Abstract
Background
Some patients develop chronic groin pain after a Lichtenstein hernia repair. Previous studies have demonstrated beneficial effects of removal of entrapped inguinal nerves or a meshectomy in patients with chronic pain after open inguinal hernia mesh repair. Factors determining success following this remedial surgery are unknown. The aim of the study was to identify potential patient- or surgery-related factors predicting the surgical efficacy for inguinodynia following Lichtenstein repair.
Methods
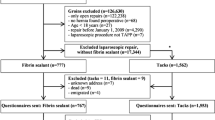
Consecutive adult patients with a history of persistent pain following Lichtenstein repair who underwent remedial surgery were analysed using univariate analysis. Significant confounders (p < 0.05) were combined in a multivariate logistic regression model using a backward stepwise regression method.
Results
A total of 136 groin pain operations were available for analysis. Factors contributing to success were removal of a meshoma (OR 4.66) or a neuroma (OR 5.60) and the use of spinal anaesthesia (OR 4.38). In contrast, female gender (OR 0.30) and preoperative opioid use (OR 0.38) were significantly associated with a less favourable outcome. Using a multivariate analysis model, surgery under spinal anaesthesia (OR 4.04), preoperative use of opioids (OR 0.37), and meshoma removal (OR 5.31) greatly determined surgical outcome.
Conclusions
Pain reduction after remedial surgery for chronic groin pain after Lichtenstein repair is more successful if surgery is performed under spinal anaesthesia compared to general anaesthesia. Removal of a meshoma must be considered as success rates are optimized following these measures. Patients using opioids preoperatively have less favourable outcomes.

Similar content being viewed by others
Abbreviations
- MMC:
-
Máxima Medical Centre
- NRS:
-
Numerical rating scale
- PROM:
-
Patient-related outcome measures
- OR:
-
Odds ratio
- 95 % CI:
-
95 % confidence interval
- SD:
-
Standard deviation
- ASA:
-
American Society of Anaesthesiologists
References
Nienhuijs S, Staal E, Strobbe L et al (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194(3):394–400
Vuilleumier H, Hubner M, Demartines N (2009) Neuropathy after herniorrhaphy: indication for surgical treatment and outcome. World J Surg 33(4):841–845. doi:10.1007/s00268-008-9869-1
Ferzli GS, Edwards E, Al-Khoury G, Hardin R (2008) Postherniorrhaphy groin pain and how to avoid it. Surg Clin North Am 88(1):203–216 x–xi
O’Dwyer PJ, Alani A, McConnachie A (2005) Groin hernia repair: postherniorrhaphy pain. World J Surg 29(8):1062–1065. doi:10.1007/s10029-015-1347-8
Wijsmuller AR, Lange JF, van Geldere D et al (2007) Surgical techniques preventing chronic pain after Lichtenstein hernia repair: state-of-the-art vs daily practice in the Netherlands. Hernia 11(2):147–151
Loos MJ, Scheltinga MR, Roumen RM (2010) Tailored neurectomy for treatment of postherniorrhaphy inguinal neuralgia. Surgery 147(2):275–281
Amid PK (2004) Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia 8(4):343–349
Kim DH, Murovic JA, Tiel RL, Kline DG (2005) Surgical management of 33 ilioinguinal and iliohypogastric neuralgias at Louisiana State University Health Sciences Center. Neurosurgery 56(5):1013–1020 discussion 1013–20
Aasvang EK, Kehlet H (2009) The effect of mesh removal and selective neurectomy on persistent postherniotomy pain. Ann Surg 249(2):327–334
Amid PK (2002) A 1-stage surgical treatment for postherniorrhaphy neuropathic pain: triple neurectomy and proximal end implantation without mobilization of the cord. Arch Surg 137(1):100–104
Chen DC, Hiatt JR, Amid PK (2013) Operative management of refractory neuropathic inguinodynia by a laparoscopic retroperitoneal approach. JAMA Surg 148(10):962–967
Bischoff JM, Enghuus C, Werner MU, Kehlet H (2013) Long-term follow-up after mesh removal and selective neurectomy for persistent inguinal postherniorrhaphy pain. Hernia 17(3):339–345
Heise CP, Starling JR (1998) Mesh inguinodynia: a new clinical syndrome after inguinal herniorrhaphy? J Am Coll Surg 187(5):514–518
Zwaans WA, Perquin CW, Roumen RM, Scheltinga MR (2015) Mesh removal and selective neurectomy for persistent groin pain following Lichtenstein repair (submitted)
Aasvang EK, Gmaehle E, Hansen JB et al (2010) Predictive risk factors for persistent postherniotomy pain. Anesthesiology 112(4):957–969
Campanelli G, Bertocchi V, Cavalli M et al (2013) Surgical treatment of chronic pain after inguinal hernia repair. Hernia 17(3):347–353
Franneby U, Sandblom G, Nordin P et al (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244(2):212–219
van Assen T, Boelens OB, van Eerten PV et al (2014) Surgical options after a failed neurectomy in anterior cutaneous nerve entrapment syndrome. World J Surg 38(12):3105–3111. doi:10.1007/s00268-014-2737-2
Lange JFM, Kaufmann R, Wijsmuller AR et al (2015) An international consensus algorithm for management of chronic postoperative inguinal pain. Hernia 19(1):33–43
Amid PK (2004) Radiologic images of meshoma: a new phenomenon causing chronic pain after prosthetic repair of abdominal wall hernias. Arch Surg 139(12):1297–1298
Keller JE, Stefanidis D, Dolce CJ et al (2008) Combined open and laparoscopic approach to chronic pain after inguinal hernia repair. Am Surg 74(8):695–700 discussion 700–1
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233(1):1–7
Steegers MA, Wilder-Smith OH (2009) Late chronic pain after surgery is prevented with good perioperative analgesics. Ned Tijdschr Geneeskd 153(12):562–566
Ozgun H, Kurt MN, Kurt I, Cevikel MH (2002) Comparison of local, spinal, and general anaesthesia for inguinal herniorrhaphy. Eur J Surg 168(8–9):455–459
Tverskoy M, Cozacov C, Ayache M et al (1990) Postoperative pain after inguinal herniorrhaphy with different types of anesthesia. Anesth Analg 70(1):29–35
Kitahata LM (1993) Pain pathways and transmission. Yale J Biol Med 66(5):437–442
Woolf CJ (1983) Evidence for a central component of post-injury pain hypersensitivity. Nature 306(5944):686–688
Sugimoto T, Takemura M, Sakai A, Ishimaru M (1987) Rapid transneuronal destruction following peripheral nerve transection in the medullary dorsal horn is enhanced by strychnine, picrotoxin and bicuculline. Pain 30(3):385–393
Dworkin RH, O’Connor AB, Audette J et al (2010) Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 85(3 Suppl):S3–S14
Eisenberg E, McNicol E, Carr DB (2006) Opioids for neuropathic pain. Cochrane Database Syst Rev 19(3):CD006146
Lee SH, Cho SY, Lee HG et al (2013) Tramadol induced paradoxical hyperalgesia. Pain Phys 16(1):41–44
Ducic I, Dellon AL (2004) Testicular pain after inguinal hernia repair: an approach to resection of the genital branch of genitofemoral nerve. J Am Coll Surg 198(2):181–184
Aasvang E, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95(1):69–76
Kalliomaki ML, Meyerson J, Gunnarsson U et al (2008) Long-term pain after inguinal hernia repair in a population-based cohort; risk factors and interference with daily activities. Eur J Pain 12(2):214–225
Bischoff JM (2014) Management of persistent inguinal postherniorrhaphy pain: pharmacological and surgical aspects. Multidisciplinary pain center and section for surgical pathophysiology, rigshospitalet. University of Copenhagen, Copenhagen
Sondenaa K, Nesvik I, Breivik K, Korner H (2001) Long-term follow-up of 1059 consecutive primary and recurrent inguinal hernias in a teaching hospital. Eur J Surg 167(2):125–129
Massaron S, Bona S, Fumagalli U et al (2007) Analysis of post-surgical pain after inguinal hernia repair: a prospective study of 1,440 operations. Hernia 11(6):517–525
Liem MS, van Duyn EB, van der Graaf Y et al (2003) Recurrences after conventional anterior and laparoscopic inguinal hernia repair: a randomized comparison. Ann Surg 237(1):136–141
Sedgwick, P (2012) What is recall bias?. BMJ 344:e3519
Delgado-Rodriguez M, Llorca J (2004) Bias. J Epidemiol Community Health 58(8):635–641
Acknowledgments
We would like to thank Dr. J.P. Dieleman (epidemiologist) for her contribution to the statistical analyses performed in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Financial disclosure
None declared.
Rights and permissions
About this article
Cite this article
Zwaans, W.A.R., Verhagen, T., Roumen, R.M.H. et al. Factors Determining Outcome After Surgery for Chronic Groin Pain Following a Lichtenstein Hernia Repair. World J Surg 39, 2652–2662 (2015). https://doi.org/10.1007/s00268-015-3183-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3183-5