Abstract
Purpose
The aim was to investigate the contribution of robotics assisted total hip arthroplasty (THA) through direct anterior approach (DAA) in improving radiographic precision, functional results and complications.
Methods
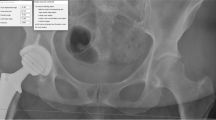
This retrospective study compared 100 primary conventional THA (cTHA) to 50 primary robotic THA (rTHA) through DAA. All cups were placed with the objective of having no anterior overhang while respecting the safe zones (SZ). Radiographic analysis included cup inclination and anteversion, vertical and horizontal changes of the rotation centre (ΔVCOR, ΔHCOR), acetabular and femoral offset. SZ were 30–50° of inclination and 10–30° of anteversion. Outliers were defined as medial displacement of the COR > 5 mm, vertical displacement of the COR > 3 mm superiorly. Harris hip score (HHS) and complications were compared at one year of follow-up.
Results
The robotic cups were better oriented with 98% in the global SZ versus 68% in the cTHA group (p = 0.0002). The COR was on average better restored in the robotic group in both the horizontal and vertical planes (Δ HCOR = − 5.0 ± 5.0 vs − 3.4 ± 4.9, p = 0.03; Δ VCOR = 1.6 ± 3.3 vs 0.2 ± 2.7, p = 0.04). There were fewer outliers in the rTHA group concerning VCOR (28% versus 10%, p = 0.03). There was no significant difference in HHS and complication rate at one year.
Conclusion
The use of robotics for THA by DAA provided an advantage in controlling the orientation of the cup and the restoration of its rotation centre. Thanks to the 3D planning on CT scan, it allowed to respect the thresholds while avoiding the anterior overhangs.







Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Batailler C, Fary C, Batailler P et al (2017) Total hip arthroplasty using direct anterior approach and dual mobility cup: safe and efficient strategy against post-operative dislocation. Int Orthop 41:499–506. https://doi.org/10.1007/s00264-016-3333-x
Free MD, Owen DH, Agius PA et al (2018) Direct anterior approach total hip arthroplasty: an adjunct to an enhanced recovery pathway: outcomes and learning curve effects in surgeons transitioning from other surgical approaches. J Arthroplasty 33:3490–3495. https://doi.org/10.1016/j.arth.2018.06.033
Homma Y, Baba T, Kobayashi H et al (2016) Safety in early experience with a direct anterior approach using fluoroscopic guidance with manual leg control for primary total hip arthroplasty: a consecutive one hundred and twenty case series. Int Orthop 40:2487–2494. https://doi.org/10.1007/s00264-016-3159-6
Foissey C, Fauvernier M, Fary C et al (2020) Total hip arthroplasty performed by direct anterior approach - Does experience influence the learning curve? SICOT-J 6:15. https://doi.org/10.1051/sicotj/2020015
Homma Y, Baba T, Sano K et al (2016) Lateral femoral cutaneous nerve injury with the direct anterior approach for total hip arthroplasty. Int Orthop 40:1587–1593. https://doi.org/10.1007/s00264-015-2942-0
Foissey C, Kenney R, Luceri F et al (2021) Greater trochanter fractures in the direct anterior approach: evolution during learning curve, risk factors and consequences. Arch Orthop Trauma Surg 141:675–681. https://doi.org/10.1007/s00402-020-03710-1
Foissey C, Fary C, Luceri F et al (2020) Transitioning the Total Hip Arthroplasty (THA) technique from posterior approach in lateral position to direct anterior approach in supine position - Risk Factors for acetabular malpositioning and the learning curve. Int Orthop. https://doi.org/10.1007/s00264-020-04583-0
Sharma AK, Cizmic Z, Dennis DA et al (2021) Low dislocation rates with the use of patient specific “Safe zones” in total hip arthroplasty. J Orthop 27:41–48. https://doi.org/10.1016/j.jor.2021.08.009
Marchetti E, Krantz N, Berton C et al (2011) Component impingement in total hip arthroplasty: Frequency and risk factors. A continuous retrieval analysis series of 416 cup. Orthop Traumatol Surg Res 97:127–133. https://doi.org/10.1016/j.otsr.2010.12.004
Batailler C, Bonin N, Wettstein M, null, et al (2017) Outcomes of cup revision for ilio-psoas impingement after total hip arthroplasty: Retrospective study of 46 patients. Orthop Traumatol Surg Res OTSR 103:1147–1153. https://doi.org/10.1016/j.otsr.2017.07.021
Cheung A, Yan CH, Fu H et al (2019) Ten- to sixteen-year follow-up of highly cross-linked polyethylene in total hip arthroplasty: what factors affect wear? J Arthroplasty 34:2016–2021. https://doi.org/10.1016/j.arth.2019.04.041
Myers CA, Laz PJ, Shelburne KB et al (2018) The impact of hip implant alignment on muscle and joint loading during dynamic activities. Clin Biomech 53:93–100. https://doi.org/10.1016/j.clinbiomech.2018.02.010
Ando W, Takao M, Hamada H et al (2021) Comparison of the accuracy of the cup position and orientation in total hip arthroplasty for osteoarthritis secondary to developmental dysplasia of the hip between the Mako robotic arm-assisted system and computed tomography-based navigation. Int Orthop 45:1719–1725. https://doi.org/10.1007/s00264-021-05015-3
Domb BG, Redmond JM, Louis SS et al (2015) Accuracy of component positioning in 1980 total hip arthroplasties: a comparative analysis by surgical technique and mode of guidance. J Arthroplasty 30:2208–2218. https://doi.org/10.1016/j.arth.2015.06.059
Han P-F, Chen C-L, Zhang Z-L et al (2019) Robotics-assisted versus conventional manual approaches for total hip arthroplasty: A systematic review and meta-analysis of comparative studies. Int J Med Robot Comput Assist Surg MRCAS 15:e1990. https://doi.org/10.1002/rcs.1990
Fontalis A, Kayani B, Thompson JW et al (2022) Robotic total hip arthroplasty: past, present and future. Orthop Trauma 36:6–13. https://doi.org/10.1016/j.mporth.2021.11.002
Kouyoumdjian P, Mansour J, Assi C et al (2020) Current concepts in robotic total hip arthroplasty. SICOT-J. 6:45. https://doi.org/10.1051/sicotj/2020041
Xu S, Bernardo LIC, Andy KS, Pang HN (2020) Robotic-Arm Assisted Direct Anterior Total Hip Arthroplasty Improving Implant Accuracy. Surg Technol Int 38:347–352. https://doi.org/10.52198/21.sti.38.os1368
Flecher X, Ollivier M, Argenson JN (2016) Lower limb length and offset in total hip arthroplasty. Orthop Traumatol Surg Res OTSR 102:S9-20. https://doi.org/10.1016/j.otsr.2015.11.001
Widmer K-H (2004) A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty 19:387–390. https://doi.org/10.1016/j.arth.2003.10.016
Kayani B, Konan S, Thakrar RR et al (2019) Assuring the long-term total joint arthroplasty. Bone Jt J 101-B:11–18. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0377.R1
McGoldrick NP, Antoniades S, El Meniawy S et al (2022) Supine versus lateral position for total hip replacement: accuracy of biomechanical reconstruction. Arch Orthop Trauma Surg 142:2945–2955. https://doi.org/10.1007/s00402-021-04179-2
Domb BG, El Bitar YF, Sadik AY et al (2014) Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop 472:329–336. https://doi.org/10.1007/s11999-013-3253-7
Ng N, Gaston P, Simpson PM et al (2021) Robotic arm-assisted versus manual total hip arthroplasty : a systematic review and meta-analysis. Bone Jt J 103-B(6):1009–1020. https://doi.org/10.1302/0301-620X.103B6.BJJ-2020-1856.R1
Kayani B, Konan S, Huq SS, et al (2019) The learning curve of robotic-arm assisted acetabular cup positioning during total hip arthroplasty. Hip Int J Clin Exp Res Hip Pathol Ther 1120700019889334https://doi.org/10.1177/1120700019889334
Pagkalos J, Chaudary MI, Davis ET (2014) Navigating the reaming of the acetabular cavity in total hip arthroplasty: does it improve implantation accuracy? J Arthroplasty 29:1749–1752. https://doi.org/10.1016/j.arth.2014.03.038
Yoder SA, Brand RA, Pedersen DR, O’Gorman TW (1988) Total hip acetabular component position affects component loosening rates. Clin Orthop. 228:79–87
Dastane M, Dorr LD, Tarwala R, Wan Z (2011) Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clin Orthop 469:429–436. https://doi.org/10.1007/s11999-010-1554-7
McGrory BJ, Morrey BF, Cahalan TD et al (1995) Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br 77:865–869
Lewinnek G, Lewis J, Tarr R et al (1978) Dislocations after total hip-replacement arthroplasties. J Bone Jt Surg 60:217–220
Callanan MC, Jarrett B, Bragdon CR et al (2011) The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop 469:319–329. https://doi.org/10.1007/s11999-010-1487-1
Atkinson HD, Johal KS, Willis-Owen C et al (2010) Differences in hip morphology between the sexes in patients undergoing hip resurfacing. J Orthop Surg 5:76. https://doi.org/10.1186/1749-799X-5-76
Bonnin MP, Archbold PHA, Basiglini L et al (2012) Do we medialise the hip centre of rotation in total hip arthroplasty? Influence of acetabular offset and surgical technique. HIP Int 22:371–378. https://doi.org/10.5301/HIP.2012.9350
Author information
Authors and Affiliations
Contributions
Constant Foissey: study design, data collection, statistical analysis, literature review and manuscript writing. Cécile Batailler: study design, manuscript editing. Remy Coulomb: study design, manuscript editing. Dia Eldean Giebaly: manuscript editing. Benoit Coulin: data collection. Sébastien Lustig: study design, supervision, literature review and manuscript editing. Pascal Kouyoumdjian: study design, supervision, literature review and manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Advisory Committee on Research Information Processing in the Field of Health (CCTIRS) approved this study on June 4, 2015 under number 15–430. For this type of study formal consent is not required.
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. CF, CB, RC and DEG declare that they have no conflict of interest. ES: Consultant for Corin. SL: Consultant for Stryker, Smith Nephew, Heraeus, Depuy Synthes; Institutional research support from Groupe Lepine, Amplitude; Editorial Board for Journal of Bone and Joint Surgery (Am), PK: Consultant for Stryker and for Lepine.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Foissey, C., Batailler, C., Coulomb, R. et al. Image-based robotic-assisted total hip arthroplasty through direct anterior approach allows a better orientation of the acetabular cup and a better restitution of the centre of rotation than a conventional procedure. International Orthopaedics (SICOT) 47, 691–699 (2023). https://doi.org/10.1007/s00264-022-05624-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05624-6