Abstract
Background
The Pietermaritzburg Metropolitan Trauma Service (PMTS) attempts to provide care for a whole city and hence is referred to as a service rather than a center. As part of a multifaceted quality improvement program, the PMTS has developed and implemented a robust electronic surgical registry (ESR). This review of the first year’s data from the ESR forms part of a situational analysis to assess the burden of trauma managed by the service and the quality of care delivered within the constraints of the available resources.
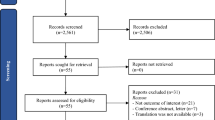
Methods
Formal ethical approval was obtained prior to design and development of this study, and appropriate commercial software was sourced. The exercise of data capture was integrated into the process of service delivery and was accomplished at the endpoint of patient care. 12 months after implementation of the registry, the data were extracted and audited.
Results
A total of 2,733 patients were admitted over the 12 month study period. The average patient age was 28.3 years. There were 2,255 (82.5 %) male patients and 478 (17.5 %) female patients. The average monthly admission rate was 228 patients, with a peak of 354 admissions over the December period. The mean injury severity score (ISS) was 12 [interquartile range (IQR) 6.7–23.2]. A quarter (24.8 %) of all new emergency admissions had an ISS > 15. The average duration of stay for patients was 5.12 days (IQR 2.3–13.2 days). Some 2,432 (92.1 %) patients survived, and 208 (7.9 %) died. A total of 333 (13 %) patients required admission to either the intensive care unit (ICU) or the high dependency unit. From the city mortuary data a further 362 deaths were identified. These included 290 deaths that occurred on scene and 72 that occurred within Pietermaritzburg hospitals other than Greys and Edendale. The total trauma-related mortality for the entire city in 2012 was 570 (51 % on-scene deaths and 49 % in-hospital deaths). Blunt trauma accounted for 62 % of deaths.
Conclusions
The PMTS treats a significant volume and spectrum of trauma. Despite significant resource limitations, we have managed to implement a functional and sustainable trauma service across multiple hospitals. We believe the major resource deficits limiting our service could be ameliorated by the development of an additional trauma facility, adequately equipped with dedicated trauma operating slates and trauma ICU beds. The adoption of our current model of trauma care came out of a need to work within our resource constraints, and it differs from the traditional model. Within the aforementioned limits, our data suggest that this model of delivering care is feasible, practical, and successful. Considering the universal burden of trauma and the all-too-common imbalance between resource demand and supply among many health-care institutions, it is our hope that this report will contribute to the ongoing academic debate around the topic of optimal systems of providing global trauma care.


Similar content being viewed by others
References
Muckart DJ (1991) Trauma—the malignant epidemic. S Afr Med J 79:93–95
Clarke DL, Thomson SR, Madiba TE et al (2005) Selective conservatism in trauma management: a South Africa contribution. World J Surg 29:962–965. doi:10.1007/s00268-005-0131-9
Bowley DM, Khavandi A, Boffard KD et al (2002) The malignant epidemic—changing patterns of trauma. S Afr Med J 92:798–802
Goosen J, Veller M (2008) Trauma and emergency surgery: South African model. World J Surg 32:1622–1625. doi:10.1007/s00268-008-9573-1
Mock C, Joshipura M, Goosen J et al (2006) Overview of the essential trauma care project. World J Surg 30:919–929. doi:10.1007/s00268-005-0764-8
Mock C, Joshipura M, Goosen J et al (2005) Strengthening trauma systems globally: the essential trauma care project. J Trauma 59:1243–1246
Joshipura M, Mock C, Goosen J et al (2004) Essential trauma care: strengthening trauma systems around the world. Injury 35:841–845
Mock C, Joshipura M, Goosen J (2004) Global strengthening of care for the injured. Bull World Health Organ 82:241
Hardcastle TC, Steyn E, Boffard K, Trauma Society of South Africa et al (2011) Guidelines for the assessment of trauma centers for South Africa. S Afr Med J 101:189–194
Hardcastle TC, Finlayson M, van Heerden M et al (2012) The prehospital burden of disease due to trauma in Kwa-Zulu Natal: the need for afrocentric trauma systems. World J Surg 37:1513–1525. doi:10.1007/s00268-012-1852-1
Nwomeh BC, Lowell W, Kable R et al (2006) History and development of trauma registry: lessons from developed to developing countries. World J Emerg Surg 1:32
O’Reilly GM, Cameron PA, Joshipura M (2012) Global trauma registry mapping: a scoping review. Injury 43:1148–1153
Juillard CJ, Mock C, Goosen J et al (2009) Establishing the evidence for trauma quality improvement: a collaborative WHO-IATSIC review. World J Surg 33:1075–1086. doi:10.1007/s00268-009-9959-8
Laing GL, Bruce JL, Aldous C et al (2014) The design, construction and implementation of a computerized trauma registry in a developing South African metropolitan trauma service. Injury 45:3–8
Clarke DL, Quazi MA, Reddy K et al (2011) Emergency operation for penetrating thoracic trauma in a metropolitan surgical service in South Africa. J Thorac Cardiovasc Surg 142:563–568
Howes N, Walker T, Allorto NL et al (2012) Laparotomy for blunt abdominal trauma in a civilian trauma service. S Afr J Surg 50:30–32
Alexander T, Fuller G, Hargovan P et al (2009) An audit of the quality of care of traumatic brain injury at a busy regional hospital in South Africa. S Afr J Surg 47(120–122):124–126
Kong VY, Bulajic B, Allorto NL et al (2012) Acute appendicitis in a developing country. World J Surg 36:2068–2073. doi:10.1007/s00268-012-1626-9
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laing, G.L., Skinner, D.L., Bruce, J.L. et al. Understanding the Burden and Outcome of Trauma Care Drives a New Trauma Systems Model. World J Surg 38, 1699–1706 (2014). https://doi.org/10.1007/s00268-014-2448-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2448-8