Abstract
Background
In patients with papillary thyroid carcinoma (PTC), the appropriate extent of lymph node dissection has not yet been established due to lack of accurate patterns of lymph node metastases (LNM). The aim of this study was to clarify the LNM pattern in PTC patients based on our institution’s experience with a consistent technique of bilateral neck dissection, and to consider the rational extent of lymph node dissection.
Methods
Between 1990 and 1999, 152 consecutive patients with PTC who underwent curative total thyroidectomy and bilateral neck dissection as initial treatment were analyzed. The patterns of LNM according to clinicopathological classification were analyzed using the lymph node ratio (LNR; number of metastatic lymph nodes/number of dissected nodes) and frequency (FLNM; number of patients with LNM/number of dissected patients) in cervical compartments.
Results
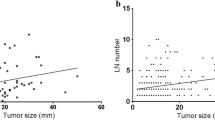
Regardless of clinicopathological classification, LNR in the central compartment was consistently higher than in other compartments, and FLNM in the ipsilateral lateral compartment was consistently higher than in other compartments except for multifocal tumors. The LNR and FLNM in the contralateral lateral compartment were significantly higher in advanced (≥T3) cases than in cases with smaller tumors (T1) and were comparable to those in the ipsilateral lateral compartment in advanced (≥T3) cases.
Conclusions
The pattern of LNR provided a better reflection of the patterns of LNM. In terms of the LNR, central neck dissection is the basic extent of lymph node dissection for all clinically apparent PTC. In advanced patients, it is also advisable to include bilateral lateral neck dissection.








Similar content being viewed by others

References
Noguchi S, Noguchi A, Murakami N (1970) Papillary carcinoma of the thyroid. I. Developing pattern of metastasis. Cancer 26:1053–1060
Udelsman R, Lakatos E, Ladenson P (1996) Optimal surgery for papillary thyroid carcinoma. World J Surg 20:88–93
Caron NR, Clark OH (2006) Papillary thyroid cancer. Curr Treat Options Oncol 7:309–319
Hay ID, Grant CS, Taylor WF et al (1987) Ipsilateral lobectomy versus bilateral lobar resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system. Surgery 102:1088–1095
Scheumann GF, Gimm O, Wegener G et al (1994) Prognostic significance and surgical management of locoregional lymph node metastases in papillary thyroid cancer. World J Surg 18:559–567 discussion 567–558
Mann B, Buhr HJ (1998) Lymph node dissection in patients with differentiated thyroid carcinoma: who benefits? Langenbecks Arch Surg 383:355–358
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418–428
Yanir Y, Doweck I (2008) Regional metastases in well-differentiated thyroid carcinoma: pattern of spread. Laryngoscope 118:433–436
Toniato A, Boschin I, Casara D et al (2008) Papillary thyroid carcinoma: factors influencing recurrence and survival. Ann Surg Oncol 15:1518–1522
Rosa Pelizzo M, Toniato A, Boschin IM et al (2005) Locally advanced differentiated thyroid carcinoma: a 35-year mono-institutional experience in 280 patients. Nucl Med Commun 26:965–968
Noguchi S, Murakami N, Yamashita H et al (1998) Papillary thyroid carcinoma: modified radical neck dissection improves prognosis. Arch Surg 133:276–280
Hartl DM, Travagli JP (2009) The updated American thyroid association guidelines for management of thyroid nodules and differentiated thyroid cancer: a surgical perspective. Thyroid 19:1149–1151
National comprehensive cancer network (2010) Clinical practice guidelines in oncology: thyroid carcinoma. http://www.nccn.org/professionals/physician_gls/f-guidelines.asp. Accessed 27 Apr 2010
British thyroid association and royal college of physicians (2007) Guidelines for the management of thyroid cancer, 2nd ed. http://www.british-thyroid-association.org/news/Docs/Thyroid_cancer_guidelines_2007.pdf, pp 13–15
Rotstein L (2009) The role of lymphadenectomy in the management of papillary carcinoma of the thyroid. J Surg Oncol 99:186–188
McGregor GI, Luoma A, Jackson SM (1985) Lymph node metastases from well-differentiated thyroid cancer. A clinical review. Am J Surg 149:610–612
Shaha AR (1998) Management of the neck in thyroid cancer. Otolaryngol Clin North Am 31:823–831
Machens A, Hinze R, Thomusch O et al (2002) Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg 26:22–28
Qubain SW, Nakano S, Baba M et al (2002) Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery 131:249–256
Sadowski BM, Snyder SK, Lairmore TC (2009) Routine bilateral central lymph node clearance for papillary thyroid cancer. Surgery 146:696–703 discussion 703–695
Kupferman ME, Patterson M, Mandel SJ et al (2004) Patterns of lateral neck metastasis in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 130:857–860
Sivanandan R, Soo KC (2001) Pattern of cervical lymph node metastases from papillary carcinoma of the thyroid. Br J Surg 88:1241–1244
Wada N, Suganuma N, Nakayama H et al (2007) Microscopic regional lymph node status in papillary thyroid carcinoma with and without lymphadenopathy and its relation to outcomes. Langenbecks Arch Surg 392:417–422
Lale Atahan I, Yildiz F, Ozyigit G et al (2008) Percent positive axillary lymph node metastasis predicts survival in patients with non-metastatic breast cancer. Acta Oncol 47:232–238
Lee HY, Choi HJ, Park KJ et al (2007) Prognostic significance of metastatic lymph node ratio in node-positive colon carcinoma. Ann Surg Oncol 14:1712–1717
Leggett MD, Chen SL, Schneider PD et al (2008) Prognostic value of lymph node yield and metastatic lymph node ratio in medullary thyroid carcinoma. Ann Surg Oncol 15:2493–2499
Funahashi H, Satoh Y, Imai T et al (1993) Our technique of parathyroid autotransplantation in operation for papillary thyroid carcinoma. Surgery 114:92–96
Shah JP (1990) Cervical lymph node metastases—diagnostic, therapeutic, and prognostic implications. Oncology (Williston Park) 4:61–69 discussion 72, 76
Hisham AN, Lukman MR (2002) Recurrent laryngeal nerve in thyroid surgery: a critical appraisal. ANZ J Surg 72:887–889
Simon D, Goretzki PE, Witte J et al (1996) Incidence of regional recurrence guiding radicality in differentiated thyroid carcinoma. World J Surg 20:860–866 discussion 866
Grebe SK, Hay ID (1996) Thyroid cancer nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am 5:43–63
Gimm O, Rath FW, Dralle H (1998) Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg 85:252–254
Wada N, Duh QY, Sugino K et al (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237:399–407
Disclosure
The authors have no conflicts of interest or financial ties to disclose.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takada, H., Kikumori, T., Imai, T. et al. Patterns of Lymph Node Metastases in Papillary Thyroid Carcinoma: Results from Consecutive Bilateral Cervical Lymph Node Dissection. World J Surg 35, 1560–1566 (2011). https://doi.org/10.1007/s00268-011-1133-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1133-4