Abstract
Purpose
Six different mono-axial and poly-axial distal humeral plating systems with an anatomical plate design were compared. The aim of the biomechanical tests was to examine differences regarding system stiffness, median fatigue limit, and failure mechanisms.
Methods
Different configurations of two double plate fixation systems by two manufacturers for the treatment of complex distal humeral fractures (AO/OTA type C2.3) were biomechanically tested in a physiologically relevant setup.
Results
The 180° Stryker configuration presented itself as the system with the highest stiffness, being significantly stiffer (p < 0.001) than every system other than the poly-axial 180° aap system (p = 0.378). For the median fatigue limit the 180° Stryker and poly-axial aap systems were ranked first and second. The failure mechanism for all 90° systems was a fatigue breakage of the posterolateral plate. The 180° aap systems demonstrated breakage of the most distal screws of the lateral plate. The 180° Stryker system demonstrated screw breakage on both the medial and lateral plates.
Discussion
Breakage of the posterolateral plate as a failure mechanism for the 90° systems was expected. The 180° systems demonstrated a higher stiffness compared to the 90° constructs for the axial loading. In conclusion, both poly-axial anatomical plating systems provide sufficient stability in this scenario, and the 180° configurations demonstrated superior stiffness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Comminuted distal humeral fractures remain a challenge in trauma surgery [1]. There is insufficient evidence from randomized controlled trials that investigate which surgical interventions are the most appropriate for the surgical treatment of different types of distal humeral fractures [2]. The current gold standard for surgical treatment of intra-articular distal humeral fractures is open reduction and internal fixation with plates and/or screws [3]. In earlier studies, locked plating configurations demonstrated significantly better performance than non-locked plating configurations, independently of their orientation [4]. The fixation methods evolved into the present third generation of locking plates which include anatomical plate design and poly-axial locking screws. These features aim at rigid stability to allow early mobilization as well as adequate stiffness to stimulate fracture healing [5]. The preferred plating techniques for comminuted distal humeral fractures include the Mayo clinic configuration (180° between plates) with parallel plate fixation and medial and lateral plate positioning as well as the AO/ASIF configuration (90° angle between plates) with perpendicular plate fixation and medial and postero-lateral plate positioning [3, 6–9]. Parallel orientation of the plates seemed biomechanically superior [10], but for the translation to the clinical setting the soft tissue envelope and exposure of the distal humerus must be taken into consideration [4]. Hence, under some circumstances the 90° angle configuration might be preferable. Moreover, recent literature indicated that fixed-angle screw trajectories can make it difficult to place screws of correct length in this anatomically circumscribed region [11]. A main focus of this study is to give surgeons an idea about the biomechanical characteristics of different implant systems and configurations, especially to create an understanding of the stability of the different configurations. Subsequently, this should help the surgeon to have another parameter to include in his or her decision on which configuration to use during surgery.
In the present study the two preferred application positions (parallel and perpendicular fixation) combined with mono-axial or poly-axial screws were compared biomechanically regarding system stiffness, median fatigue limit, and failure mechanisms. We hypothesized that different fixation configurations of the different plate designs would lead to different mechanical stability of complex distal humeral fractures.
Materials and methods
The choice of load application [12, 13] as well as testing procedures [14] were based on previous studies and are briefly summarized below.
Implant types
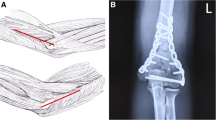
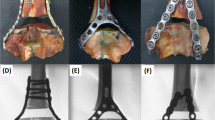
Osteosynthesis systems for the distal humerus with poly-axial locking screws (Stryker Corporation, Kalamazoo, Michigan, U.S.A.) and with mono and poly-axial locking screws (aap Implantate AG, Berlin, Germany) were tested in two different configurations (Fig. 1): a combination of medial and lateral plate (180°) and a combination of medial and posterior plate (90°). Plating systems varied in the locking mechanisms of the screws, i.e., mono-axial or poly-axial systems, resulting in six groups (Table 1).
Fracture configuration
Three senior physicians were instructed to create an AO/OTA type C2.3 fracture (intraarticular fracture site and a metaphyseal comminution area) on Large Left 4th Generation Composite Humerus (Item #3404, Sawbones Europe AB, Malmö, Sweden). The comminution zone was created by removal of a 6 mm thick bone piece in the transversal plane, starting 15 mm proximal of the distal joint axis. A second osteotomy was performed with a 0.5 mm saw from the deepest point of the trochlea humeri meeting the proximal fracture gap. Afterwards, the surgeons would attach the plates to create the correct osteosynthesis. Implants were used according to manufacturer’s instructions: For the Stryker system 2.7 mm screws were utilized and for the aap system 2.5 mm, 2.7 mm, and 3.5 mm screws were used. For the poly-axial implants surgeons were instructed to use the screws in a 0° angle. The composite humeri were cut off 190 mm from their proximal end for fixation in the clamping device.
Test setup and parameters
For each of the six tested groups, a two-piece mold was created out of polymethylmethacrylate (RENCAST FC 53, Huntsman Advanced Materials, Bad Säckingen, Germany) where only the bone was embedded, but not the plates or screws. The specimens were then clamped in a testing machine (INSTRON E3000/8874, INSTRON GmbH, Darmstadt, Germany; Fig. 2) which was equipped with a 10kN load cell, with accuracy class 0.5 (DIN EN ISO 7500-1). Specimens were loaded at the elbow joint in a 5° flexion angle which represents an extended position of the arm. Compressive loading was induced by using a compensator with an eccentric centre of rotation. By eccentric loading a force distribution of 60% on the humero-radial joint and 40% on the humero-ulnar joint could be realized [13, 15]. Stiffnesses of the specimens were assessed by using at least three specimens from each group that were loaded to 300 N three times for setting and once for stiffness determination. One specimen in each group was further loaded until failure in order to estimate the system yield strength (R p0.2 ) for the starting point of the cyclic fatigue testing. Median fatigue limit (MFL) testing was based on ASTM STP 731 [16], a technical standard for fatigue tests by the American Society for Testing and Materials, and was conducted according to our previous study [14] with a run out criterion of 250,000 cycles as an approximate number of movements during three months after surgery. Failure criteria for destructive and MFL testing was bone, plate or screw failure or a displacement more than 4 mm. MFL tests started with 50% of the previously estimated systems yield strengths (R p0.2 ), and loads were then either increased (run out) or decreased (failure) by 10% R p0.2 for the next specimen of a group.
Outcome parameters and data analyses
MFL was calculated according to ASTM STP 731 [16]. The measured stiffnesses were in every case corrected with testing machines’ stiffnesses by assuming a serial connection of springs (machine and specimen). Comparison of stiffnesses was performed in IBM SPSS Statistics 19 (IBM Corp, Armonk, NY, U.S.A.). Significance level was set to α = 0.05. For stiffness comparison of the different implant systems a three-way (manufacturer, configuration, poly-/mono-axial) analysis of variance was performed. Individual stiffnesses were compared by student’s t-tests (Bonferroni adjusted: α* = 0.05/15 = 0.003). MFLs were compared by one-way (implant system) ANOVA and post-hoc Tukey’s HSD.
Results
The absolute differences among the individual groups and their respective post hoc p-values are depicted in Fig. 3 and Table 2 for the stiffness and Fig. 4 and Table 3 for the median fatigue limit. The three-way ANOVA demonstrated that the main effect configuration had a significant effect (p < 0.001) on stiffness, with the 180° configurations demonstrating three times higher stiffness compared to the 90° configurations (Fig. 3). For the main effect of manufacturer, no differences were found for 90° configuration but for the 180° configuration the Stryker constructs were significantly stiffer (46% and 13%) compared to both aap constructs (p < 0.01). Comparing the systems’ individual stiffnesses, the 180° Stryker configuration demonstrated the highest stiffness, being significantly stiffer (p < 0.001) than any other system but the poly-axial 180° aap system (p = 0.06; Fig. 3 and Table 2). No difference was observed between mono-axial and poly-axial screw fixation regarding the construct stiffness in the aap system (p = 0.69 for 90° and p = 0.19 for 180°).
The cyclic fatigue tests revealed significant differences among the six groups for the median fatigue limits (p < 0.001). For aap, Tukey’s post hoc analysis demonstrated a higher MFL for the 180° configurations than for the 90° configurations but did not demonstrate differences between the mono- and poly-axial configurations (Fig. 4, Table 3).
Failure mechanism for all 90° systems was a fatigue breakage of the posterolateral plate. The 180° aap systems failed by breakage of the distal screws of the lateral plate, the 180° Stryker systems additionally on the medial plate. In some cases additional breakage of the composite bone was observed at the location of the screw holes.
Discussion
Double plate osteosynthesis is the standard treatment for intercondylar or supracondylar distal humeral fractures [17] demonstrating good and reliable treatment outcome [18–20]. In this biomechanical study the two most common plate configurations (parallel and perpendicular) were compared with respect to the stiffness they provide for fracture fixation and their fatigue strength under cyclic loading. Parallel plating (180°) consistently demonstrated higher fracture fixation stiffness and higher median fatigue limit compared to perpendicular plating (90°). For the implants used in this study the use of poly-axial locking screws did not affect stiffness or fatigue compared to mono-axial locking screws.
For the biomechanical tests a setup was chosen which enabled testing of the distal humerus in an extension loading mode [12]. Therefore, the mechanical performance of the plating configuration was assessed in the most relevant physiological loading condition of the elbow joint [3]. Loads were physiologically distributed on the elbow joint [12, 13].
As expected from previous studies [8, 21–23] the 180° parallel configurations demonstrated a higher stiffness than the 90° perpendicular configurations for the axial loading mode. This biomechanical advantage of parallel plating, has been confirmed by good clinical results [24]. However, this biomechanical advantage in extension loading does not necessarily transfer to flexion loading mode as the bending moments in flexion interact differently with the plate configurations [14]. As the loads in extension are expected to be higher than in flexion [25], the extension configuration might be more relevant for the analysis of fixation stiffness as well as for the failure of fixation. Loads in varus and valgus direction are not introduced during controlled elbow flexion and extension but are rather due to unintended force applications, which should be avoided during early rehabilitation after fractures around the elbow. Furthermore, loads in other directions, e.g. anterior or posterior direction need to be compensated by muscular activity mainly resulting in compressive loading of the elbow joint. Nevertheless, the findings from our biomechanical study are limited to the extent that they focus on compressive loading during extension and lack the inclusion of torsion and moments from other loading situations.
In our biomechanical testing scenario, failure for the perpendicular configuration occurred as breakage of the posterolateral plate and can be explained by high bending forces acting on the posterolateral plate which resulted in stress concentration in the plate holes [26]. Failure for the parallel configuration occurred consistently at higher load levels and through breakage of the screws or the bone material suggesting a more efficient load distribution in parallel plating. For all tested configurations the median fatigue limit for 250,000 loading cycles exceeded 340 N. Loads occurring at the elbow during activities of daily living are about 0.3 to 0.5 times body weight [25], equivalent to 220 N to 370 N for a person of 75 kg. Considering the fact that the elbow will only be loaded carefully during the first weeks of post-operative fracture care, the median fatigue limit appears to be sufficient for all plate configurations to endure the time for normal fracture healing. The values for stiffness and fatigue are in good agreement with results from previous studies on similar implant configurations [5, 14].
The design of recent locked plating systems provides the opportunity for poly-axial screw placement. While this enhances the ability to capture individual fracture fragments by placing the screws accordingly, it involves the risk of earlier screw loosening [27]. The findings from this study suggest that the poly-axial mechanism has no biomechanical disadvantages in terms of construct stiffness and fatigue failure. Previous studies even suggested that poly-axial locking mechanisms are more forgiving in terms of screw stability for deviation from correct screw inclination than fixed angle locking mechanisms [27].
As a limitation, dynamic testing was only performed in extension because this is the more challenging load application for the elbow joint [12]. However, the elbow joint also has to support a considerable amount of torsion which was not tested in the current study. Artificial bones were used instead of human bones due to our particular interest in the implant systems themselves and their mechanical performance. Thus, the test setup did not consider any soft tissue forces from tendons and ligaments which are thought to stabilize the fracture. It has to be considered that human bone, in particular osteoporotic bone may not be able to withstand the loads applied in this study and might result in failure at lower load levels due to bone failure or screw penetration. Furthermore, biological factors potentially affecting the biomechanical responses such as or individual healing response or comorbidities (e.g., smoking, obesity, or diabetes mellitus) which are associated with early loosening or breakage of implants cannot be considered in the biomechanical test setting [28]. Finally, only one singular fracture situation, the AO/OTA C2.3 fracture type was investigated representing a frequent and technically challenging type of complex intra-articular distal humeral fractures [29].
In conclusion, the tested anatomical plating systems provide sufficient mechanical stability for the fixation of complex distal humeral fractures. Consistently the parallel plate configurations demonstrated superior stiffness and fatigue performance. No differences in mechanical performance were found between poly- and mono-axial screw systems. Nevertheless, the clinical choice of the correct implant configuration needs to consider the individual fracture configuration, local soft tissue situation, and surgeon’s preferences.
References
Bégué T (2014) Articular fractures of the distal humerus. Orthop Traumatol Surg Res 100(1 Suppl):S55–S63. doi:10.1016/j.otsr.2013.11.002
Wang Y, Zhuo Q, Tang P et al (2013) Surgical interventions for treating distal humeral fractures in adults. Cochrane Database Syst Rev 1:CD009890. doi:10.1002/14651858.CD009890.pub2
Amis AA, Dowson D, Wright V (1980) Analysis of elbow forces due to high-speed forearm movements. J Biomech 13(10):825–831
Caravaggi P, Laratta JL, Yoon RS et al (2014) Internal fixation of the distal humerus: a comprehensive biomechanical study evaluating current fixation techniques. J Orthop Trauma 28(4):222–226. doi:10.1097/BOT.0b013e3182a6693f
Hungerer S, Wipf F, von Oldenburg G et al (2014) Complex distal humerus fractures-comparison of polyaxial locking and nonlocking screw configurations-a preliminary biomechanical study. J Orthop Trauma 28(3):130–136. doi:10.1097/BOT.0b013e31829d19a4
Lee J-K, Choi Y-S, Sim Y-S et al (2016) Dual plate fixation on distal third diaphyseal fracture of the humerus. Int Orthop. doi:10.1007/s00264-016-3355-4
Li SH, Li ZH, Cai ZD et al (2011) Bilateral plate fixation for type C distal humerus fractures: experience at a single institution. Int Orthop 35(3):433–438. doi:10.1007/s00264-010-1011-y
Bogataj M, Kosel F, Norris R et al (2015) Biomechanical study of different plate configurations for distal humerus osteosynthesis. Med Biol Eng Comput 53(5):381–392. doi:10.1007/s11517-015-1247-1
Atalar AC, Tunali O, Ersen A et al (2016) Biomechanical comparison of orthogonal versus parallel double plating systems in intraarticular distal humerus fractures. Acta Orthop Traumatol Turc. doi:10.1016/j.aott.2016.11.001
Taylor PA, Owen JR, Benfield CP et al (2016) Parallel plating of simulated distal humerus fractures demonstrates increased stiffness relative to orthogonal plating with a distal humerus locking plate system. J Orthop Trauma 30(4):e118–e122. doi:10.1097/BOT.0000000000000477
Jayakumar P, Ring D (2015) A pitfall in fixation of distal humeral fractures with pre-contoured locking compression plate. Arch Bone Jt Surg 3(2):130–133
Schuster I, Korner J, Arzdorf M et al (2008) Mechanical comparison in cadaver specimens of three different 90-degree double-plate osteosyntheses for simulated C2-type distal humerus fractures with varying bone densities. J Orthop Trauma 22(2):113–120. doi:10.1097/BOT.0b013e3181632cf8
Halls AA, Travill A (1964) Transmission of pressures across the elbow joint. Anat Rec 150:243–247
Penzkofer R, Hungerer S, Wipf F et al (2010) Anatomical plate configuration affects mechanical performance in distal humerus fractures. Clin Biomech (Bristol, Avon) 25(10):972–978. doi:10.1016/j.clinbiomech.2010.07.005
Morrey BF, Sanchez-Sotelo J (eds) (2009) The elbow and its disorders, 4th edn. Elsevier, Philadelphia
Little RE (1981) Tables for estimating median fatigue limits. ASTM special technical publication, vol 731. ASTM, Philadelphia
Zalavras CG, McAllister ET, Singh A et al (2007) Operative treatment of intra-articular distal humerus fractures. Am J Orthop (Belle Mead NJ) 36(12 Suppl 2):8–12
Kumar S, Singh S, Kumar D et al (2015) Intercondylar humerus fracture- parallel plating and its results. J Clin Diagn Res 9(1):RC01–RC04. doi:10.7860/JCDR/2014/12137.5479
Lee SK, Kim KJ, Park KH et al (2014) A comparison between orthogonal and parallel plating methods for distal humerus fractures: a prospective randomized trial. Eur J Orthop Surg Traumatol 24(7):1123–1131. doi:10.1007/s00590-013-1286-y
Tian D, Jing J, Qian J et al (2013) Comparison of two different double-plate fixation methods with olecranon osteotomy for intercondylar fractures of the distal humeri of young adults. Exp Ther Med 6(1):147–151. doi:10.3892/etm.2013.1102
Arnander MW, Reeves A, MacLeod IA et al (2008) A biomechanical comparison of plate configuration in distal humerus fractures. J Orthop Trauma 22(5):332–336. doi:10.1097/BOT.0b013e31816edbce
Kollias CM, Darcy SP, Reed JGR et al (2010) Distal humerus internal fixation: a biomechanical comparison of 90 degrees and parallel constructs. Am J Orthop (Belle Mead NJ) 39(9):440–444
Zalavras CG, Vercillo MT, Jun B-J et al (2011) Biomechanical evaluation of parallel versus orthogonal plate fixation of intra-articular distal humerus fractures. J Shoulder Elbow Surg 20(1):12–20. doi:10.1016/j.jse.2010.08.005
Celli A, Donini MT, Minervini C (2008) The use of pre-contoured plates in the treatment of C2-C3 fractures of the distal humerus: clinical experience. Chir Organi Mov 91(2):57–64. doi:10.1007/s12306-007-0022-3
An KN, Kwak BM, Chao EY et al (1984) Determination of muscle and joint forces: a new technique to solve the indeterminate problem. J Biomech Eng 106(4):364–367
Kudo T, Hara A, Iwase H et al (2016) Biomechanical properties of orthogonal plate configuration versus parallel plate configuration using the same locking plate system for intra-articular distal humeral fractures under radial or ulnar column axial load. Injury 47(10):2071–2076. doi:10.1016/j.injury.2016.08.012
Lenz M, Wahl D, Gueorguiev B et al (2015) Concept of variable angle locking--evolution and mechanical evaluation of a recent technology. J Orthop Res 33(7):988–992. doi:10.1002/jor.22851
Claessen FMAP, Braun Y, Peters RM et al (2015) Plate and screw fixation of bicolumnar distal humerus fractures: factors associated with loosening or breakage of implants or nonunion. J Hand Surg [Am] 40(10):2045–2051.e2. doi:10.1016/j.jhsa.2015.07.009
McCarty LP, Ring D, Jupiter JB (2005) Management of distal humerus fractures. Am J Orthop (Belle Mead NJ) 34(9):430–438
Acknowledgements
Open access funding provided by Paracelsus Medical University. Patrick A. Varady and Christian von Rüden contributed equally to this work.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Stryker and aap provided financial support to the authors’ institution for the biomechanical testing of the implants.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Varady, P.A., von Rüden, C., Greinwald, M. et al. Biomechanical comparison of anatomical plating systems for comminuted distal humeral fractures. International Orthopaedics (SICOT) 41, 1709–1714 (2017). https://doi.org/10.1007/s00264-017-3444-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3444-z