Abstract
Purpose
Cartilage lesions are usually accompanied by subchondral bone alterations or bone marrow lesions (BMLs). BML associated with joint degeneration and cartilage lesions are considered to be predictors of rapidly progressing OA. Currently no existing treatment can fully halt OA progression. One of the approaches is an autologous, biological treatment based on the use of platelet rich plasma (PRP) injections. The purpose of this study is to assess the short-term effectiveness of intraosseous PRP injections, within the BML of individuals affected by OA, in ameliorating pain and improving knee functionality.
Materials and methods
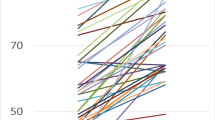
The study involved 17 patients with an average age of 41.7 ± 14.3 years old. OA stage was determined using the Kellgren-Lawrence grading system by performing radiographic scanning of the knee joint before surgical intervention. Patients with K–L grade 3 knee joint OA prevailed. Patient OA history varied between one and nine years (average 5.2 ± 4.5 years). Clinical and functional state of the knee were assessed by pain visual analogue scale (VAS) score, the Western Ontario and McMaster Universities Score (WOMAC), and the Knee Injury and Osteoarthritis Outcome Score (KOOS) which were filled out by patients previous to the surgical procedure at one, three, six and 12 months post-operatively. Before surgery, in addition to standard blood tests, serum cartilage oligomeric matrix protein (COMP) levels were tested for all patients.
Results
Evaluation of preliminary results revealed a statistically significant reduction of pain based on the VAS score. A significant improvement was also observed in the patients’ WOMAC score and in the overall KOOS score. Serum marker levels were initially elevated in our experimental patient group compared to the same marker in healthy control respondents, and continued to rise one month and three months following surgery, at six and 12 month the level was similar as at three months.
Conclusions
In our opinion, first COMP increasing can be caused by injection of platelet rich plasma. It is not adequate to interpret this growth in COMP levels as increased osteochondral degeneration. One year follow-up period showed good quality of life improvement, significant pain reduction, and essential MRI changes. The long-term observation of these cohort of patients combined with an analysis of MRI images is still ongoing.




Similar content being viewed by others
References
Delgado D, Garate A, Hunter V, Bilbao A, Patel R, Fiz AS, Sampson S, Sanchez M (2019) Current concepts in intraosseous platelet-rich plasma injections for knee osteoarthritis. J Clin Orthopaedics Trauma 10:36–41
Madry H, van Dijk CN, Mueller-Gerbl M (2010) The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc 18:419–433
Li et al (2013) Subchondral bone in osteoarthritis: insight into risk factors and microstructural changes. Arthritis Res Ther 15:223. https://doi.org/10.1186/ar4405
Kon E, Ronga M, Filardo G, Farr G, Madry H, Milano G, Andriolo L, Shabshin N (2016) Bone marrow lesions and subchondral bone pathology of the knee. Knee Surg Sports Traumatol Arthrosc 24(6):1797–1814. https://doi.org/10.1007/s00167-016-4113-2
Appel H, Kuhne M, Spiekermann S, Kohler D, Zacher J, Stein H et al (2006) Immunohistochemical analysis of hip arthritis in ankylosing spondylitis: evaluation of the bone-cartilage interface and subchondral bone marrow. Arthritis Rheum 54:1805–1813
Pelletier JP (2007) Risk factors associated with the loss of cartilage volume on weight-bearing areas in knee osteoarthritis patients assessed by quantitative magnetic resonance imaging: a longitudinal study. Arthritis Res Ther 9(4):R74
Zhao J, Li X, Bolbos RI, Link TM, Majumdar S (2010) Longitudinal assessment of bone marrow edema-like lesions and cartilage degeneration in osteoarthritis using 3 T MR T1rho quantification. Skelet Radiol 39:523–531
Wilson AJ, Murphy WA, Hardy DC, Totty WG (1988) Transient osteoporosis: transient bone marrow edema? Radiology 167:757–760
Felson DT, McLaughlin S, Goggins J, LaValley MP, Gale ME, Totterman S, Li W, Hill C, Gale D (2003) Bone marrow edema and its relation to progression of knee osteoarthritis. Ann Intern Med 139:330–336
Perry T, O'Neill T, Parkes M, Felson DT, Hodgson R, Arden NK (2018) Bone marrow lesion type and pain in knee osteoarthritis. Ann Rheum Dis 77:1145
Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N et al (2003) Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology 226:373–381
Roemer FW, Frobell R, Hunter DJ, Crema MD, Fischer W, Bohndorf K et al (2009) MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthr Cartil 17:1115–1131
Roemer FW et al (2010) Subchondral bone marrow lesions are highly associated with, and predict subchondral bone attrition longitudinally: the MOST study. Osteoarthr Cartil 18(1):47–53
Peterfy CG et al (2004) Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthr Cartil 12(3):177–190
Abhishek A, Doherty M (2013) Diagnosis and clinical presentation of osteoarthritis. Rheum Dis Clin N Am 39(1):45–66. https://doi.org/10.1016/j.rdc.2012.10.007
Mayerhoefer ME, Breitenseher MJ, Kramer J, Aigner N, Norden C, Hofmann S (2005) STIR vs. T1- weighted fat-suppressed gadolinium-enhanced MRI of bone marrow edema of the knee: computer-assisted quantitative comparison and influence of injected contrast media volume and acquisition parameters. J Magn Reson Imaging 22:788–793
McAlindon TE, Watt I, McCrae F, Goddard P, Dieppe PA (1991) Magnetic resonance imaging in osteoarthritis of the knee: correlation with radiographic and scintigraphic findings. Ann Rheum Dis 50:14–19
Ahlback S, Bauer GC, Bohne WH (1968) Spontaneous osteonecrosis of the knee. Arthritis Rheum 11(6):705–733
Wluka AE, Hanna F, Davies-Tuck M, Wang Y, Bell RJ, Davis SR, Adams J, Cicuttini FM (2009) Bone marrow lesions predict increase in knee cartilage defects and loss of cartilage volume in middle-aged women without knee pain over 2 years. Ann Rheum Dis 68:850–855
Odding E et al (1998) Associations of radiological osteoarthritis of the hip and knee with locomotor disability in the Rotterdam study. Ann Rheum Dis 57(4):203–208
Sowers MF et al (2003) Magnetic resonance-detected subchondral bone marrow and cartilage defect characteristics associated with pain and X-ray-defined knee osteoarthritis. Osteoarthr Cartil 11(6):387–393
Hunter DJ, Gerstenfeld L, Bishop G, Davis AD, Mason ZD, Einhorn TA, Maciewicz RA, Newham P, Foster M, Jackson S, Morgan EF (2009) Bone marrow lesions from osteoarthritis knees are characterized by sclerotic bone that is less well mineralized. Arthritis Res Ther 11:R11
Manicourt DH, Brasseur JP, Boutsen Y, Depreseux G, Devogelaer JP (2004) Role of alendronate in therapy for posttraumatic complex regional pain syndrome type I of the lower extremity. Arthritis Rheum 50:3690–3697
Lecouvet FE, van de Berg BC, Maldague BE, Lebon CJ, Jamart J, Saleh M, Noel H, Malghem J (1988) Early irreversible osteonecrosis versus transient lesions of the femoral condyles: prognostic value of subchondral bone and marrow changes on MR imaging. AJR Am J Roentgenol 170:71–77
Carrino JA, Blum J, Parellada JA, Schweitzer ME, Morrison WB (2006) MRI of bone marrow edema-like signal in the pathogenesis of subchondral cysts. Osteoarthr Cartil 14:1081–1085
Radke S, Rader C, Kenn W, Kirschner S, Walther M, Eulert J (2003) Transient marrow edema syndrome of the hip: results after core decompression. A prospective MRI-controlled study in 22 patients. Arch Orthop Trauma 123:223–227
Kohn MD, Sassoon AA, Fernando ND (2016) Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res 474(8):1886–1893. https://doi.org/10.1007/S11999-016-4732-4
Marot V, Murgier J, Carrozzo A, Reina N, Monaco E, Chiron P, Berard E, Cavaignac E (2019) Determination of normal KOOS and WOMAC values in a healthy population. Knee Surg Sports Traumatol Arthrosc 27(2):541–548. https://doi.org/10.1007/s00167-018-5153-6
Bellido M, Lugo L, Roman-Blas JA et al (2011) Improving subchondral bone integrity reduces progression of cartilage damage in experimental osteoarthritis preceded by osteoporosis. Osteoarthr Cartil 19(10):1228–1236
Vasina EM, Cauwenberghs S, Feijge MA, Heemskerk JW, Weber C, Koenen RR (2011) Microparticles from apoptotic platelets promote resident macrophage differentiation. Cell Death Dis 2:211
Liu-Bryan R, Terkeltaub R (2015) Emerging regulators of the inflammatory process in osteoarthritis. Nat Rev Rheumatol 11(1):35–44
Tohidnezhad M, Wruck CJ, Slowik A et al (2014) Role of platelet-released growth factors in detoxification of reactive oxygen species in osteoblasts. Bone 65:9–17
Cohen SB, Sharkey PF (2016) Subchondroplasty for treating bone marrow lesions. J Knee Surg 29(7):555–563
Bonadio MB, Giglio PN, Helito CP, Pécora JR, Camanho GL, Demange MK (2017) Subchondroplasty for treating bone marrow lesions in the knee - initial experience. Rev Bras Ortop 52(3):325–330. https://doi.org/10.1016/j.rboe.2017.04.003
Marcacci M, Filardo G, Kon E (2013) Treatment of cartilage lesions: what works and why? Injury 44(Suppl. 1):S11–S15
Bi X (2018) Correlation of serum cartilage oligomeric matrix protein with knee osteoarthritis diagnosis: a meta-analysis. J Orthop Surg Res 13(1):262. https://doi.org/10.1186/s13018-018-0959-y
Hao HQ, Zhang JF, He QQ, Wang Z (2019) Cartilage oligomeric matrix protein, C-terminal cross-linking telopeptide of type II collagen, and matrix metalloproteinase-3 as biomarkers for knee and hip osteoarthritis (OA) diagnosis: a systematic review and meta-analysis. Osteoarthr Cartil 27(5):726–736. https://doi.org/10.1016/j.joca.2018.10.009
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration ant its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lychagin, A., Lipina, M., Garkavi, A. et al. Intraosseous injections of platelet rich plasma for knee bone marrow lesions treatment: one year follow-up. International Orthopaedics (SICOT) 45, 355–363 (2021). https://doi.org/10.1007/s00264-020-04546-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04546-5