Abstract
Introduction
Laparoscopic surgery is the treatment of choice for repair of large hiatus hernia, but can be followed by recurrence. Repair with prosthetic mesh has been recommended to prevent recurrence, although complications following mesh repair have generated disagreement about whether or not mesh should be used. The early objective and clinical results of a randomized trial of repair with mesh versus sutures have been reported, and revealed few differences. In the current study, we evaluated quality of life outcomes within this trial at follow-up to 2 years.
Methods
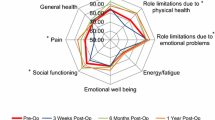
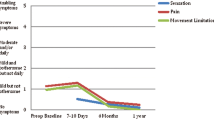
In a multicenter prospective double-blind randomized trial three methods for repair of large hiatus hernia were compared: sutures versus repair with absorbable mesh (Surgisis) versus non-absorbable (Timesh). Quality of life assessment using the Short-Form 36 (SF-36) questionnaire was undertaken at 3, 6, 12 and 24 months after surgery. SF-36 outcomes (8 individual scales and 2 composite scales) were determined for each group, and compared between groups, and across different follow-up points.
Results
126 patients were enrolled—43 sutures, 41 absorbable mesh and 42 non-absorbable mesh. 115 (91.3 %) completed a preoperative questionnaire, and 113 (89.7 %) completed the post-operative questionnaire at 3 months, 116 (92.1 %) at 6 months, 114 (90.5 %) at 12 months, and 91 (72.2 %) at 24 months. The SF-36 Physical and Mental Component Scores (PCS and MCS) improved significantly following surgery, and this improvement was sustained across 24 months follow-up (p < 0.001 for PCS and MCS at each follow-up point). There were no significant differences between the groups for the component scores or the eight SF-36 subscale scores at each follow-up time. 29 individuals had a recurrence at 6 months follow-up, of which 9 were symptomatic. The PCS were higher in patients with recurrence versus without (p < 0.01), and in patients with a symptomatic recurrence versus asymptomatic recurrence versus no recurrence (p = 0.001).
Conclusion
SF-36 measured quality of life improved significantly after repair of large hiatal hernia at up to 2 years follow-up, and there were no differences in outcome for the different repair techniques. The use of mesh versus no mesh in repair of large hiatal hernia did not influence quality of life.











Similar content being viewed by others
References
Watson DI, Davies N, Devitt PG, Jamieson GG (1999) Importance of dissection of the hernial sac in laparoscopic surgery for large hiatal hernias. Arch Surg 134:1069–1073
Andujar JJ, Papasavas PK, Birdas T et al (2004) Laparoscopic repair of large paraesophageal hernia is associated with a low incidence of recurrence and reoperation. Surg Endosc 18:444–447
Wijnhoven BP, Watson DI (2008) Laparoscopic repair of a giant hiatus hernia—how I do it. J Gastrointest Surg 12:1459–1464
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA et al (2000) Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg 190:553–560
Smith GS, Isaacson JR, Draganic BD, Baladas HG, Falk GL (2004) Symptomatic and radiological follow-up after para-esophageal hernia repair. Dis Esophagus 17:279–284
Aly A, Munt J, Jamieson GG, Ludemann R, Devitt PG, Watson DI (2005) Laparoscopic repair of large hiatal hernias. Br J Surg 92:648–653
Carlson MA, Richards CG, Frantzides CT (1999) Laparoscopic prosthetic reinforcement of hiatal herniorrhaphy. Dig Surg 16:407–410
Granderath FA, Carlson MA, Champion JK, Szold A, Basso N, Pointner R et al (2006) Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc 20:367–379
Furnee E, Hazebroek E (2013) Mesh in laparoscopic large hiatal hernia repair: a systematic review of the literature. Surg Endosc 27:3998–4008
Hazebroek EJ, Leibman S, Smith GS (2009) Erosion of a composite PTFE/ePTFE mesh after hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 19:175–177
Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ Jr, Michael Brunt L, Hunter JG et al (2009) Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc 23:1219–1226
Oelschlager BK, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B et al (2006) Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244:481–490
Frantzides CT, Madan AK, Carlson MA, Stavropoulos GP (2002) A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair vs simple cruroplasty for large hiatal hernia. Arch Surg 137:649–652
Oelschlager BK, Pellegrini CA, Hunter JG et al (2011) Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 213:461–468
Watson DI, Thompson SK, Devitt PG et al (2015) Laparoscopic repair of very large hiatus hernia with sutures vs. absorbable vs. non-absorbable mesh—a randomized controlled trial. Ann Surg 261:282–289
Kamolz T, Pointner R, Velanovich V (2003) The impact of gastroesophageal reflux disease on quality of life. Surg Endosc 17:1193–1199
Kaplan-Machlis B, Spiegler GE, Revicki DA (1999) Health-related quality of life in primary care patients with gastroesophageal reflux disease. Ann Pharmacother 33:1032–1036
Revicki DA, Wood M, Maton PN, Sorensen S (1998) The impact of gastroesophageal reflux disease on health-related quality of life. Am J Med 104:252–258
Kamolz T, Wykypiel H Jr, Bammer T, Pointner R (1998) Quality of life after laparoscopic antireflux surgery-Nissen fundoplication. Chirurg 69:947–950
Granderath FA, Kamolz T, Schweiger UM, Pointner R (2002) Quality of life, surgical outcome, and patient satisfaction three years after laparoscopic Nissen fundoplication. World J Surg 26:1234–1238. doi:10.1007/s00268-002-6416-3
Ware JE Jr (1992) Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Woodcock SA, Watson DI, Lally C, Archer S, Bessell JR, Booth M et al (2006) Quality of life following laparoscopic anterior 90 degrees versus Nissen fundoplication: results from a multicenter randomized trial. World J Surg 30:1856–1863.doi:10.1007/s00268-005-0623-7
Granderath FA, Schweiger UM, Kamolz T et al (2005) Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg 140:40–48
Kamolz T, Granderath F, Pointner R (2003) Laparoscopic antireflux surgery: disease-related quality of life assessment before and after surgery in GERD patients with and without Barrett’s esophagus. Surg Endosc 17:880–885
Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T et al (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Ware JE Jr., Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A (1995) Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care 33(4 Suppl):AS264–AS279
Acknowledgments
This randomized trial was supported by Research Project Grants from the National Health and Medical Research Council (NHMRC) of Australia—Grant numbers 375111 and 1022722. We are grateful for the assistance of Ms Lorelle Smith, Ms Nicky Carney and Ms Lorraine Sheehan-Hennessy who contributed to data collection, and Drs Susan Gan and Philip Game who helped with enrolment of patients into the randomized trial. This trial is registered with the Australia and New Zealand Clinical Trials Registry ACTRN12605000725662.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koetje, J.H., Irvine, T., Thompson, S.K. et al. Quality of Life Following Repair of Large Hiatal Hernia is Improved but not Influenced by Use of Mesh: Results From a Randomized Controlled Trial. World J Surg 39, 1465–1473 (2015). https://doi.org/10.1007/s00268-015-2970-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-2970-3