Abstract
Background
Some patients with persistent inguinodynia following a Lichtenstein hernia repair fail all non-surgical treatments. Characteristics of mesh-related pain are not well described whereas a meshectomy is controversial. Aims were to define mesh-related pain symptoms, to investigate long-term effects of a meshectomy and to provide recommendations on meshectomy.
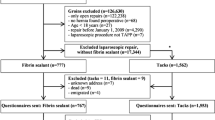
Methods
Consecutive patients undergoing open meshectomy with/without selective neurectomy for chronic inguinodynia following Lichtenstein repair were analysed including a follow-up questionnaire. Outcome measures were complications, satisfaction (excellent, good, moderate, poor) and hernia recurrence rate. Recommendations for meshectomy are proposed based on a literature review.
Results
Seventy-four patients (67 males, median age 56 years) underwent mesh removal (exclusively mesh, 26%; combined with tailored neurectomy, 74%) between June 2006 and March 2015 in a single centre. Complications were intraoperatively recognized small bowel injury (n = 1) and testicular atrophy (n = 2). A 64% excellent/good long-term result was attained (median 18 months). Success rates of a meshectomy (63%) or combined with a neurectomy (64%) were similar. Five hernia recurrences occurred during follow-up (7%). A patient with a pure mesh-related groin pain characteristically reports a ‘foreign body feeling’. Pain intensifies during hip flexion (car driving) and is attenuated following hip extension or supine position. Palpation is painful along the inguinal ligament whereas neuropathic characteristics (hyperpathic skin, trigger points) are lacking.
Conclusions
Mesh removal either or not combined with tailored neurectomy is beneficial in two of three patients with characteristics of mesh-related inguinodynia following Lichtenstein hernia repair who are refractory to alternative pain treatments.




Similar content being viewed by others
References
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194(3):394–400
Classification of Chronic Pain (1986) Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the international association for the study of pain, subcommittee on Taxonomy. Pain Suppl 3:S1–S226
Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19(1):48–54
Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244(2):212–219
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13(4):343–403
Loos MJ, Scheltinga MR, Roumen RM (2010) Tailored neurectomy for treatment of postherniorrhaphy inguinal neuralgia. Surgery 147(2):275–281
Aasvang EK, Kehlet H (2009) The effect of mesh removal and selective neurectomy on persistent postherniotomy pain. Ann Surg 249(2):327–334
Campanelli G, Bertocchi V, Cavalli M, Bombini G, Biondi A, Tentorio T, Sfeclan C, Canziani M (2013) Surgical treatment of chronic pain after inguinal hernia repair. Hernia 17(3):347–353
Bischoff JM, Enghuus C, Werner MU, Kehlet H (2013) Long-term follow-up after mesh removal and selective neurectomy for persistent inguinal postherniorrhaphy pain. Hernia 17(3):339–345
Valvekens E, Nijs Y, Miserez M (2015) Long-term outcome of surgical treatment of chronic postoperative groin pain: a word of caution. Hernia 19(4):587–594
Amid PK (2004) Radiologic images of meshoma: a new phenomenon causing chronic pain after prosthetic repair of abdominal wall hernias. Arch Surg 139(12):1297–1298
Lange JF, Kaufmann R, Wijsmuller AR, Pierie JP, Ploeg RJ, Chen DC, Amid PK (2014) An international consensus algorithm for management of chronic postoperative inguinal pain. Hernia 19(1):33–43
Arlt GD, Lamm T, Klosterhalfen B (2003) Mesh removal in inguinal hernia repair. Eur Surg 35(1):42–44
Madura JA, Madura JA 2nd, Copper CM, Worth RM (2005) Inguinal neurectomy for inguinal nerve entrapment: an experience with 100 patients. Am J Surg 189(3):283–287
Amid PK, Chen DC (2011) Surgical treatment of chronic groin and testicular pain after laparoscopic and open preperitoneal inguinal hernia repair. J Am Coll Surg 213(4):531–536
Delikoukos S, Fafoulakis F, Christodoulidis G, Theodoropoulos T, Hatzitheofilou C (2008) Re-operation due to severe late-onset persisting groin pain following anterior inguinal hernia repair with mesh. Hernia 12(6):593–595
Vuilleumier H, Hubner M, Demartines N (2009) Neuropathy after herniorrhaphy: indication for surgical treatment and outcome. World J Surg 33(4):841–845. doi:10.1007/s00268-008-9869-1
Zacest AC, Magill ST, Anderson VC, Burchiel KJ (2010) Long-term outcome following ilioinguinal neurectomy for chronic pain. J Neurosurg 112(4):784–789
Koopmann MC, Yamane BH, Starling JR (2011) Long-term follow-up after meshectomy with acellular human dermis repair for postherniorrhaphy inguinodynia. Arch Surg 146(4):427–431
Heise CP, Starling JR (1998) Mesh inguinodynia: a new clinical syndrome after inguinal herniorrhaphy? J Am Coll Surg 187(5):514–518
Aasvang EK, Jensen KE, Fiirgaard B, Kehlet H (2009) MRI and pathology in persistent postherniotomy pain. J Am Coll Surg 208(6):1023–1028 (discussion 1028–1029)
Rosen MJ, Novitsky YW, Cobb WS, Kercher KW, Heniford BT (2006) Combined open and laparoscopic approach to chronic pain following open inguinal hernia repair. Hernia 10(1):20–24
Keller JE, Stefanidis D, Dolce CJ, Iannitti DA, Kercher KW, Heniford BT (2008) Combined open and laparoscopic approach to chronic pain after inguinal hernia repair. Am Surg 74(8):695–700 (discussion 700–701)
Magnusson N, Gunnarsson U, Nordin P, Smedberg S, Hedberg M, Sandblom G (2015) Reoperation for persistent pain after groin hernia surgery: a population-based study. Hernia 19(1):45–51
Dirksen CD, Beets GL, Go PM, Geisler FE, Baeten CG, Kootstra G (1998) Bassini repair compared with laparoscopic repair for primary inguinal hernia: a randomised controlled trial. Eur J Surg 164(6):439–447
Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR, Di Miceli D, Doglietto GB (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15(3):239–249
Voorbrood CE, Burgmans JP, Van Dalen T, Breel J, Clevers GJ, Wille F, Simmermacher RK (2015) An algorithm for assessment and treatment of postherniorrhaphy pain. Hernia 19(4):571–577
Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, Fortelny R, Heikkinen T, Jorgensen LN, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Simons MP (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18(2):151–163
Kouhia S, Silvasti S, Kainulainen J, Hakala T, Paajanen H (2015) Magnetic resonance imaging has no role in diagnosing the origin of pain in patients with overwhelmingly painful inguinal hernia. Hernia 19(4):557–563
Zwaans WA, Verhagen T, Roumen RM, Scheltinga MR (2015) Factors determining outcome after surgery for chronic groin pain following a Lichtenstein hernia repair. World J Surg 39(11):2652–2662. doi:10.1007/s00268-015-3183-5
Baron R (2006) Mechanisms of disease: neuropathic pain—a clinical perspective. Nat Clin Pract Neurol 2(2):95–106
Loos MJ, Roumen RM, Scheltinga MR (2007) Classifying post-herniorrhaphy pain syndromes following elective inguinal hernia repair. World J Surg 31(9):1760–1765. doi:10.1007/s00268-007-9121-4 (discussion 1766–1767)
Acknowledgements
The authors thank Dr. J.P. Dieleman for her support and expertise regarding statistical analysis. We thank authors who responded to our e-mail and provided detailed data on their studies: Prof. H. Kehlet, Dr. C. Heise, Dr. J. Starling, Dr. E. Valvekens, Dr. G. Sandblom and Prof. G. Campanelli.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declares that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zwaans, W.A.R., Perquin, C.W., Loos, M.J.A. et al. Mesh Removal and Selective Neurectomy for Persistent Groin Pain Following Lichtenstein Repair. World J Surg 41, 701–712 (2017). https://doi.org/10.1007/s00268-016-3780-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3780-y