Abstract
Purpose
The platelet-to-lymphocyte ratio (PLR) has been extensively studied in various diseases. However, the relationship between PLR and hip fracture remains unknown. The aim of this study was to evaluate whether PLR would be an independent prognostic factor in elderly hip fracture patients.
Methods
Between January 2014 and December 2018, a retrospective cohort study was conducted in a orthopaedic centre, China. A total of 460 hip fracture patients were included. PLR was calculated as the ratio of platelet to lymphocyte counts and divided into high PLR group (≥ 189) and low PLR group (< 189) by using the receiver operating characteristic (ROC) curve. The relationship between PLR and one year all-cause mortality rate was assessed by univariate and multivariate Cox proportional hazard models. Further subgroup analysis stratified by different clinical and biological characteristics was performed to make the results more accurate.
Results
After a median follow-up of 32.0 months (range, 12.0–75.4), 92 patients (mortality rate: 20.0%) died within one year. PLR was significantly higher in dead patients compared with alive patients (p < 0.05), and high PLR group also had a high mortality rate (32.21% vs. 14.15%, p < 0.001). After multivariate adjustment, high PLR remained an independent predictor for one year all-cause mortality (adjusted hazard ratio (HR) 1.56, 95% confidence interval (CI) 1.02–2.41, p = 0.041). Moreover, advanced age (HR 1.05, 95% CI 1.01–1.08), male (HR 1.62, 95% CI 1.06–2.45), CCI ≥ 2 (HR 2.83, 95% CI 1.64–4.89), conservative treatment (HR 5.94, 95% CI 3.71–9.73), low haemoglobin level (HR 1.02, 95% CI 1.01–1.04), and low albumin level (HR 1.07, 95% CI 1.02–1.13) were independent risk factors for survival. Furthermore, subgroup analysis results were consistent with the main findings in most stratified groups.
Conclusion
This study highlights that high PLR (≥ 189) is associated with increased one year all-cause mortality in elderly hip fracture patients. As PLR is a simple indicator that can be calculated from the blood routine test, it can be easily performed in usual clinical practice.
Similar content being viewed by others
Introduction
Due to the high morbidity and mortality, hip fracture has become a major public health issue worldwide. A recent meta-analysis showed that the one year mortality rate was 13.96% after hip fracture in mainland China [1], and hip fracture was associated with excess short- and long-term all-cause mortality in Europe and USA [2]. At the same time, hip fracture incidence data suggested that hip fracture rates may be increasing in Poland [3], France [4], Japan [5], Italy [6], and China [7].
Recently, the relationship between inflammation and prognosis has attracted more attention. A study conducted by Norring-Agerskov et al. [8] found that the 30-day mortality after hip fracture was significantly associated with elevated levels of inflammation markers, such as C-reactive protein (CRP), soluble urokinase plasminogen activating receptor (suPAR), and ferritin. In addition, a series of studies have reported that many inflammation-based markers were directly related to poor prognosis or post-operative complications in patients with hip fracture, including prognostic nutritional index ratio (PNI) [9], CRP/PNI ratio [10], and neutrophil-to-lymphocyte ratio (NLR) [11, 12]. Platelet-to-lymphocyte ratio (PLR), a novel marker of systemic inflammation, has been reported to be closely related to the prognosis of many diseases, such as inflammatory diseases [13], cardiovascular disease [14], and various malignancies [15,16,17], even in the 2019-novel coronavirus disease (COVID-19) [18].
To our knowledge, elevated PLR was found to be significantly associated with increased all-cause mortality in general population, especially in the elderly [19]. However, none studies have examined the relationship between PLR and all-cause mortality in elderly hip fracture patients. Therefore, the aim of this study was to investigate the predictive value of PLR in elderly hip fracture patients.
Methods
Study design and patients
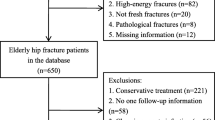
This retrospective cohort study was performed at the Orthopaedic Center of Deyang City, China. Consecutive patients with hip fracture who admitted to our department from January 2014 to December 2018 were initially considered. The inclusion criteria were as follows: (1) aged over 60 years; (2) diagnosis of hip fracture, including femur neck fracture and intertrochanteric fracture; (3) caused by a fall from no greater than standing height; and (4) fresh fracture less than three weeks. Patients who were either high-energy fractures or pathological fractures, lacked complete data, and failed to follow-up were excluded from the study. The study was approved by the Institutional Ethics Committee of Peoples’s Hospital of Deyang City, and written informed consents were obtained from patients or their immediate family members.
Data collection
Patient characteristics were gathered from the hospital records, including demogrphics (age, gender), fracture information (cause of fracture, fracture type, fracture location), comorbid diseases according to Charlson comorbidity index (CCI), and treatment details (surgery or conservative treatment, blood transfusion).
Blood tests were routinely measured for each patient on admission. We also collected laboratory data including platelet counts (× 109/L, reference range 100–300), lymphocyte counts (× 109/L, reference range 1.1–3.2), hemoglobin (g/L, reference range 130.0–175.0), albumin (g/L, reference range 35.0–55.0), and creatinine (μmol/L, reference range 53.0–106.0). The platelet-to-lymphocyte ratio (PLR) was calculated as the ratio of platelet to lymphocyte counts (PLR = platelet/lymphocyte counts). According to the World Health Organization (WHO) criteria, anemia was defined as hemoglobin level < 13.0 g/dL in men and < 12.0 g/dL in women. In addition, the albumin and creatinine levels were classified as follows: (1) albumin < 35.0 g/L and albumin ≥ 35.0 g/L and (2) creatinine ≤ 106.0 μmol/L and creatinine > 106.0 μmol/L.
Follow-up and study endpoint
Patients were telephonically followed up monthly for the first three months, and then every three months until the one year, and every six months thereafter. The outcome of this study was one year all-cause mortality, which was defined as the proportion of patients who died within 365 days after hospital admission. The follow-up time was defined as the period between hospital admission and date of death or the last follow-up time (December 31, 2019).
Statistical analysis
Continous variables were expressed as means ± standard deviation (SD) or median (interquartile range, IQR) according to the distribution. The Shapiro–Wilk test was used to assess normal distribution. Differences between groups were analyzed using the independent Student’s t test for normally distributed variables, and Wilcoxon rank-sum test for non-normally distributed variables. Categorical variables were shown as frequencies (percentages), and compared by χ2 test. Receiver operating characteristic (ROC) curves were used to determine the optimal cut-off values for the platelet, lymphocyte, and PLR, and then divided into high or low group. Survival was estimated using the Kaplan–Meier method, and the differences between groups were assessed using the log-rank test. After adjusting for significant variables identified by univariate analysis (p < 0.10), multivariate Cox proportional hazard model was performed to calculate hazard ratio (HR) and 95% confidence interval (CI) for risk of mortality. We also conducted subgroup analyses for each stratified groups of age, gender, hypertension, anaemia, CCI, hip fracture type, treatment, blood transfusion, and albumin level. For the subgroup analysis, we did not perform multivariable adjustment due to a very small number of events. All statistical analyses were performed using JMP Pro software (version 13.0.0; SAS Institute Inc., Cary, NC, USA), and a p < 0.05 was considered statistically significant.
Results
Patient characteristics
A total of 460 hip fracture patients were included in this study, and the patient characteristics are summarized in Table 1. Of these participants, the average age was 79.31 years, and women made up the majority of the patients (66.96%). With respect to comorbid diseases, 70.43% had anemia, 36.52% had hypertension, and the proportions of none (CCI = 0), low (CCI = 1) and high comorbidity (CCI ≥ 2) were 48.91%, 33.04%, and 18.04%, respectively. Additionally, 47.61% were intertrochanteric fracture, 73.04% underwent surgery, and 18.26% received red blood cells transfusion. Laboratory data showed that the median values of platlet, lymphocyte, and PLR were 141.50, 0.98, and 143.96, respectively. During the median follow-up time of 32.0 months (range, 12.0–75.4), 92 cases (mortality rate: 20.00%) died within 1 year.
According to the ROC curves (Fig. 1), the optimal cut-off value was 177.0 for platelet counts (sensitivity 44.57%, specificity 72.55%), 0.93 for lymphocyte counts (sensitivity 60.87%, specificity 57.61%), and 189.0 for PLR (sensitivity 52.17%, specificity 72.55%). As expected, the area under curve (AUC) of PLR (AUC 0.61, 95% CI 0.54–0.68) was slightly larger than platelet (AUC 0.57, 95% CI 0.50–0.64) and lymphocyte (AUC 0.59, 95% CI 0.43–0.66).
As shown in Table 1, the high PLR patients (PLR ≥ 189) were more likely to be older age, intertrochanteric fracture, receiving conservative treatment, lower haemoglobin, and albumin levels (all p < 0.05). Likewise, the one year mortality rate was significantly higher in the high PLR group compared with the low PLR group (32.21% vs. 14.15%, p < 0.001). Consistently, deceased patients had significantly higher platelet counts (154.0 (111.3–211.3) vs. 140.0 (104.0–185.85), p = 0.041), and PLR level (190.5 (115.9–270.3) vs. 139.0 (103.7–198.0), p = 0.001), and lower lymphocyte counts (0.8 (0.6–1.2) vs. 1.0 (0.7–1.3), p = 0.007) than alive patients (Fig. 2).
Violin plots comparing platelet counts, lymphocyte counts, and platelet-to-lymphocyte ratio between alive and dead patients. The horizontal lines within the violin represent the median; the boxes represent the interquartile range; the bars represent the 95% confidence intervals; the width of the shapes represent the density of distribution. Differences between groups were analyzed by Wilcoxon rank-sum test
Clinical variables predicting one year mortality
The relationships between clinical variables and 1-year mortality are listed in Table 2. In univariate analysis, older age, male, CCI ≥ 1, undergoing conservative treatment, low haemoglobin level, high platelet counts (≥ 177 × 109/L), low lymphocyte counts (< 0.93 × 109/L), high PLR (≥ 189), low albumin level, and high creatinine (> 106.0 μmol/L) were significantly associated with the increased one year mortality. Consistent with this result, log-rank test of the Kaplan–Meier curves also showed that patients with high platelet counts and PLR level, as well as low lymphocyte had worse one year mortality (Fig. 3).
Kaplan–Meier survival analyses of elderly hip fracture patients according to platelet counts, lymphocyte counts and platelet-to-lymphocyte ratio (PLR). Hazard ratio (HR) was calculated using a Cox regression analysis, and p value was estimated using the log-rank test, and the shaded areas indicate 95% confidence interval (CI). The numbers shown below the Kaplan–Meier survival curves are the number of patients at risk at the specified month for each group
As PLR includes platelet and lymphocyte counts, they were not entered into the multivariate Cox proportional hazard model. After inclusion of significant factors in the multivariate analysis to adjust the effects of covariates, high PLR (adjusted HR 1.55, 95% CI 1.01–2.39) remained an independent prognostic factor for predicting the prognosis. In addition, advanced age (HR 1.05, 95% CI 1.01–1.08), male (HR 1.62, 95% CI 1.06–2.45), CCI ≥ 2 (HR 2.83, 95% CI 1.64–4.89), conservative treatment (HR 5.94, 95% CI 3.71–9.73), low haemoglobin level (HR 1.02, 95% CI 1.01–1.04), and low albumin level (HR 1.07, 95% CI 1.02–1.13) were independent risk factors for one year mortality.
Subgroup analysis
To further verify whether the predictive value of PLR was consistent among different populations, we performed a subgroup analysis using forest plot, as shown in Fig. 4. Consistent with the main analysis, the subgroup analysis revealed that high PLR was significantly associated with increased one year mortality in most subgroups (p < 0.05), except for only three subgroups including patients without anaemia (p = 0.115), albumin level < 35 g/L (p = 0.088), and creatine level > 106 μmol/L (p = 0.132).
Forest plot of the subgroup analysis estimating the association between platelet-to-lymphocyte ratio (PLR) and 1-year mortality based on different characteristics. Differences between subgroups were analyzed the Cox regression analysis. The purple squares represent the effect size [hazard ratio (HR)], and the black horizontal lines represent 95% confidence interval (CI)
Discussion
Systemic inflammation is associated with many orthopaedic diseases, such as periprosthetic joint infection [20, 21], and surgical site infection [22, 23]. PLR is a simple inflammatory marker that does not need any additional laboratory testing, and easily calculated by the platelet count/lymphocyte count formula. According to several population-based cohort studies, increased platelet counts had a significant association with mortality, risk of cardiovascular disease, and dementia [24,25,26]. In patients with hip fracture, Galivanche et al. [27] reported that high platelet counts were a risk factor for developing a post-operative pressure ulcer. On the other hand, total lymphocyte count (TLC) is considered to be a nutritional marker, and 62.6% of hip fracture patients were malnourished as defined by TLC blew 1500 cells per cubic millimeter [28]. A recent meta analysis also suggested that lower lymphocyte counts were closely related to a higher mortality after hip fracture surgery [29]. As such, we hypothesized that elevated PLR level by raising platelet counts and/or lowering lymphocyte counts may contribute to poor prognosis in elderly patients with a hip fracture.
To our best knowledge, this is the first study showing a clear association between PLR and mortality in elderly hip fracture patients. We found that high PLR (≥ 189) had an increased one year mortality rate, with a 18.06% higher than patients with low PLR (< 189). Likewise, deceased patients had significantly higher platelet counts and PLR level, and lower lymphocyte counts than alive patients. Similar to our study, Mathur et al. [19] observed that mean PLR was significantly higher in general population who died than those who were living, and participants in the fourth quartile of PLR were at significantly higher risk of mortality than those in the first quartile (19.8 vs. 13.9 per 1000 person-years).
In univariate analysis, our current results revealed that older age, male, CCI ≥ 1, undergoing conservative treatment, low haemoglobin and albumin level, and high creatinine level were significantly associated with the increased one year mortality. These risk factors associated with the poor prognosis after hip fracture has been confirmed in the previous studies [30, 31]. Although blood transfusion was associated with mortality after hip fracture in some studies [32, 33], no such relationship was found in our data. We speculated that the possible reason was that the number of patients receiving blood transfusion were small (n = 84 in our study), which may influence this relationship. After adjustment with other factors in multivariate analysis, older age, male, CCI ≥ 2, conservative treatment, low haemoglobin, and albumin levels were independent risk factors for one year mortality, which were consistent with other studies [30, 31]. Notably, high PLR remained an independent prognostic factor for predicting the prognosis (adjusted HR 1.55; 95% CI 1.01–2.39). However, high creatinine level lost statistical significance in the multivariate analysis, but there was a trend toward significance (p = 0.075). This might be due to an insufficient sample size of patients with high creatinine level (n = 57 in our study), although we had a relatively large overall sample.
In addition, previous study pointed out that the value of PLR varied with age and sex [34], we therefore performed a subgroup analysis to verify whether the predictive value of PLR was consistent among different populations. The subgroup analysis also confirmed that the relationship between PLR and mortality remained stable across all the age groups, as well as male or female subgroups. Of note, this relationship existed in other subgroups, including patients with femoral neck or intertrochanteric fracture, undergoing surgery or conservative treatment, and receiving blood transfusion or not. Although several studies have confirmed that a low serum albumin level was negatively correlated with the risk of post-operative complications and total mortality in patients with hip fracture [29], our study found that the predictive value of PLR did not reach statistical significance in subgroup patients with hypoalbuminemia (albumin level < 35.0 g/L). It is noteworthy that there was such a trend toward lower mortality (p = 0.088). Similarly, patients with high creatinine level (> 106 μmol/L) failed to achieve statistical significance (p = 0.132). This finding was consistent with prior research that only high PLR level over 311 had a higher risk of death in older patients with acute kidney injury [35].
Although high PLR level has been reported to be closely related to a poor prognosis of many diseases, the possible mechanism of this predictive ability is not clear so far. Herein, we assumed the following factors may account for it. First, hip fractures occur commonly in the elderly, and the average age was 79.31 years in our study. A recent study has demonstrated that elevated PLR was associated with increased all-cause mortality in the elderly but not in the middle age or younger participants [19]. Second, about 34.08% elderly hip fracture patients suffered chronic obstructive pulmonary disease (COPD) [36], and high PLR was significantly associated with both hospital mortality and 90-day mortality in patients with COPD [30, 37]. Third, elderly hip fracture patients are even more prone to complications, such as pneumonia [38], deep vein thrombosis [39], and heart failure [40]. These factors are closely related to a worse prognosis of hip fracture, and high PLR level was associated with a poor prognosis in patients with these diseases [18, 41, 42]. Additionally, PLR was observed to be significant association with deep vein thrombosis after total joint arthroplasty [43].
However, this study had several limitations. First, the PLR level was recorded only at time of admission to hospital, which limited us to explore the relationship of the change of PLR over time after hip fracture. Second, the current study was a single-center retrospective study, and additional large-scale clinical cohorts are needed to confirm these findings. Finally, we are unable to assess the short-term prognosis of PLR due to a relatively small number of deaths.
Conclusion
This study highlights that elevated PLR (≥ 189) is associated with increased one year all-cause mortality in elderly hip fracture patients. As PLR is a simple indicator that can be calculated from the blood routine test, it can be easily performed in usual clinical practice.
Data availability
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cui Z, Feng H, Meng X, Zhuang S, Liu Z, Ye K, Sun C, Xing Y, Zhou F, Tian Y (2019) Age-specific 1-year mortality rates after hip fracture based on the populations in mainland China between the years 2000 and 2018: a systematic analysis. Arch Osteoporos 14(1):55. https://doi.org/10.1007/s11657-019-0604-3
Katsoulis M, Benetou V, Karapetyan T, Feskanich D, Grodstein F, Pettersson-Kymmer U, Eriksson S, Wilsgaard T, Jørgensen L, Ahmed LA, Schöttker B, Brenner H, Bellavia A, Wolk A, Kubinova R, Stegeman B, Bobak M, Boffetta P, Trichopoulou A (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med 281(3):300–310. https://doi.org/10.1111/joim.12586
Glinkowski W, Narloch J, Krasuski K, Śliwczyński A (2019) The increase of osteoporotic hip fractures and associated one-year mortality in Poland: 2008–2015. J Clin Med 8(9). https://doi.org/10.3390/jcm8091487
Garofoli R, Maravic M, Ostertag A, Cohen-Solal M (2019) Secular trends of hip fractures in France: impact of changing characteristics of the background population. Osteoporos Int 30(2):355–362. https://doi.org/10.1007/s00198-018-4666-7
Tamaki J, Fujimori K, Ikehara S, Kamiya K, Nakatoh S, Okimoto N, Ogawa S, Ishii S, Iki M (2019) Estimates of hip fracture incidence in Japan using the National Health Insurance Claim Database in 2012-2015. Osteoporos Int 30(5):975–983. https://doi.org/10.1007/s00198-019-04844-8
Piscitelli P, Feola M, Rao C, Neglia C, Rizzo E, Vigilanza A, Rivezzi M, Faccilongo N, Contò F, Distante A, Tarantino U (2019) Incidence and costs of hip fractures in elderly Italian population: first regional-based assessment. Arch Osteoporos 14(1):81. https://doi.org/10.1007/s11657-019-0619-9
Tian FM, Sun XX, Liu JY, Liu ZK, Liang CY, Zhang L (2017) Unparallel gender-specific changes in the incidence of hip fractures in Tangshan, China. Arch Osteoporos 12(1):18. https://doi.org/10.1007/s11657-017-0313-8
Norring-Agerskov D, Bathum L, Pedersen OB, Abrahamsen B, Lauritzen JB, Jørgensen NR, Jørgensen HL (2019) Biochemical markers of inflammation are associated with increased mortality in hip fracture patients: the Bispebjerg Hip Fracture Biobank. Aging Clin Exp Res 31(12):1727–1734. https://doi.org/10.1007/s40520-019-01140-7
Xing H, Xiang D, Li Y, Ji X, Xie G (2020) Preoperative prognostic nutritional index predicts postoperative delirium in elderly patients after hip fracture surgery. Psychogeriatrics. https://doi.org/10.1111/psyg.12511
Ren H, Wu L, Hu W, Ye X, Yu B (2017) Prognostic value of the c-reactive protein/prognostic nutritional index ratio after hip fracture surgery in the elderly population. Oncotarget 8(37):61365–61372. https://doi.org/10.18632/oncotarget.18135
Fisher A, Srikusalanukul W, Fisher L, Smith P (2016) The neutrophil to lymphocyte ratio on admission and short-term outcomes in orthogeriatric patients. Int J Med Sci 13(8):588–602. https://doi.org/10.7150/ijms.15445
Forget P, Moreau N, Engel H, Cornu O, Boland B, De Kock M, Yombi JC (2015) The neutrophil-to-lymphocyte ratio (NLR) after surgery for hip fracture (HF). Arch Gerontol Geriatr 60(2):366–371. https://doi.org/10.1016/j.archger.2014.11.008
Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD (2019) The platelet-to-lymphocyte ratio as an inflammatory marker in rheumatic diseases. Ann Lab Med 39(4):345–357. https://doi.org/10.3343/alm.2019.39.4.345
Kurtul A, Ornek E (2019) Platelet to lymphocyte ratio in cardiovascular diseases: a systematic review. Angiology 70(9):802–818. https://doi.org/10.1177/0003319719845186
Chang WL, Yang WC, Zeng XY, Li CG, Xiong Z, Wang T, Zhang RZ, Tao KX, Zhang P (2020) Elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis of patients with primary gastrointestinal stromal tumor. BMC Gastroenterol 20(1):124. https://doi.org/10.1186/s12876-020-01275-2
Shi M, Zhao W, Zhou F, Chen H, Tang L, Su B, Zhang J (2020) Neutrophil or platelet-to-lymphocyte ratios in blood are associated with poor prognosis of pulmonary large cell neuroendocrine carcinoma. Transl Lung Cancer Res 9(1):45–54. https://doi.org/10.21037/tlcr.2020.01.17
Li LQ, Bai ZH, Zhang LH, Zhang Y, Lu XC, Zhang Y, Liu YK, Wen J, Li JZ (2020) Meta-analysis of hematological biomarkers as reliable indicators of soft tissue sarcoma prognosis. Front Oncol 10:30. https://doi.org/10.3389/fonc.2020.00030
Qu R, Ling Y, Zhang YH, Wei LY, Chen X, Li XM, Liu XY, Liu HM, Guo Z, Ren H, Wang Q (2020) Platelet-to-lymphocyte ratio is associated with prognosis in patients with coronavirus disease-19. J Med Virol. https://doi.org/10.1002/jmv.25767
Mathur K, Kurbanova N, Qayyum R (2019) Platelet-lymphocyte ratio (PLR) and all-cause mortality in general population: insights from national health and nutrition education survey. Platelets 30(8):1036–1041. https://doi.org/10.1080/09537104.2019.1571188
Klim SM, Amerstorfer F, Glehr G, Hauer G, Smolle MA, Leitner L, Leithner A, Glehr M (2020) Combined serum biomarker analysis shows no benefit in the diagnosis of periprosthetic joint infection. Int Orthop. https://doi.org/10.1007/s00264-020-04731-6
Ettinger M, Savov P, Calliess T, Windhagen H, Lichtinghagen R, Lukasz A, Omar M (2020) Improved diagnostic accuracy with the classification tree method for diagnosing low-grade periprosthetic joint infections by quantitative measurement of synovial fluid alpha-defensin and C-reactive protein. Int Orthop 44(1):31–38. https://doi.org/10.1007/s00264-019-04338-6
Zheng S, Wang Z, Qin S, Chen JT (2020) Usefulness of inflammatory markers and clinical manifestation for an earlier method to diagnosis surgical site infection after spinal surgery. Int Orthop. https://doi.org/10.1007/s00264-020-04567-0
Pawłowska I, Ziółkowski G, Wójkowska-Mach J, Bielecki T (2019) Can surgical site infections be controlled through microbiological surveillance? A three-year laboratory-based surveillance at an orthopaedic unit, retrospective observatory study. Int Orthop 43(9):2009–2016. https://doi.org/10.1007/s00264-019-04298-x
Vinholt PJ, Hvas AM, Frederiksen H, Bathum L, Jørgensen MK, Nybo M (2016) Platelet count is associated with cardiovascular disease, cancer and mortality: a population-based cohort study. Thromb Res 148:136–142. https://doi.org/10.1016/j.thromres.2016.08.012
Patti G, Di Martino G, Ricci F, Renda G, Gallina S, Hamrefors V, Melander O, Sutton R, Engström G, De Caterina R, Fedorowski A (2019) Platelet indices and risk of death and cardiovascular events: results from a large population-based cohort study. J Thromb Haemost 119(11):1773–1784. https://doi.org/10.1055/s-0039-1694969
van der Willik KD, Fani L, Rizopoulos D, Licher S, Fest J, Schagen SB, Ikram MK, Ikram MA (2019) Balance between innate versus adaptive immune system and the risk of dementia: a population-based cohort study. J Neuroinflammation 16(1):68. https://doi.org/10.1186/s12974-019-1454-z
Galivanche AR, Kebaish KJ, Adrados M, Ottesen TD, Varthi AG, Rubin LE, Grauer JN (2020) Postoperative pressure ulcers after geriatric hip fracture surgery are predicted by defined preoperative comorbidities and postoperative complications. J Am Acad Orthop Surg 28(8):342–351. https://doi.org/10.5435/jaaos-d-19-00104
Wilson JM, Boissonneault AR, Schwartz AM, Staley CA, Schenker ML (2019) Frailty and malnutrition are associated with inpatient postoperative complications and mortality in hip fracture patients. J Orthop Trauma 33(3):143–148. https://doi.org/10.1097/bot.0000000000001386
Li S, Zhang J, Zheng H, Wang X, Liu Z, Sun T (2019) Prognostic role of serum albumin, Total lymphocyte count, and mini nutritional assessment on outcomes after geriatric hip fracture surgery: a Meta-analysis and systematic review. J Arthroplast 34(6):1287–1296. https://doi.org/10.1016/j.arth.2019.02.003
Kumar P, Law S, Sriram KB (2017) Evaluation of platelet lymphocyte ratio and 90-day mortality in patients with acute exacerbation of chronic obstructive pulmonary disease. J Thorac Dis 9(6):1509–1516. https://doi.org/10.21037/jtd.2017.05.77
Liu Y, Wang Z, Xiao W (2018) Risk factors for mortality in elderly patients with hip fractures: a meta-analysis of 18 studies. Aging Clin Exp Res 30(4):323–330. https://doi.org/10.1007/s40520-017-0789-5
Puckeridge G, Terblanche M, Wallis M, Fung YL (2019) Blood management in hip fractures; are we leaving it too late? A retrospective observational study. BMC Geriatr 19(1):79. https://doi.org/10.1186/s12877-019-1099-x
Arshi A, Lai WC, Iglesias BC, McPherson EJ, Zeegen EN, Stavrakis AI, Sassoon AA (2020) Blood transfusion rates and predictors following geriatric hip fracture surgery. Hip Int:1120700019897878. https://doi.org/10.1177/1120700019897878
Wu L, Zou S, Wang C, Tan X, Yu M (2019) Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio in Chinese Han population from Chaoshan region in South China. BMC Cardiovasc Disord 19(1):125. https://doi.org/10.1186/s12872-019-1110-7
Zheng CF, Liu WY, Zeng FF, Zheng MH, Shi HY, Zhou Y, Pan JY (2017) Prognostic value of platelet-to-lymphocyte ratios among critically ill patients with acute kidney injury. Crit Care 21(1):238. https://doi.org/10.1186/s13054-017-1821-z
Cha YH, Ha YC, Park HJ, Lee YK, Jung SY, Kim JY, Koo KH (2019) Relationship of chronic obstructive pulmonary disease severity with early and late mortality in elderly patients with hip fracture. Injury 50(9):1529–1533. https://doi.org/10.1016/j.injury.2019.05.021
Yao C, Liu X, Tang Z (2017) Prognostic role of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio for hospital mortality in patients with AECOPD. Int J Chron Obstruct Pulmon Dis 12:2285–2290. https://doi.org/10.2147/copd.s141760
Byun SE, Shon HC, Kim JW, Kim HK, Sim Y (2019) Risk factors and prognostic implications of aspiration pneumonia in older hip fracture patients: a multicenter retrospective analysis. Geriatr Gerontol Int 19(2):119–123. https://doi.org/10.1111/ggi.13559
Zhang BF, Wei X, Huang H, Wang PF, Liu P, Qu SW, Li JH, Wang H, Cong YX, Zhuang Y, Zhang K (2018) Deep vein thrombosis in bilateral lower extremities after hip fracture: a retrospective study of 463 patients. Clin Interv Aging 13:681–689. https://doi.org/10.2147/cia.s161191
Cha YH, Ha YC, Ryu HJ, Lee YK, Park SH, Lee KJ, Koo KH (2020) Effect of heart failure on postoperative short and long-term mortality in elderly patients with hip fracture. Injury 51(3):694–698. https://doi.org/10.1016/j.injury.2020.01.004
Kuplay H, Erdoğan SB, Bastopcu M, Arslanhan G, Baykan DB, Orhan G (2020) The neutrophil-lymphocyte ratio and the platelet-lymphocyte ratio correlate with thrombus burden in deep venous thrombosis. J Vasc Surg Venous Lymphat Disord 8(3):360–364. https://doi.org/10.1016/j.jvsv.2019.05.007
Pourafkari L, Wang CK, Tajlil A, Afshar AH, Schwartz M, Nader ND (2018) Platelet-lymphocyte ratio in prediction of outcome of acute heart failure. Biomark Med 12(1):63–70. https://doi.org/10.2217/bmm-2017-0193
Yao C, Zhang Z, Yao Y, Xu X, Jiang Q, Shi D (2018) Predictive value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio for acute deep vein thrombosis after total joint arthroplasty: a retrospective study. J Orthop Surg Res 13(1):40. https://doi.org/10.1186/s13018-018-0745-x
Acknowledgements
We would like to thank several nurses from the Department of Orthopedic Surgery in People’s Hospital of Deyang City, for the help with the data inspection.
Funding
This research was funded by Deyang Science and Technology Breau (2019SZ125).
Author information
Authors and Affiliations
Contributions
Yuehong Liu designed the research and revised the manuscript. Zhicong Wang and Hong Wang contributed to analysis and drafting the manuscript. Ling Yang, Xi Chen, and Wei Jiang participated in data collection and patients’ follow-up. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study protocol was approved by the Institutional Ethics Committee of Peoples’s Hospital of Deyang City. This study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Z., Wang, H., Yang, L. et al. High platelet-to-lymphocyte ratio predicts poor survival of elderly patients with hip fracture. International Orthopaedics (SICOT) 45, 13–21 (2021). https://doi.org/10.1007/s00264-020-04833-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04833-1