Abstract
Background
Existing evaluation tools of tear trough deformity are based on subjective impression of clinicians. More accurate quantitative assessment methods are needed. This study aimed to propose a quantitative three-dimensional assessment method for the tear trough deformity in comparison with the Barton’s grading system and apply it to the efficacy evaluation of orbital septum fat transposition.
Methods
117 healthy Chinese adults (234 eyes) were enrolled and divided into four groups according to the Barton’s grading system. Three-dimensional facial images were captured using Vectra H1 handheld camera. 6 anthropometric landmarks were identified on each eye and 8 linear measurements were generated accordingly. Intra-observer reliability was determined and measurements were compared between groups. Pre- and post-operative three-dimensional measurements were compared in 19 patients who received lower blepharoplasty with orbital septum fat transposition.
Results
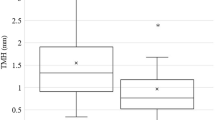
The severity of tear trough was positively correlated with age (P < 0.001) but not BMI (P = 0.145) or gender (P = 0.280). Intra-rater reliability of the 8 linear measurements was excellent except for the vertical distance between the palpebrale inferioris margin and the tear trough below the pupillary center. Intergroup comparison showed that the horizontal distance between the lateral end of tear trough (P < 0.001) and medial canthus and the sagittal vector from tear trough point toward eyelid bag point (P = 0.009) increased with grade, while the vertical distance from mid-pupil to palpebrale inferioris margin decreased gradually (P = 0.001). Orbital septum fat transposition significantly improved the tear trough deformity as assessed by these three-dimensional measurements.
Conclusions
We demonstrated a novel quantitative evaluation method of the tear trough deformity using three-dimensional stereophotogrammetry and proved it to be valid and reliable. It showed good value of clinical application and might help with periorbital rejuvenation planning and outcome assessment.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.




Similar content being viewed by others
References
Wong CH, Hsieh MKH, Mendelson B (2012) The tear trough ligament: anatomical basis for the tear trough deformity. Plast Reconstr Surg 129(6):1392–1402. https://doi.org/10.1097/PRS.0b013e31824ecd77
Goldberg RA, McCann JD, Fiaschetti D et al (2005) What causes eyelid bags? Analysis of 114 consecutive patients. Plast Reconstr Surg 115(5):1395–1402. https://doi.org/10.1097/01.prs.0000157016.49072.61
Anido J, Fernández JM, Genol I et al (2021) Recommendations for the treatment of tear trough deformity with cross-linked hyaluronic acid filler. J Cosmet Dermatol 20(1):6–17. https://doi.org/10.1111/jocd.13475
Hirmand H (2010) Anatomy and nonsurgical correction of the tear trough deformity. Plast Reconstr Surg 125(2):699–708. https://doi.org/10.1097/PRS.0b013e3181c82f90
Barton FE Jr, Ha R, Awada M (2004) Fat extrusion and septal reset in patients with the tear trough triad: a critical appraisal. Plast Reconstr Surg 113(7):2115–2121. https://doi.org/10.1097/01.prs.0000122409.00716.34
Donofrio L, Carruthers J, Hardas B et al (2016) Development and validation of a photonumeric scale for evaluation of infraorbital hollows. Dermatol Surg 42(1):S251-s258. https://doi.org/10.1097/dss.0000000000000856
Rohrich RJ, Ghavami A, Mojallal A (2011) The five-step lower blepharoplasty: blending the eyelid-cheek junction. Plast Reconstr Surg 128(3):775–783. https://doi.org/10.1097/PRS.0b013e3182121618
Goldberg RA (2000) Transconjunctival orbital fat repositioning: transposition of orbital fat pedicles into a subperiosteal pocket. Plast Reconstr Surg 105(2):743–748. https://doi.org/10.1097/00006534-200002000-00044
Kawamoto HK, Bradley JP (2003) The tear “TROUF” procedure: transconjunctival repositioning of orbital unipedicled fat. Plast Reconstr Surg 112(7):1903–1907. https://doi.org/10.1097/01.Prs.0000091238.72843.7e
Nassif PS (2005) Lower blepharoplasty: transconjunctival fat repositioning. Facial Plast Surg Clin North Am 13(4):553–559. https://doi.org/10.1016/j.fsc.2005.06.006
Momosawa A, Kurita M, Ozaki M et al (2008) Transconjunctival orbital fat repositioning for tear trough deformity in young Asians. Aesthet Surg J 28(3):265–271. https://doi.org/10.1016/j.asj.2008.02.002
Pak C, Yim S, Kwon H et al (2018) A novel method for lower blepharoplasty: repositioning of the orbital septum using inverted T-shaped plication. Aesthet Surg J 38(7):707–713. https://doi.org/10.1093/asj/sjy010
Chen J, Zhang T, Zhu X et al (2021) Fat repositioning with a combination of internal fixation and external fixation in transconjunctival lower blepharoplasty. Aesthet Surg J 41(8):893–902. https://doi.org/10.1093/asj/sjab059
Lambros V (2007) Observations on periorbital and midface aging. Plast Reconstr Surg 120(5):1367–1376. https://doi.org/10.1097/01.prs.0000279348.09156.c3
Chong Y, Li J, Liu X et al (2021) Three-dimensional anthropometric analysis of eyelid aging among Chinese women. J Plast Reconstr Aesthet Surg 74(1):135–142. https://doi.org/10.1016/j.bjps.2020.08.010
Park DH, Choi WS, Yoon SH et al (2008) Anthropometry of asian eyelids by age. Plast Reconstr Surg 121(4):1405–1413. https://doi.org/10.1097/01.prs.0000304608.33432.67
Stutman RL, Codner MA (2012) Tear trough deformity: review of anatomy and treatment options. Aesthet Surg J 32(4):426–440. https://doi.org/10.1177/1090820x12442372
Atiyeh B, Hakim CR, Oneisi A et al (2023) Surgical correction of tear trough deformity (TTD) with orbicularis retaining ligament release and volume augmentation for periorbital rejuvenation: review of the literature. Aesthetic Plast Surg 47(1):199–214. https://doi.org/10.1007/s00266-022-03183-0
Wong CH, Mendelson B (2019) The long-term static and dynamic effects of surgical release of the tear trough ligament and origins of the orbicularis oculi in lower eyelid blepharoplasty. Plast Reconstr Surg 144(3):583–591. https://doi.org/10.1097/prs.0000000000005908
Miller TR (2016) Long-term 3-dimensional volume assessment after fat repositioning lower blepharoplasty. JAMA Facial Plast Surg 18(2):108–113. https://doi.org/10.1001/jamafacial.2015.2184
Cristel RT, Caughlin BP (2020) Lower blepharoplasty three-dimensional volume assessment after fat pad transposition and concomitant fat grafting. Facial Plast Surg 36(4):478–483. https://doi.org/10.1055/s-0040-1713790
Miranda RE, Matayoshi S (2022) Vectra 3D simulation in lower eyelid blepharoplasty: how accurate is it? Aesthetic Plast Surg 46(3):1241–1250. https://doi.org/10.1007/s00266-021-02661-1
Guo Y, Rokohl AC, Schaub F et al (2019) Reliability of periocular anthropometry using three-dimensional digital stereophotogrammetry. Graefes Arch Clin Exp Ophthalmol 257(11):2517–2531. https://doi.org/10.1007/s00417-019-04428-6
Guo Y, Schaub F, Mor JM et al (2020) A simple standardized three-dimensional anthropometry for the periocular region in a european population. Plast Reconstr Surg 145(3):514e–523e. https://doi.org/10.1097/prs.0000000000006555
Funding
The work was supported by National High Level Hospital Clinical Research Funding, grant No. 2022-PUMCH-B-041
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial interest to declare in relation to the content of this article.
Ethical approval
This study was approved by the Institutional Review Board of the Peking Union Medical College Hospital (No. JS-2807) and conducted in accordance with the Declaration of Helsinki.
Informed Consent
All participants provided written consent for the use of their 2D and 3D facial images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, Y., Xia, Z., Shi, Y. et al. A Quantitative Three-Dimensional Tear Trough Deformity Assessment and Its Application in Orbital Septum Fat Transposition. Aesth Plast Surg 47, 2453–2460 (2023). https://doi.org/10.1007/s00266-023-03474-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03474-0