Abstract
Background
This study was designed to evaluate the outcomes of pancreaticoduodenectomy (PD) at a low-volume specialised Hepato Pancreato Biliary (HPB) unit. Volume outcome analyses show significantly better results for patients undergoing PD at high-volume centres (Begg et al. JAMA 280:1747–1751, 1998; Finlayson et al. Arch Surg 138:721–725, 2003; Birkmeyer et al. N Engl J Med 346:1128–1137, 2002; Gouma et al. Ann Surg 232:786–795, 2000). Centralisation of PD seems to be the logical conclusion to be drawn from these results. In countries like Australia with a small and widely dispersed population, centralisation may not be always feasible. Alternative strategy would be to have similar systems in place to those in high-volume centres to achieve similar results at low-volume centres. Many Australian tertiary care centres perform low to medium volumes of PD (Chen et al. HPB 12:101–108, 2010; Kwok et al. ANZ J Surg 80:605–608, 2010; Barnett and Collier ANZ J Surg 76:563–568, 2006; Samra et al. Hepatobiliary Pancreat Dis Int 10:415–421, 2011). Most of these have a specialised HPB unit, accredited by the Australia and New Zealand Hepatic pancreatic and biliary association (ANZHPBA), as training units for post fellowship training in HPB surgery. It is imperative to perform outcome-based analyses in these units to ensure safety and high quality of care.
Methods
Retrospective analysis of database for periampullary carcinoma (1998 till date) was performed in an ANZHPBA accredited HPB unit based at a tertiary care teaching hospital in South Australia. Because age older than 74 years is shown to be a predictive marker of increased morbidity and mortality after a PD, we analysed the outcomes in this subset of patients separately.
Results
Fifty-three patients underwent PD in 14 years. Overall mortality was 3.8 %. The last in hospital mortality was in 1999. The morbidity rates and the oncologic outcomes were similar to those in high-volume units.
Conclusions
PD can be safely performed in a low-volume specialised unit at centres where the amenities and processes at high-volume centres can be replicated.
Similar content being viewed by others
Introduction
Analytical studies performed on administrative databases have demonstrated significantly better outcomes of complex surgical procedures, such as pancreaticoduodenectomy (PD) when performed at high-volume centres [2, 3]. A policy of centralising complex surgeries to high-volume centres using volume as marker of quality has logically emerged based on these results [9, 10].
Age ≥74 years is shown to be an independent risk factor for predicting increased morbidity and mortality associated with PD [11] in an analysis by National Surgical Quality Improvement Program (NSQIP) of the American College of Surgeons. This is included in the NSQIP predictive “risk calculator” for PD.
In Australia, the incidence of pancreatic and periampullary cancers is similar to United States and Europe [12]. Australia has a much smaller and widely dispersed population. This has led to the unique situation of low-volume tertiary care facilities for PD in Australia. Pancreatic cancer is strongly age-dependent and with increasing longevity; increasingly older patients present for treatment of pancreatic cancer [12].
The tertiary institutes with specialist Hepato Pancreato Biliary (HPB) units in Australia are equipped with high-quality infrastructure and sound surgical expertise. Excellent anaesthetic, nursing, intensive care, interventional radiology, and gastroenterology services are readily available. Many other complex surgeries, such as liver resections, complex biliary surgeries, etc., are performed in high volumes at these institutes.
A unique opportunity therefore exists to assess if the results of PD in such low-volume specialised HPB units replicate those from high-volume centres.
Materials and methods
A prospective database for all PDs has been maintained at our institution since 2003. Data were retrospectively collected from 1998 to 2003. Demographic details, postoperative morbidity, and in-hospital mortality was recorded. Oncologic outcomes, including TNM staging, resection margins, number of lymph nodes harvested, along with perineural and vascular invasion were noted.
Overall morbidity, mortality, oncological outcomes, and survival were analysed. Subgroup analysis was performed for these outcomes for patients aged 74 years or older.
Statistical analysis
Descriptive statistics was analysed with SPSS 20 software. Fisher’s exact test with cross-tabulations was performed to provide a p value for all categorical variables to compare outcomes between patients less than (group A) and more than 74 years (group B) of age. For continuous variables, a t test was used.
Survival in months and status at last follow-up were used to compute Kaplan–Meier survival curves for both groups. A Cox proportional hazard model with age group as predictor was performed to evaluate difference between the two age groups.
Poisson regression was performed on count variables. Two variables with underdispersion (days on ventilator and days in ICU) were analysed using Poisson regression with robust error variance. Three variables with overdispersion (hospital stay, nodes, and number of positive nodes) were analysed with negative binomial regression.
Patients and procedure
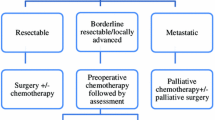
All patients presenting with periampullary and pancreatic head tumours who underwent a PD were included. Patients were primarily assessed by surgeons. Staging investigations included routine blood tests, tumour markers (CA19-9), and CT scan of the chest, abdomen, and pelvis. Endoscopic ultrasound was performed where indicated. All cases were discussed in a multidisciplinary (MDT) meeting to formulate a management plan. The MDT consulting panel included surgeons with HPB expertise, gastroenterologists, diagnostic and interventional radiologists, oncologists, as well as pathologists. Anaesthetic and intensive care unit (ICU) opinion was sought preoperatively where indicated to aid decision making. All surgeries were performed by two qualified surgeons (consultant surgeon and fellow or two consultants).The surgical procedure was standardised [13]. A classical PD was performed in most cases. Resection of portal vein and primary reconstruction was the procedure of choice where needed. Vascular surgery expertise was readily available if required.
A Roux-en-Y reconstruction with a two-layered “duct to mucosa” pancreaticojejunostomy was performed. Hepaticojejunostomy was performed as a single-layer interrupted anastomosis. The gastroenterostomy was either handsewn or stapled. All patients were electively treated in ICU/high-dependency units (HDU) in the immediate postoperative period.
Patient demographics, intraoperative surgical and anaesthetic data, postoperative morbidity and mortality, as well as overall survival were recorded in the database. All histopathology reports were reviewed.
Pancreatic leak and fistula was defined according to the International study group in pancreatic fistula (ISGPF) definition [14]. Subgroup analysis was performed in patients aged older than 74 years. Outcomes in this group were compared with those in younger patients (age <74).
Results
A total of 61 patients underwent a laparotomy with intent of curative resection. Disseminated peritoneal disease (n = 3, confirmed on frozen section) and superior mesenteric/mesocolic arterial involvement (n = 5) rendered eight patients unresectable. These patients underwent palliative bypass procedures. PD was performed in 53 patients.
Demographics
There were 31 males and 22 females. Thirty-four (64.15 %) were aged younger than 74 years and 19 (35.85 %) were aged older than 74 years (Table 1). The median age was 71 (range 49–83) years for the entire cohort. The common presenting symptoms were painless obstructive jaundice (92 %), weight loss (20 %), and abdominal pain (12 %).
Perioperative indicators
Overall operating time ranged between 253 and 1,104 min (mean 408, median 398). Median blood loss was 1,000 (range 300–3,800) ml. Partial excision of portal vein with primary reconstruction was performed in four cases. No intraoperative adverse event was noted. The average number of days spent in ICU were 2.5 (range 0–6) days, whereas number of days ventilated were 1.3 (range 0–4) days. The median length of hospital stay was 14 (range 8–180) days (Table 2).
Operating time (p = 0.89), intraoperative blood loss (p = 0.26), length of ICU stay (p = 0.42), number of ventilated days (p = 0.24), and length of hospital stay (p = 0.85) were similar in patients younger than age 74 years and those older than 74 years (Table 2). There was no difference in the American Society of Anesthesiology (ASA) grade for the two groups (p = 0.14).
Morbidity and mortality
There were two in-hospital mortalities (3.8 %). The last mortality was recorded in 1999. The morbidity rate was 41 % (22/53 patients). This included ten (18.8 %) pancreatic fistulae (8 minor ISGPF grade A/B, and 2 major ISGPF grade C). All minor leaks could be conservatively managed with total parenteral nutrition, octreotide, and percutaneous drainage where indicated.
A patient with Myasthenia gravis on immunosuppressive therapy suffered a major pancreatic leak in combination with a leak from the gastroenterostomy leading to septicaemia. He underwent numerous operative and interventional radiology procedures, including a reexploration and near total pancreatectomy. His recovery was further complicated by recurrent episodes of sepsis, necessitating a hospital stay of 180 days. Overseas expert opinion was sought in the management of this patient via telemedicine and personal communication.
Biliary anastomotic leak was evident in an 80-year-old female with intraductal papillary mucinous tumour and a nondilated biliary system. Interventional radiology and gastroenterology expertise proved invaluable in stenting the anastomosis to control the leak.
Significant postoperative haemorrhage necessitated urgent reexploration in two patients. A slipped ligature on one of the portal venous tributaries and bleeding from gastroenterostomy staple line were the causes. These were controlled with sutures and the patient’s recovered uneventfully thereafter.
The postoperative morbidities and their frequency are detailed in Table 3. There was a much higher morbidity rate in group B, but this was not statistically significant (26.4 vs. 47 %, p = 0.18) possibly due to the small numbers.
Histology
Commonest tumour location was the head of the pancreas (54.7 %), followed by ampulla of Vater (26.4 %), lower end of common bile duct (13.2 %), and duodenum (5.6 %). 85 % of the patients had malignant tumours. Margins were reported in 49 of 53 (not reported in 4 patients with benign pathology) patients. Forty-two (85.7 %) had microscopically clear margins; four were close (<3 mm). A median of 8 (range 1–27) lymph nodes were sampled. The comparison of outcomes between the groups with age older and younger than 74 years is presented in Table 4.
Survival
Thirty patients were alive at the time of final analysis. Of these, 24 were disease-free whereas 6 had evidence of recurrent/metastatic disease. Of the 23 patients who died during follow-up, 21 had recurrent/metastatic disease. Overall median survival was 14 months for patients with a malignant pathology (Fig. 1).
Discussion
In 1995, Lieberman et al. [15] published a study that demonstrated a relationship between high volume of surgery and low mortality rates. These results were further validated by a number of studies [2, 3]. Birkmeyer’s study published in 2002, based on administrative data of Medicare patients in the United States, showed significantly higher postoperative adverse events in patients undergoing complex surgery in low-volume centres. The difference in mortality in patients undergoing pancreatic resections was especially significant with 3.8 % mortality in very high-volume centres versus 16.8 % in low-volume centres. These studies have encouraged the belief that complex surgical procedures especially in high-risk patients should be centralised to nominated high-volume centres.
Recently published NSQIP [11] risk factor score for predicting morbidity and mortality in PD cites age ≥74 years as an independent predictor for increased morbidity and mortality.
In Australia, many tertiary referral centres with specialised HPB units are low- to medium-volume centres for PD [5, 6]. An average life expectancy of 84 years for females and 79 years for males [16] implies an older patient population at presentation (median age 71 in the current series) at most such centres [5]. Ability to deliver high quality of complex surgery in the elderly at low-volume tertiary centres therefore is vital.
This study was performed at a university teaching hospital. The hospital is equipped with all the expertise and infrastructure to provide a health care delivery system that is equivalent to high-volume centres. The HPB unit is accredited for postfellowship training in HPB surgery by the ANZHPBA.
A total of 53 PDs were performed in the past 14 years. There has been a trend towards an increase in the numbers of PD being performed in recent years (Fig. 2), but volumes remain low. The in-hospital mortality (3.8 %) was similar to that reported from high-volume centres [17–19]. The last recorded mortality was in 1999. Operative times and intraoperative blood loss along with ICU stay were at par with results from high-volume centres [19, 20]. Morbidity was similar to that described in large series and similar in both groups, including a pancreatic fistula rate of 18.8 % [8, 19–21].
The process of patient selection, surgical procedure, and postoperative care has been standardised for over a decade, especially following the last recorded mortality. This consists of protocol-based investigations followed by formal preoperative MDT discussions. The surgical procedures are performed by two senior surgeons working together along with experienced assistants. Surgical and intensive care teams collaborate actively in the postoperative management along with experienced nursing staff. Good gastroenterology and interventional radiology services are readily available after hours and are vitally important in management of complications. Excellent telemedicine support is available for local and overseas consultations. The successful and timely management of significant postoperative complications is a critical indicator of the quality of services provided at any hospital and impacts significantly on the patient outcomes [22]. This was amply illustrated in the current series with the successful management of the patients with significant postoperative complications (two major pancreatic leaks, one biliary leak, and two postoperative haemorrhages) depending on the availability of significant resources: interventional radiology, interventional gastroenterology, expert anaesthetic, and good ICU management along with surgical expertise in early recognition and management. Importance of good interventional radiology support cannot be overstated. Sohn et al. [23] reported that 44 % of patients undergoing pancreatectomy had some type of interventional radiologic procedure. High-quality intensive care facilities are a cornerstone for achieving good outcomes. Many PD patients and most with postoperative complications will require ICU management and presence of a specialist intensivist at the bedside. ICU staffing and safe practices make a difference in patient care in this regard [24].
A policy of close observation and early intervention is the norm for all complex surgeries if complications are suspected. Emick and colleagues [22] conclude that expeditious identification and management of complications prevent them from being fatal. This is borne out by the fact that the morbidity rates for PD remain high at ~40 % [8] even in high-volume hospitals, but the mortality rates are very low. It can be logically argued that better understanding and early management of complications is strongly associated with reduced mortality.
It is our belief that quality infrastructure along with good clinical and surgical expertise and adherence to the aforementioned protocol based standardisation of all aspects of patient care is critically important to obtain good patient outcomes. In short, if the system processes at high-volume centres can be replicated in low-volume centres with good surgical expertise, equivalent outcomes can be achieved.
Elderly patients present a further challenge in complex surgical procedures. Age >74 years is an independent risk factor for increase in morbidity and perioperative mortality according to the recent NSQIP publication [11]. A number of other studies concur that elderly patients undergoing PD have higher morbidity and mortality rates [25, 26]. An increasing number of elderly people are treated in Australian hospitals. This is reflected by the median age of 71 years in this series, which is significantly more than that reported in some large series [19]. The proportion of patients more than 74 years undergoing PD was 35.85 %—much higher than that reported in high-volume hospitals [27]. It is important to evaluate results in this age group in low-volume tertiary centres. In the current series, although there was no statistical difference in the hospital mortality in the elderly age group, there was a definite trend towards increased morbidity. These findings are similar to those reported from high-volume centres [2, 3, 10, 28]. Operating times, blood loss, and transfusion rates were at par with those at high-volume centres [29].
Median survival for patients with malignant pathology was 14 months. Oncological clearance was at par with international standards. Margin positivity and lymph node yield are important prognostic markers in this respect. A R0 clearance was achieved in 85 % patients overall, and this was consistent across both age groups. Microscopic margin positivity has been reported to be ~25 % even in the highest-volume centres [30]. Margin positivity is inversely proportional to survival, and La Torre et al. [30] suggest that margin status rate after PD should be considered a measure of quality for selection of hospitals dedicated to pancreatic surgery.
Standard nonextended lymphadenectomy is most commonly performed in the western world. In this series, the median number of lymph nodes sampled was 8 (range 1–27) and was similar in both age groups. An average yield of 10–15 lymph nodes is the accepted standard for a curative resection in PD [31–33]. The role of extended lymphadenectomy is debatable and most studies have not shown any survival advantage [29, 34]. Survival results similar to high-volume centres even in the elderly can thus be expected based on these prognostic markers.
The results of our series are encouraging. Whilst centralisation for complex surgery is logical to obtain the best outcomes, our study shows that replicating the system processes at high-volume centres makes it possible to achieve good outcomes in low-volume centres with adequate expertise. This is a good alternative when centralisation is not feasible due to geographic and logistic reasons.
Limitations
This is a single-centre study performed on partly retrospective data. Patient numbers are small. We consider the retrospective nature of this study as an advantage, because this reflects the significance of systems already in place at our centre. Specific alterations to the existing systems for a trial setting can potentially influence outcomes in such studies (Hawthorn effect).
Conclusions
PD can be safely performed in a low-volume, specialised unit at centres where the amenities and processes at high-volume centres can be replicated.
References
Begg CB, Cramer LD, Hoskins WJ, Brennan MF (1998) Impact of hospital volume on operative mortality for major cancer surgery. JAMA 280(20):1747–1751
Finlayson EV, Goodney PP, Birkmeyer JD (2003) Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg 138(7):721–725. doi:10.1001/archsurg.138.7.721 discussion 726
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346(15):1128–1137. doi:10.1056/NEJMsa012337
Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, Obertop H (2000) Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg 232(6):786–795
Chen JW, Bhandari M, Astill DS, Wilson TG, Kow L, Brooke-Smith M, Toouli J, Padbury RT (2010) Predicting patient survival after pancreaticoduodenectomy for malignancy: histopathological criteria based on perineural infiltration and lymphovascular invasion. HPB (Oxford) 12(2):101–108. doi:10.1111/j.1477-2574.2009.00140.x
Kwok KH, Rizk J, Coleman M, Fenton-Lee D (2010) Pancreaticoduodenectomy—outcomes from an Australian institution. ANZ J Surg 80(9):605–608. doi:10.1111/j.1445-2197.2010.05348.x
Barnett SA, Collier NA (2006) Pancreaticoduodenectomy: does preoperative biliary drainage, method of pancreatic reconstruction or age influence perioperative outcome? A retrospective study of 104 consecutive cases. ANZ J Surg 76(7):563–568. doi:10.1111/j.1445-2197.2006.03778.x
Samra JS, Bachmann RA, Choi J, Gill A, Neale M, Puttaswamy V, Bell C, Norton I, Cho S, Blome S, Maher R, Gananadha S, Hugh TJ (2011) One hundred and seventy-eight consecutive pancreatoduodenectomies without mortality: role of the multidisciplinary approach. Hepatobiliary Pancreat Dis Int 10(4):415–421
Topal B, Van de Sande S, Fieuws S, Penninckx F (2007) Effect of centralization of pancreaticoduodenectomy on nationwide hospital mortality and length of stay. Br J Surg 94(11):1377–1381. doi:10.1002/bjs.5861
de Wilde RF, Besselink MG, van der Tweel I, de Hingh IH, van Eijck CH, Dejong CH, Porte RJ, Gouma DJ, Busch OR, Molenaar IQ, Dutch Pancreatic Cancer Group (2012) Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Br J Surg 99(3):404–410. doi:10.1002/bjs.8664
Parikh P, Shiloach M, Cohen ME, Bilimoria KY, Ko CY, Hall BL, Pitt HA (2010) Pancreatectomy risk calculator: an ACS-NSQIP resource. HPB (Oxford) 12(7):488–497. doi:10.1111/j.1477-2574.2010.00216.x
Maisonneuve P, Lowenfels AB (2010) Epidemiology of pancreatic cancer: an update. Dig Dis 28(4–5):645–656. doi:10.1159/000320068
Trochsler MTST, Kanhere HA (2011) Pancreatic surgery. In: Wichmann M, Caron N, Maddern G (eds) Rural surgery. Springer, Berlin, pp 187–194
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, International Study Group on Pancreatic Fistula Definition (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13. doi:10.1016/j.surg.2005.05.001
Lieberman MD, Kilburn H, Lindsey M, Brennan MF (1995) Relation of perioperative deaths to hospital volume among patients undergoing pancreatic resection for malignancy. Ann Surg 222(5):638–645
Welfare A (2006) World population prospects: the 2006 Revision
Allareddy V, Ward MM, Allareddy V, Konety BR (2010) Effect of meeting Leapfrog volume thresholds on complication rates following complex surgical procedures. Ann Surg 251(2):377–383. doi:10.1097/SLA.0b013e3181cb853f
Massarweh NN, Flum DR, Symons RG, Varghese TK, Pellegrini CA (2011) A critical evaluation of the impact of Leapfrog’s evidence-based hospital referral. J Am Coll Surg 212(2):150–159. doi:10.1016/j.jamcollsurg.2010.09.027
Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, Hodgin MB, Sauter PK, Hruban RH, Riall TS, Schulick RD, Choti MA, Lillemoe KD, Yeo CJ (2006) 1423 Pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg 10(9):1199–1210. doi:10.1016/j.gassur.2006.08.018
Schmidt CM, Powell ES, Yiannoutsos CT, Howard TJ, Wiebke EA, Wiesenauer CA, Baumgardner JA, Cummings OW, Jacobson LE, Broadie TA, Canal DF, Goulet RJ Jr, Curie EA, Cardenes H, Watkins JM, Loehrer PJ, Lillemoe KD, Madura JA (2004) Pancreaticoduodenectomy: a 20-year experience in 516 patients. Arch Surg 139(7):718–725. doi:10.1001/archsurg.139.7.718
Teh SH, Diggs BS, Deveney CW, Sheppard BC (2009) Patient and hospital characteristics on the variance of perioperative outcomes for pancreatic resection in the United States: a plea for outcome-based and not volume-based referral guidelines. Arch Surg 144(8):713–721. doi:10.1001/archsurg.2009.67
Emick DM, Riall TS, Cameron JL, Winter JM, Lillemoe KD, Coleman J, Sauter PK, Yeo CJ (2006) Hospital readmission after pancreaticoduodenectomy. J Gastrointest Surg 10(9):1243–1252. doi:10.1016/j.gassur.2006.08.016 discussion 1252-1243
Sohn TA, Yeo CJ, Cameron JL, Geschwind JF, Mitchell SE, Venbrux AC, Lillemoe KD (2003) Pancreaticoduodenectomy: role of interventional radiologists in managing patients and complications. J Gastrointest Surg 7(2):209–219
Milstein A, Galvin RS, Delbanco SF, Salber P, Buck CR Jr (2000) Improving the safety of health care: the leapfrog initiative. Eff Clin Pract 3(6):313–316
Sohn TA, Yeo CJ, Cameron JL, Lillemoe KD, Talamini MA, Hruban RH, Sauter PK, Coleman J, Ord SE, Grochow LB, Abrams RA, Pitt HA (1998) Should pancreaticoduodenectomy be performed in octogenarians? J Gastrointest Surg 2(3):207–216
Prashant S, Jonathan T, Mauricio S, James S, Peter D (2012) Advanced age is a risk factor for postoperative complications and mortality after a pancreaticoduodenectomy: a meta-analysis and systematic review. HPB (Oxford) 14(10):649–657. doi:10.1111/j.1477-2574.2012.00506.x
Riall TS, Nealon WH, Goodwin JS, Townsend CM Jr, Freeman JL (2008) Outcomes following pancreatic resection: variability among high-volume providers. Surgery 144(2):133–140. doi:10.1016/j.surg.2008.03.041
Kingsnorth AN (2000) Major HPB procedures must be undertaken in high volume quaternary centres? HPB Surg 11(5):359–361
Yeo CJ, Cameron JL, Sohn TA, Coleman J, Sauter PK, Hruban RH, Pitt HA, Lillemoe KD (1999) Pancreaticoduodenectomy with or without extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma: comparison of morbidity and mortality and short-term outcome. Ann Surg 229(5):613–622 discussion 622-624
La Torre M, Nigri G, Ferrari L, Cosenza G, Ravaioli M, Ramacciato G (2012) Hospital volume, margin status, and long-term survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Am Surg 78(2):225–229
Gutierrez JC, Franceschi D, Koniaris LG (2008) How many lymph nodes properly stage a periampullary malignancy? J Gastrointest Surg 12(1):77–85. doi:10.1007/s11605-007-0251-7
Hellan M, Sun CL, Artinyan A, Mojica-Manosa P, Bhatia S, Ellenhorn JD, Kim J (2008) The impact of lymph node number on survival in patients with lymph node-negative pancreatic cancer. Pancreas 37(1):19–24. doi:10.1097/MPA.0b013e31816074c9
Schwarz RE, Smith DD (2006) Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol 13(9):1189–1200. doi:10.1245/s10434-006-9016-x
Michalski CW, Kleeff J, Wente MN, Diener MK, Buchler MW, Friess H (2007) Systematic review and meta-analysis of standard and extended lymphadenectomy in pancreaticoduodenectomy for pancreatic cancer. Br J Surg 94(3):265–273. doi:10.1002/bjs.5716
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kanhere, H.A., Trochsler, M.I., Kanhere, M.H. et al. Pancreaticoduodenectomy: Outcomes in a Low-Volume, Specialised Hepato Pancreato Biliary Unit. World J Surg 38, 1484–1490 (2014). https://doi.org/10.1007/s00268-013-2431-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2431-9