Abstract
Background
Since probiotics are considered to exert beneficial health effects by enhancing the host’s immune response, we investigated the benefits of a synbiotics treatment on the rate of infections, systemic inflammatory response syndrome (SIRS), severe sepsis, and mortality in critically ill, mechanically ventilated, multiple trauma patients. Length of stay in the intensive care unit (ICU) and number of days under mechanical ventilation were also evaluated.
Method
Sixty-five patients were randomized to receive once daily for 15 days a synbiotic formula (Synbiotic 2000Forte, Medipharm, Sweden) or maltodextrin as placebo. The synbiotic preparation consisted of a combination of four probiotics (1011 CFU each): Pediococcus pentosaceus 5–33:3, Leuconostoc mesenteroides 32–77:1, L. paracasei ssp. paracasei 19; and L. plantarum 2,362; and inulin, oat bran, pectin, and resistant starch as prebiotics. Infections, septic complications, mortality, days under ventilatory support, and days of stay in ICU were recorded.
Results
Synbiotic-treated patients exhibited a significantly reduced rate of infections (P = 0.01), SIRS, severe sepsis (P = 0.02), and mortality. Days of stay in the ICU (P = 0.01) and days under mechanical ventilation were also significantly reduced in relation to placebo (P = 0.001).
Conclusion
The administration of this synbiotic formula in critically ill, mechanically ventilated, multiple trauma patients seems to exert beneficial effects in respect to infection and sepsis rates and to improve the patient’s response, thus reducing the duration of ventilatory support and intensive care treatment.
Similar content being viewed by others
Critically ill trauma patients are at increased risk for the development of severe and even fatal infections despite advanced therapeutic measures and meticulous monitoring. This is the result of multiple factors, including the increased patient’s catabolism, decreased immune function, and gut-barrier malfunction. Additionally, the critical illness itself is coupled with prolonged use of mechanical ventilatory support as well as of other invasive procedures and devices; thus, the patient is subjected to an increased exposure to potentially pathogenic gram negative microorganisms, either from the hospital environment or, mainly, from his or her own microflora.1,2,3
In recent years, the importance of the intestinal microflora composition in physiological and pathophysiological processes in the human gastrointestinal tract has become ever more evident, and an ongoing number of trials dealing with the beneficial effects of probiotics—in particular, specific lactobacilli and bifidobacteria—given to manipulate the composition of gastrointestinal microflora have been published. The effects of probiotics are attributed to the enhancement of the immune response to pathogens, restoration to normal of increased intestinal permeability, balanced gut microecology, improved immunological gut barrier function, and downregulation of proinflammatory cytokines.4 They have been used extensively in many clinical situations, such as patients with acute pancreatitis, liver transplantation, antibiotic associated diarrhea, inflammatory bowel disease, and pouchitis.5,6,7 The experience, however, obtained from treatment in critically ill patients, and especially of those after multiple trauma—in whom the acute neurohormonal and inflammatory cascades and immediate immune responses are already over—is still limited.
Thus, we proposed to investigate the benefits of treatment with a combination of pre- and probiotics regimens in critically ill, long-term mechanically ventilated patients after severe polytrauma. The end points of the study were infection rate, duration of stay under ventilatory support and in the ICU, and mortality. Proinflammatory indexes were supplementarily used for comparative evaluation of patients’ improvement.
MATERIAL AND METHODS
Patients
All severe multiple trauma victims admitted over a 12-month period to any 1 of the 5 participating surgical ICUs of the Thessaloniki University’s tertiary-care AHEPA Hospitals and the affiliated 424th Military Hospital were eligible for the study. Patients were enrolled if they had two or more organ-system traumas, if it was predicted that they would have a long ICU stay and would need to be mechanically ventilated or under ventilatory support, if they were older than 18 years of age and with a life expectancy of more than 15 days after randomization. Pregnancy or lactation, immunosuppression, obesity (BMI > 40), or any contraindication to enteral administration of medication were additional causes for exclusion of patients from the study.
A sample-size calculation based on data previously collected by our group demonstrated that approximately 102 patients would be required to demonstrate a 30% reduction in overall infections at the 5% significance level with a power of 80%. An intermediate analysis was performed after recruiting 60% of patients, the results of which are presented herein. The study was approved by the University of Thessaloniki Research Ethics Committee. Informed consent was obtained from all patients’ first-degree relatives on entry into the study.
Randomization and Treatment Regimens
This study was a double-blind, placebo-controlled trial. Patients were randomly assigned to receive synbiotic or placebo treatment according to a list blinded to study investigators and physicians in charge. The synbiotic preparation (Synbiotic 2000Forte, Medipharm, Sweden) consisted of a combination of 1011 CFU of each of four probiotics; Pediococcus pentoseceus 5–33:3, Leuconostoc mesenteroides 32–77:1, L. paracasei ssp 19, and L. plantarum 2362, as well as 2.5 g each of inulin, oat bran, pectin, and resistant starch. It was given in doses of 12 g (1 sachet) per day for a 15-day study period, diluted in 100 ml of tap water. The placebo preparation consisted of identical doses of powdered glucose polymer (maltodextrin, Caloreen, Nestle, UK).
The two groups did not differ with respect to age, gender, underlying disease comorbidities, severity of trauma on ICU admission, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, Glasgow Coma Scale, and route of nutrition (Table 1). All patients had at least one central venous catheter inserted and an arterial line. Medication was administered via endoscopic gastrostomy or through a nasogastric tube by ICU nursing staff. All received concomitant therapy with antibiotics, inotropes, and enteral or parenteral nutrition, as considered appropriate by the attending clinician. Proton pump inhibitors or histamine–H2 antagonists were used routinely. The study medication was terminated after a 15-day period; in the case of a patient discharge from ICU earlier, he or she was automatically excluded from the study.
Study Variables
Study variables included patient’s demographics and comorbidities,8 admission diagnosis, medical history, surgical procedures, medical treatment, devices, and microbiological, biochemical, and hematological data. The Glasgow Coma Scale and the APACHE II score on admission to the ICU;9 infections, sepsis, acute organ system failure, and outcome were also recorded.10,11 Follow-up continued until death or discharge from the ICU.
Definitions
Systemic inflammatory response syndrome (SIRS), sepsis, septic shock, and multiple organ dysfunction syndrome (MODS) were defined according to the American College of Chest Physicians Definitions and Guidelines and the American College of Chest Physicians/Society of Critical Care Medicine (ACCP/SCCM) Consensus Conference Committee.12,13,14 Clinical diagnosis of bacterial pneumonia was defined by the presence of all of the following criteria: new or progressive pulmonary radiological infiltrate, purulent tracheal secretions, fever (> 38.5°C), and leukocytosis or leukopenia (white blood cell count more than 12 × 109 L−1 or less than 4 × 109 L−1).15,16,17 Diagnosis of pneumonia was regarded as microbiologically confirmed by the isolation of a potentially pathogenic microorganisms in bronchoalveolar lavage in concentrations of 105 CFU mL−1 or more.
Systemic infections were diagnosed according to standard definitions.15,18 Bacteremia was diagnosed when a pathogen was isolated from the blood with a temperature above 38.5°C or below 35°C or a white blood cell count greater than 10 × 109 L−1 or less than 3 × 109 L−1 and it was not related to infection at another site. Intraabdominal infection was diagnosed when a pathogen was isolated from a culture of purulent material during surgery or drainage. Urinary tract infection was diagnosed if the urine culture showed at least 105 colonies of a pathogen. Catheter-related sepsis was diagnosed if the patient had local signs of infection at the entry site, a temperature above 38.5°C or below 35°C, a white blood cell count greater than 10 × 109 L−1 or less than 3 × 109 L−1 that resolved after catheter removal with no other infection site, the semiquantitative culture of the catheter tip showing more than 15 CFU mL−1, or isolation of a pathogen from blood cultures.
Systemic Inflammatory Response
To quantify systemic inflammatory response, serum levels of procalcitonin (PCT) and C-reactive protein (CRP) were measured on days 0, 4, 7, and 15. Serum PCT was estimated with an assay based on immunochemiluminescence (BRAHMS Diagnostica, Berlin, Germany; lower detection limit of 0.1 ng·mL−1, upper limit 0.5 ng·mL−1), and CRP was measured by nephelometry (Boehring, Mannhein, Germany; lower detection limit of 0 mg·dl, upper limit 0.8 mg·dL−1). According to the diagnostic cutoffs proposed previously, PCT levels higher than 2 ng·mL−1 are strongly suggestive of the surgical ICU patient being in SIRS, higher than 10 ng·mL−1 as being in severe sepsis, and higher than 20 ng·ml as being in septic shock.19,20,21
Additionally, blood was collected on the same days for estimation of proinflammatory cytokines tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and malondialdehyde (MDA) as an index of oxidative stress. Serum was kept refrigerated at −70°C until measurements using enzyme immunoassay (Diaclone Inc., Paris, France) for cytokines and thiobarbiturate assay for MDA. Lower detections limits were 0.50 and 6.25 pg·mL−1 for TNF-α and IL-6, respectively.
Outcome Measures
Patients entered into the study were followed prospectively until ICU discharge. Primary endpoints were systemic infection rate during ICU stay, as described previously or the development of SIRS and MODS. Mortality, length of stay in the ICU, and number of days under mechanical ventilation were secondary endpoints. Clinical efficacy was defined as either the absence of infection or a reduction of the days in the ICU and/or under mechanical ventilation.
Statistical Analysis
Data were stored on a Microsoft Excel spreadsheet, and statistical analysis was performed using SPSS for Windows Version 10.0 (SPSS Inc., Chicago, IL, USA). Qualitative data were compared using the two-tailed chi-square test. Quantitative data were expressed as medians plus range or means, with standard deviation (SD) of the mean. Differences between means were evaluated using analysis of variance (ANOVA) or paired t-tests, as appropriate. The Mann–Whitney U-test was used to compare nonparametric data. A P-value of 0.05 or less was considered to indicate statistical significance.
RESULTS
Patients
Sixty percent of the calculated sample size was recruited in this study, which means 35 and 30 patients to the synbiotic- and placebo-treated groups, respectively. Seventy-seven patients were initially allocated randomly into two groups of 41 and 36 patients, respectively; 12 patients were not eligible for analysis because of death within the first 48 hours postinjury.
Systemic Infections and Septic Complications
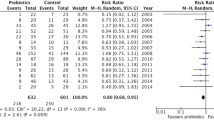
The overall infection rate was 63% in the synbiotic group in comparison with 90% in the placebo-treated group (P = 0.01). Forty patients developed 1 or more septic complications during the study period: 17 out of 35 (49%) in the synbiotic group and 23 out of 30 (77%) in the placebo-treated group, (P = 0.02) (Table 2).
The most common site of infection was the respiratory tract (19 and 24 patients, respectively, P = 0.03), followed by central line (13 and 20 patients, respectively, P = 0.02), urine (6 and 13 patients, respectively, P = 0.02), and wound infection (6 and 8 patients, respectively, P = 0.35). The most frequently isolated organisms from septic foci were Pseudomonas aeruginosa, Acinetobacter baumannii, Staphylococcus aureus, methicillin-resistant Staphylococcus Aureus (MRSA), Klebsiella pneumoniae, Proteus mirabilis, Candida albicans, Escherichia coli, Enterococcus faecalis, and Chryseobacterium indologenes.
A total of 19 patients, 6 from the synbiotic group and 13 from the placebo group, developed severe sepsis (P = 0.02); 14 (21.5%) patients died, 5 (14.3%) from the synbiotics group and 9 (30%) from the placebo-treated group (P = 0.12) after MODS development. In all patients, death occurred within the 2nd week of entry into the study (Table 2).
Days of Ventilation and in ICU
The number of days the patients needed mechanical ventilation were a median of 15 (range 5–32) days for the synbiotic group and a median of 26 (range 7–60) days for the placebo-treated patients (P = 0.001). Additionally, a median of 5 (range 3–12) days and 9 (range 5–14) days, respectively, were needed for total weaning from ventilatory support. Total duration of ICU stay for patients who survived was a median of 25 (range 13–54) days in the synbiotic group and a median of 43 (range 17–82) days in the placebo group. (P = 0.01).
Systemic Inflammatory Response
Mean levels of PCT on days 0, 4, 7, and 15 are shown in Fig. 1. PCT was found significantly elevated on day 4 in relation to day 0 in both groups. However, there was a highly statistically significant difference between groups, with the synbiotic group having the lowest. On days 7 and 15, there was a further reduction in both groups, but there were significant differences between the groups at any time point (P = 0.05, ANOVA). Similar was the expression profile of CRP in both groups, as well as the statistical differences between groups and among study periods (P = 0.05, ANOVA), Fig. 2.
Mean values of procalcitonin (PCT) throughout the study period. Open bars represent the synbiotic group, and closed bars represent the placebo group. One asterisk represents significance at the level of 5% (P = 0.05), two asterisks at the level of 1% (P = 0.01), and three asterisks at the level of 0.1% (P = 0.001) between synbiotic and placebo groups within the same study period.
Mean values of C-reactive protein (CRP) throughout the study period. Open bars represent synbiotic group and closed bars represent placebo group. One asterisk represents significance at the level of 5% (P = 0.05) two asterisks at the level of 1% (P = 0.01) and three asterisks at the level of 0.1% (P = 0.001) between synbiotic and placebo within the same study period.
Concerning MDA, a very high mean value was found on day 4 in the placebo-treated group in relation to the synbiotic group, in which it was also elevated. The next measurements, on days 7 and 15, respectively, revealed a sharper reduction in the synbiotic group than in the placebo (P = 0.05, ANOVA), Fig. 3.
Mean values of malondialdehyde (MDA) throughout the study period. Open bars represent the synbiotic group, and closed bars represent the placebo group. One asterisk represents significance at the level of 5% (P = 0.05), two asterisks at the level of 1% (P = 0.01), and three asterisks at the level of 0.1% (P = 0.001) between the synbiotic and placebo groups within the same study period.
Finally, cytokine TNF-α assay revealed an increase on day 4 in both groups in relation to day 0 (Fig. 4). Both TNF-α and IL-6 (Fig. 5) exhibited a trend toward reduction in both groups from day 4 over the course of the study. However, mean values in the synbiotic group were significantly reduced at any time point in relation to the placebo-treated group (P = 0.05, ANOVA).
Mean values of tumor necrosis factor-α (TNF-α) throughout the study period. Open bars represent the synbiotic group, and closed bars represent the placebo group. One asterisk represents significance at the level of 5% (P = 0.05), two asterisks at the level of 1% (P = 0.01), and three asterisks at the level of 0.1% (P = 0.001) between the synbiotic and placebo groups within the same study period.
Gastrointestinal Complications
A total of 7 out of 35 and 5 out of 30 patients received total parenteral nutrition during their ICU hospitalization (P = 0.72). Enteral nutrition and medication was generally administered through an endoscopic gastrostomy tube. The diet was infused at a constant rate throughout the 24 hours by an infusion pump. The incidence of gastrointestinal complications in the synbiotic and placebo groups, respectively, exhibited a significant difference at the level of 5%: 10 patients had severe constipation (4 and 6, respectively, P = 0.34), 15 had diarrhea (5 and 10, respectively, P = 0.04), and 22 had increased gastric residuals (7 and 15, respectively, P = 0.01). Despite the relatively high gastrointestinal complication rate, only three placebo-treated patients switched back to parenteral nutrition.
DISCUSSION
Nosocomial infections are a common problem in ICU-hospitalized patients, dramatically increasing the already high—due to the critical illness—morbidity and mortality. More over, multiple trauma patients who need mechanical ventilation, especially those with chest trauma, are at higher risk of infection. These infections, directly related to the suppressed immune function and the gut-barrier malfunction, seem to promote a continuous systemic inflammatory response and in some cases result in multiple organ and system dysfunction and eventually death.
Although the pathogenesis of sepsis and multiple organ failure remains obscure, it is generally believed that the gut plays a pivotal role; the precise mechanism is not clearly documented in humans, but there is evidence to suggest changes in gastrointestinal microflora associated with the acute illness, gut ischemia, immunosuppression, the use of broad-spectrum antibiotics, and nutrient-deprivation stress.3,22 It is also known from experimental studies with induced disease such as pancreatitis that the Lactobacillus flora disappears after 6–8 hours and is replaced by an overgrowth of potentially pathogenic microorganisms; soon thereafter, microbial translocation follows.23 Similarly, Knight et al.24 support the view that the majority of patients in the ICU have lost their total Lactobacillus flora, but this loss can successfully be compensated for by supply of a specific synbiotic preparation.23 Recent research documenting the presence of various microorganisms, such as lactobacilli, bifidobacteria, and anaerobic bacteria have been shown to occupy critical receptors on intestinal epithelial cells, which prevent colonizing pathogens from occupying a niche for persistence and proliferation.22,25
Thus, an alternative approach to gut commensal floral changes is the preservation or reestablishment of normal gut flora with pro- and prebiotics. Probiotics are live microbial supplements that have a beneficial effect on the host by altering gastrointestinal flora. Prebiotics are nondigestible sugars that selectively stimulate the growth of certain colonic bacteria. When administered in combination, prebiotics may enhance the survival of probiotic strains as well as stimulating the activity of the host’s endogenous bacteria. The combination of a pre- and probiotics has been termed synbiotic.
The objectives of the present study were to investigate the effects of such a combination regimen of pro- and prebiotics, namely, Synbiotic 2000Forte, on the clinical outcome of critically ill patients long-term mechanically ventilated after severe polytrauma. We found that this treatment can significantly decrease the overall infection rate from 90% to 63% and thus the rate of SIRS and sepsis complications from 77% to 49%, and the subsequent mortality rate of 30% in the placebo-treated group to 14.3%. Both groups were comparable in terms of demographic data and illness severity, and all patients had multiple trauma of similar extent and severity.
ICU research in this area is in its early stages. The only pilot data available thus far involve a comparison between treatment with live lactobacilli plus oat fiber and heat-treated lactobacilli with oat fiber as a control in critically ill patients with respect to multiorgan dysfunction. This study, with 19 patients in each arm, resulted in a mortality rate of 26% in the live synbiotic group versus 42% in the control group.26 Although this is too small a study to allow statistical significance, the same unit is currently undertaking a large-scale trial, and more than 300 patients have thus far been recruited (unpublished data, referred by27).
We did not achieve a diminished rate of overall infection in our material although we used the “Forte” regimen, which is stronger than the simple one (Synbiotic 2000). However, the observed reduction from the rate of 80%–54% for respiratory tract infections, from 66% to 37% for central line infections, from 43% to 17% for urine, and from 26% to 17% for wound infections, and from 90% to 63% for the total number of infections is considered of great importance for the life of our patients. The high rates of infections found in our patients reflect that of the literature on polytrauma patients needing mechanical ventilation for a long period;14 additionally, our patients had a high APACHE II score representing critical illness, and the majority combined abdominal, chest, and cerebral injury. Severe illnesses can also be verified by the number of days on mechanical ventilation as well as days of stay in ICU. The control group remained under mechanical ventilation for a median of 26 (range 7–60) days, needing a median of 9 (range 5–14) additional days for total weaning from ventilatory support, and had an overall ICU stay of a median of 43 (range 17–82) days. The use of synbiotic treatment led to a significant reduction of all parameters to a median of 15 (range 5–32) days and a median of 5 (range 3–12) days, respectively, for ventilator dependence and to a median of 25 (range 13–54) days for overall ICU stay.
A similar reduction of hospitalization days is referred to in a randomized, double-blind study on acute pancreatitis patients receiving L. plantarum 299v or heat-inactivated L. plantarum for 1 week through a nasojejunal feeding tube. A trend toward a shorter mean length of hospitalization (13.7 vs. 21.4 days) was prominent in the live Lactobacillus group, which also exhibited a decrease in pancreatic necrosis infection rate (1 out of 22 patients in the live Lactobacillus group compared with 7 out of 23 in the control group).28 The common point between this study and ours was the use of L. Plantarum contained in the synbiotic formula. The most unique feature of the well-studied Lactobacillus, L. plantarum, is its ability to catabolize arginine toward nitric oxide, which is involved in a series of important gastrointestinal (GI) functions such as bacteriostasis, mucus secretion, regulation of motility and splanchnic circulation, and in stimulation of GI immune functions.29,30 Although this function is interrupted or at least depressed by antibiotic treatment, such as neomycin, bacitracin, and polymyxin B,31 which are commonly administered to sepsis patients, the results with respect to infection rate reduction are not disappointing; on the other hand, the excessive use of antibiotics or even worse, of a combination of antibiotics, would be the reason of the less impressive reduction in infection rate.
The severity of critical illness in our patients, besides the high APACHE II scores, is documented by the high values of CRP and, especially, PCT. Today, PCT has been proposed as a reliable indicator of systemic infection, even in the presence of immunosuppression. The finding of values over 10 ng·mL−1 in many of our patients is strongly suggestive of severe sepsis 19,20 and, even more, septic shock (> 20 ng·mL−1), as they actually were. On the other hand, cytokines as indexes of systemic inflammatory response and MDA as an index of oxidative stress, although good indicators of the significant difference between groups favoring synbiotics, had no further usefulness for the quantification of illness severity.
Finally, another point to be discussed is the improvement in the rate of GI complications seen in our patients. Although the absolute number of complications is small, a trend toward normalization of gut motility (constipation or diarrhea) and improvement of upper GI motility (shorter time for gastric empting) was prominent in our treated versus placebo patients. Literature dealing with severely ill medical and surgical patients mainly focuses on antibiotic-associated diarrhea. We did not experience a great number of such problems in our patients, so we are unable to correlate them with the use of synbiotic treatment. However, two published meta-analyses have evaluate all randomized, double-blind, controlled trials of probiotics in the prevention of antibiotic-associated diarrhea and confirm an odds ratio of 0.39 and 0.37, respectively, in favor of probiotics treatment over placebo.32,33
Although ICU patients seem to be the most disadvantageous group to treat because treatment is initiated after the peak of acute-phase response, results of the present study are encouraging: the early institution of treatment by this synbiotic regimen in critically ill multiple trauma patients seems to be associated with measurable clinical benefits in relation to matched placebo-treated patients: it significantly reduces the systemic infection rate as well as the incidence of SIRS, severe sepsis, MODS, and mortality, and it also significantly shortens the total length of stay in the ICU and the number of days the patient needs mechanical ventilatory support. These beneficial effects support the current trend of using synbiotic to up-regulate the host’s inflammatory response; however, further studies are needed to clarify their usefulness in acute illness and to assess the “therapeutic window” of successful immunomodulation treatment.
References
Deitch EA. Multiple organ failure. Pathophysiology and potential future therapy. Ann Surg 1992;216:117–134
Vincent JL, Bihari DJ, Suter PM, et al. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European prevalence of infection in intensive Care [EPIC] study. EPIC International Advisory Committee. J Am Med Assoc 1995;274:639–644
Marshall JC. Gastrointestinal flora and its alterations in critical illness. Curr Opin Clin Nutr Metabc Care 1999;2:405–411
Isolauri E, Salminen S, Ouwehand AC. Microbial-gut interactions in health and disease. Probiotics. Best Pract Res Clin Gastroenterol 2004;18:299–313
Bengmark S. Econutrition and health maintenance—a new concept to prevent GI inflammation, ulceration and sepsis. Clin Nutr 1996;15:1–10
Kailasapathy K, Chin J. Survival and therapeutic potential of probiotic organisms with reference to Lactobacillus acidophilus and Bifidobacterium spp. Immunol Cell Biol 2000;78:80–88
McNaught CE, Woodcock NP, MacFie J, et al. A prospective randomised study of the probiotic Lactobacillus plantarum 299 V on indices of gut barrier function in elective surgical patients. Gut 2002;51:827–831
Pittet D, Thievent B, Wenzel RP, et al. Importance of pre-existing co-morbidities for prognosis of septicemia in critically ill patients. Intensive Care Med 1993;19:265–272
Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818–829
Knaus WA, Draper EA, Wagner DP, et al. Prognosis in acute organ-system failure. Ann Surg 1985;202:685–693
Pittet D, Thievent B, Wenzel RP, et al. Bedside prediction of mortality from bacteremic sepsis. A dynamic analysis of ICU patients. Amer Jl Resp Crit Care Med 1996;153:684–693
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference. Definitions for sepsis and multiple organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 1992;20:864–874
Bone RC, Balk RA, Cerra FB, et al. The ACCP/SCCM Consensus Conference Committee. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992;101:1656–1662
Brun-Buisson C. The epidemiology of the systemic inflammatory response. Intensive Care Med 2000;26:S64–S74
Garner JS, Jarvis WR, Emori TG, et al. CDC definitions for nosocomial infections. Am J Infect Control 1988;16:128–140
Chastre J, Fagon JY. Invasive diagnostic testing should be routinely used to manage ventilated patients with suspected pneumonia. Am J Respir Crit Care Med 1994;150:570–574
American Thoracic Society. Hospital-acquired pneumonia in adults: diagnosis, assessment of severity, initial antimicrobial therapy, and preventive strategies. A consensus statement. Am J Respir Crit Care Med 1996;153:1711–1725
Eggimann P, Pittet D. Infection control in the ICU. Chest 2001;120:2059–2093
Brunkhorst FM, Wegscheider K, Forycki ZF, et al. Procalcitonin for early diagnosis and differentiation of SIRS, sepsis, severe sepsis and septic shock. Intensive Care Med 2000;26 [Suppl 2]: S148–S152
Zahorec R. Definition for septic syndrome should be re-evaluated. Intensive Care Med 2000;26:1870
Giamarellos-Bourboulis EJ, Plachouras D, Tzivra A, et al. Stimulation of innate immunity by susceptible and multidrug-resistant Pseudomonas aeruginosa: an in vitro and in vivo study. Clin Experimental Immunol 2004;135:240–246
Alverdy J, Zaborina O, Wu L. The impact of stress and nutrition on bacterial-host interactions at the intestinal epithelial surface. Curr Opin in Clin Nutr Metab Care 2005;8:205–209
Bengmark S. Synbiotics to strengthen gut barrier function and reduce morbidity in critically ill patients. Clin Nutr 2004;23:441–445
Knight DJW, Girling KJ. Gut flora in health and disease. Lancet 2003;361:1831
Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, et al. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell 2004;118:229–241
Gomersall CM. Does the Administration of Lactobacillus to Critically Ill Patients Decrease the Severity of Multi-Organ Dysfunction and Failure? A Pilot Study. London, Roehampton Institute, School of Life Sciences, 1998
Bengmark S, Martindale R. Prebiotics and synbiotics in clinical medicine. Nutr in Clin Pract 2005;20:244–261
Olah A, Belagyi T, Issekutz A, et al. Randomized clinical trial of specific lactobacillus and fibre supplement to early enteral nutrition in patients with acute pancreatitis. Br J Surg 2002;89:1103–1107
Duncan C, Dougall H, Johnston P, et al. Chemical generation of nitric oxide in the mouth from the enterosalivary circulation of dietary nitrate. Nat Med 1995;1:546–551
Bengmark S. Ecological control of the gastrointestinal tract. The role of probiotic flora. Gut 1998;42:2–7
Wright CE, Rees DD, Moncada S. Protective and pathological role of nitric oxide in endotoxin shock. Cardiovasc Res 1992;26:48–57
Cremonini F, Di Caro S, Nista EC, et al. Meta-analysis: the effect of probiotic administration on antibiotic-associated diarrhoea. Aliment Pharmacol Ther 2002;16:1461–1467
D’Souza AL, Rajkumar C, Cooke J, et al. Probiotics in prevention of antibiotic associated diarrhoea: meta-analysis. Br Med J 2002;324:1361
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kotzampassi, K., Giamarellos-Bourboulis, E.J., Voudouris, A. et al. Benefits of a Synbiotic Formula (Synbiotic 2000Forte®) in Critically Ill Trauma Patients: Early Results of a Randomized Controlled Trial. World J. Surg. 30, 1848–1855 (2006). https://doi.org/10.1007/s00268-005-0653-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0653-1