCCN clinical practice guidelines in oncology. 2.2007 ed. www.nccn.org
Greene F, Page D, Fleming I et al (2002) AJCC cancer staging manual, 6th edn. Springer, New York
Fleming I, Cooper J, Henson D (eds) (1997) American Joint Committee on cancer: AJCC cancer staging manual. Lippincott-Raven, Philadelphia
Hay ID, Bergstralh EJ, Goellner JR et al (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 114:1050–1058
DeGroot L, Kaplan E, McCormick M et al (1990) Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab 71:414–424
Moley J, Wells S (1999) Compartment-mediated dissection for papillary thyroid cancer. Langenbecks Arch Surg 384:9–15
Anonymous (2008) Differentiated thyroid cancer: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol 19:ii99–ii101
Zimmerman D, Hay I, Gough I et al (1988) Papillary thyroid cancer in children and adults: long-term follow-up of 1039 patients conservatively treated at one institution during three decades. Surgery 104:1157–1166
Vassilopoulou-Sellin R, Schultz P, Haynie T (1996) Clinical outcome of patients with papillary thyroid carcinoma who have recurrence after initial radioactive iodine therapy. Cancer 78:493–501
Mazzaferri E, Young R, Oertel J et al (1977) Papillary thyroid carcinoma: the impact of therapy in 576 patients. Medicine (Baltimore) 56:171–196
Lundgren C, Hall P, Dickman P et al (2005) Clinically significant prognostic factors for differentiated thyroid carcinoma. Cancer 106:524–531
Loh KC, Greenspan F, Gee L et al (1997) Pathological tumor-node-metastasis (pTNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. J Clin Endocrinol Metab 82:3553–3562
Gagel R, Goepfert H, Callender D (1996) Changing concepts in the pathogenesis and management of thyroid carcinoma. CA Cancer J Clin 46:261–283
Voutilainen P, Multanen M, Leppaniemi A et al (2001) Prognosis after lymph node recurrence in papillary thyroid carcinoma depends on age. Thyroid 11:953–957
Heemstra K, Liu Y, Stokkel M et al (2007) Serum thyroglobulin concentrations predict disease-free remission and death in differentiated thyroid carcinoma. Clin Endocrinol (Oxf) 66:58–64
Mazzaferri E (2007) Management of low-risk differentiated thyroid cancer. Endocr Pract 13:498–512
Kloos R, Mazzaferri E (2005) A single recombinant human thyrotropin-stimulated serum thyroglobulin measurement predicts differentiated thyroid carcinoma metastases three to five years later. J Clin Endocrinol Metab 90:5047–5057
Sawka A, Thephamongkhol K, Brouwers M et al (2004) A systematic review and metaanalysis of the effectiveness of radioactive iodine remnant ablation for well-differentiated thyroid cancer. J Clin Endocrinol Metab 89:3668–3676
Stulak J, Grant C, Farley D et al (2006) Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg 141:489–496
Sywak M, Cornford L, Roach P et al (2006) Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery 140:1000–1007
Bonnet S, Hartl D, Leboulleux S et al (2009) Prophylactic lymph node dissection for papillary thyroid cancer less than 2 cm: implications for radioiodine treatment. J Clin Endocrinol Metab 94:1162–1167
Noguchi S, Murakami N (1987) The value of lymph-node dissection in patients with differentiated thyroid cancer. Surg Clin North Am 67:251–261
Ozaki O, Kunihiko I, Kobayashi K et al (1988) Modified neck dissection for patients with nonadvanced, differentiated carcinoma of the thyroid. World J Surg 12:825–829
Hay I, Bergstralh E, Grant C et al (1999) Impact of primary surgery on outcome in 300 patients with pathologic tumor-node-metastasis stage III papillary thyroid carcinoma treated at one institution from 1940 through 1989. Surgery 126:1173
Roh JL, Park JY, Park C (2007) Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 245:604–610
Porterfield J, Factor D, Grant C (2009) Operative technique for modified radical neck dissection in papillary thyroid carcinoma. Arch Surg 144:567–574
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grant, C.S., Stulak, J.M., Thompson, G.B. et al. Risks and Adequacy of an Optimized Surgical Approach to the Primary Surgical Management of Papillary Thyroid Carcinoma Treated During 1999–2006. World J Surg 34, 1239–1246 (2010). https://doi.org/10.1007/s00268-009-0307-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0307-9