Abstract
Purpose
Reduction and fixation of proximal humerus fracture (PHF) by intra-focal distraction with a cemented device is seldom used. A cementless stem called JUST was developed to simplify and standardise reduction and fixation of three- or four-part fractures (3-/4-PFs). This study is designed to evaluate the performances of this device. In addition, we compared the results to those of a previous study based on cemented stems.
Method
Twenty-five patients underwent surgery between 2009 and 2011: ten 3-PFs and 15 4-PFs, with a median age of 65.5 and 71 years, respectively. The reduction and fixation device comprises a staple placed in the humeral head and a cementless stem impacted in the diaphysis that works like a jack. Median follow-up was 28 months.
Results
For the ten 3-PFs, the median raw and weighted Constant score were 66.5 and 86, respectively. Only one case presented with secondary displacement. All fractures healed and there was only one case of avascular necrosis. For the 15 4-PFs, the median raw and weighted Constant score were 64 and 76, respectively. Only one case of secondary cephalic displacement was observed and no cases of tuberosity displacement were observed. All fractures healed except for one case of pseudarthrosis of the lesser tuberosity. Five cases of avascular necrosis were observed.
Conclusions
This device resolves the mechanical difficulties relating to fixation of 3- and 4-PFs by providing stable fixation but does not prevent the risk of avascular necrosis. The cementless stem is more convenient but does not yield better results than the cemented stem.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open reduction and internal fixation (ORIF) of three- or four-part fractures (3-/4-PFs) of the proximal humerus remains problematic [1–3]. One of the many methods proposed to resolve this mechanical challenge is the Bilboquet implant [4–6], which reduces displacement of the humeral head by intrafocal distraction without using screws. Despite the good results reported, this surgical technique is seldom used, probably due to the fact that cement is required to fix the stem. Hence, a cementless stem was developed to adjust the height of the humeral head gradually and in a reversible manner. This observational study reports the results of 25 3-/4-PFs of the proximal humerus treated with a Bilboquet-like device with cementless stem (Fig. 1) called JUST (Jack Up for Shoulder Trauma; Evolutis, Briennon, France). The aims of this study were to evaluate the performances of the cementless stem compared with the cemented stem, and to confirm the previous results.
Materials and methods
Between January 2009 and December 2011, 73 patients were treated in our institution for proximal humerus fracture by ORIF. Twenty-seven patients had ORIF with the JUST implant for 3-/4-PF according to the Neer classification [7, 8]. Two patients were lost to follow-up. This study includes 25 fractures in 25 patients. There were ten 3-PFs and 15 4-PFs. Sixteen patients (64 %) were retired at the time of injury. There were 17 right-sided and eight left-sided fractures. The dominant side was affected in 84 % of cases (15 times on the right and 6 times on the left).
All patients had standard AP and lateral X-rays and in 20 cases a pre-operative computed tomography (CT) scan was performed. The type of head displacement and the presence of a metaphyseal head extension (also called calcar segment) were noted [9].
The ten 3-PFs concerned five women and five men with a median age of 65.5 years (range, 44–88). The X-rays showed varus displacement of the humeral head in six cases and valgus displacement in four cases. In all cases, there was no hinge and in seven cases the calcar segment measured >8 mm.
The 15 4-PFs concerned nine women and six men with a median age of 71 years (51–84). The X-rays showed six varus displacements and nine valgus displacements. There was an internal hinge in three cases. The calcar measured >8 mm in seven cases. It measured <8 mm in three cases, was comminuted in three cases and absent in two cases.
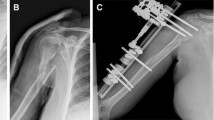
Four different surgeons performed all the surgery. The patients were operated on through a lateral deltoid split approach in the beach-chair position under fluoroscopic control. The first part of the procedure is identical in terms of technique and material to the description of the Bilboquet device [4] (Fig. 2): careful penetration into the fracture; elevation of the humeral head in the cases of valgus displacement; under fluoroscopic guidance, placement of the titanium cephalic staple in the cancellous bone of the humeral head; drilling of two holes in the external cortical bone of the diaphysis to pass two Ethibond 6 sutures ready for final suture of the greater tuberosity. The second part of the procedure is differs from that described for the Bilboquet technique as cement is not used (Fig. 3). It consists of placing a height-adjustable cementless stem in the diaphysis. A trial stem placed in the diaphysis is used to choose the proper size and the final stem is then inserted into the diaphysis. The titanium cementless stem is made of three components: a sort of trapezoid section (wedge), a stem and a locking screw. The trapezoid section is designed to be settled into the diaphysis. This section is crossed by a stem fitted with a Morse taper tilted at 130° on the vertical axis. The stem and the trapezoid section are locked together by a locking screw. When the locking screw is removed the stem slides into the section. The cementless stem is set in the diaphysis using a stem-holder. Then, by mobilising the arm, the stem Morse taper is introduced into the staple. The stem-holder is removed and a distraction forceps, in the manner of a jack, pushes the stem up and elevate the humeral head by 6-mm notches under visual and fluoroscopic control. The maximal possible distraction is 18 mm (three notches). When, under the effect of the distraction, the anatomical metaphyseal curve is restored, and the wedge and the stem are locked together by the locking screw. At this stage, fixation between the humeral head and the diaphysis is performed.
a Drawing of a four-part fracture displaced in valgus. b The fracture is exposed using a deltoid splitting approach. c The humeral head is carefully elevated using a rasp. d The titanium staple is impacted in the cancellous bone of the humeral head. e Two holes are drilled through the humeral shaft to pass tension band wires
a A trial stem is placed inside the humeral shaft. b Using the stem-holder, the cementless stem is placed into the shaft. c The Morse taper of the stem is engaged into the female taper of the staple. d The stem-holder is retrieved and the distraction forceps elevate the stem and the humeral head. e Tuberosities are reduced and tied with horizontal and vertical sutures
The rest of the operation consists of suturing the tuberosities using the two sutures passed through the diaphysis. In 4-PFs, additional horizontal anterior-posterior laces are needed.
Post-operatively, the arm was immobilised in a sling and physiotherapy was started between the fourth and the seventh days by passive mobilisation, and active motion started after one month.
The patients were seen again regularly for clinical and radiological follow-up.
For the 3-PFs, the median follow-up was 28 months (range, 22–36).
For the 4-PFs, the median follow-up was 24 months (range, 22–31).
The clinical parameters evaluated at final follow-up were: active range of motion, raw and weighted Constant score (CS) [10] and overall patient satisfaction.
Radiological assessment was based on the AP and lateral X-rays. To confirm suspected post-operative displacement of the humeral head or of the tuberosities, two radiological criteria were used: 30° or more change in angle of a bone fragment or more than 10 % displacement in the diameter of the humeral head on X-ray (i.e. 5 mm for 50 mm diameter on the X-ray). Avascular necrosis of the humeral head was evaluated according to the Cruess classification [11].
Finally, we used the results of a series of cemented stems previously published [4] to compare the results of the present series to this previous one. Briefly, the previous series involved 22 patients, with a mean age of 70 years, with 3-PFs and 4-PFs in seven and 15 cases, respectively, followed-up for 34 months. The results of the present study were compared with those of the study published on the cemented device using the Wilcoxon-Mann–Whitney test for the quantitative variables and Fisher’s exact test for the qualitative variables.
Results
Results for the ten 3-PFs are shown in Table 1.
The median raw CS was 66.5 points (range, 52–82) and the median weighted CS 86 % (62–100 %). Active anterior elevation median was 125° (85–160°) and that of active external rotation was 30° (0–45°).
Radiologically, only one post-operative reduction was not satisfactory (head in varus) and during follow-up only one case presented with secondary displacement (cephalic varus) clinically associated with complex regional pain syndrome (case 5).
All fractures (head and tuberosities) healed and at final follow-up, there was one case of stage 3 avascular necrosis with no functional repercussions, and only case 5 was not satisfied with the functional result.
Results for the 15 4-PFs are shown in Table 2.
The median raw CS was 64 points (30–81) and the median weighted CS 76 % (40–100 %). Active anterior elevation median was 110° (85–160°) and that of active external rotation was 30° (0–45°). There was one case of complex regional pain syndrome (case 14).
Radiologically, post-operative head reduction was not satisfactory in two cases (one high head and one in varus) and that of the tuberosities in three cases (one greater tuberosity and two lesser tuberosities). During follow-up, only one case of secondary cephalic displacement was observed (varus) and no cases of secondary tuberosity displacement were observed. All fractures healed except in one case of pseudarthrosis of the lesser tuberosity. At final follow-up there were five cases of avascular necrosis: one stage 2, three stage 4 and one stage 5.
At final follow-up, five patients were not satisfied with the functional result.
Comparison of the 3-PFs in this study with those in the study published on the cemented device indicate that follow-up was significantly shorter (p = 0.04) in the study on the cementless device, with a median difference [95 % confidence interval] of −6 m [−12; −4 × 10−5]. Male/female distribution (5/5 and 2/5 in the study with the cementless device and in that with the cemented device respectively) was not significantly different (p = 0.63), and the same applied for age (median difference of −3 years [−22; 12], p = 0.56). As for the results of surgery, the median difference [95 % confidence interval] in the raw CS (−1.3 % [−14 %; 10 %]) or weighted score (0 % [−18 %; 15 %]) was not significant (p = 0.81 and p = 0.85, respectively), and the same applied for the proportion of patients with necrosis (1/10 versus 0/7, p = 1).
The results are relatively similar for the comparisons of the 4-PFs: follow-up was also significantly shorter in the study on the cementless device (−6 m [−14; −2], p = 0.005). Male/female distribution (6/9 and 2/13 in the study with the cementless device and in that with the cemented device respectively) was not significantly different (p = 0.22), and the same applied for age (median difference of −1 year [−11; 7], p = 0.73). As for the results of surgery, the median difference [95 % confidence interval] in the raw CS (−5 % [−20 %; 8 %]) or weighted score (−4 % [−24 %; 5 %]) was not significant (p = 0.47 and p = 0.28, respectively), and the proportion of patients with necrosis was strictly identical (5/15 both for the cementless device and the cemented device).
Discussion
The Bilboquet device was developed to solve the mechanical problems of osteosynthesis in 3-/4-PFs, in particular in elderly patients [4–6]. Using the Bilboquet cemented stem, the surgeon performed manual distraction on a single-sized stem and placed cement in the openings between the diaphysis and the stem to hold it. Distraction could, therefore, not be finely adjusted or reversed. With the JUST cementless stem, the surgeon chooses the most suitable stem size, then performs gradual distraction until anatomical reduction is achieved, under fluoroscopic guidance. Reduction and fixation, reputedly difficult in this type of fracture, therefore resembles elective surgery.
The study has some limitations. This is a retrospective study involving four different surgeons on a small number of cases (n = 25). Therefore, the generalisability of the favourable results of this series should be confirmed by further studies. In addition, the comparison with the previous study based on non-cemented stems has a low statistical power.
The use of proximal nailing with locking screws is a widely used technique, in particular in two-part fractures (2-PFs) due to its minimally invasive approach [12, 13], although publications report numerous mechanical complications, especially in 3- and 4-PFs. Mittelmeier et al. [14] report a complication rate of 51 % with the Targon nail, including 22.6 % screw migrations. Cuny et al. [15] reported ten cases of revision surgery (15 %) for mechanical problems with the Telegraph nail and six cases of secondary tuberosity displacement. Sosef et al. [16] in a series of 33 patients treated by Polaris nail, most of them for 2-PF, report 18 % revisions for mechanical problems; whereas Nolan et al. [17], in a series of 18 patients with 2- and 3-PFs, with an average age of 71 years treated with Polaris nail, reported seven cases necessitating revision surgery (39 %) for mechanical problems.
For locking screw plates, Kettler et al. [18] reported the results of 176 patients treated by Philos plate. Complications included 11 % intra-articular screws, 8 % secondary tilting and 4.5 % hardware fractures. Average age was 66 years and 35 % of cases were 2-PFs.
Sudkamp et al. [19] reported that 187 patients treated by locking plate had an absolute CS of 71 after one year and a relative score of 85 %. The average age of their patients was only 63 years and most fractures were Muller-AO type A or B1. However, the authors reported 34 % of complications and 19 % of surgical revisions. Thanasa et al. [20], in a meta-analysis of 12 publications on locking plates, reported a mean CS of 74 points in a population with a mean age of 63 years. Although there were 27.8 % of 2-PFs, there were 11.6 % of secondary displacements. Sproul et al. [21] in a large review of 514 cases, reported an overall complication rate of 48.8 %, of which 13.8 % were revisions. Konrad et al. [22] in a multicentre study of 318 patients reported 29 % with intra-operative and post-operative complications, mostly screw perforations. Finally, Clement [23] wondered what are the exact indications for the Philos plate and, on behalf of 27 published studies, stated that its use would be of no significant evidence for the elderly patients.
All publications on locking plates insist on the difficulty of achieving stable fixation in the event of osteoporosis. Several authors [24–28] highlight the importance of adding medial head support to internal fixation, either with screws or internal plates, and cement or bone graft to prevent disassembly.
In our experience of 3-/4-PFs in the elderly, metaphyseal comminution does not provide support for the humeral head after anatomical reduction and, therefore to achieve stability with screws, the bone defect has to be filled-up for with some sort of support (bone, bone substitute, cement, metal). The staple in our intra-focal distraction system is an ‘equatorial’ support platform for the humeral head, from which the diaphyseal stem can provide ascending force for reduction with little risk of going through the head or causing a varus tilt, on the condition that an external tension band wire is also used.
We observed only two cases of minor displacement of the initial assembly in this series.
In the series of 22 cases with cemented stems to which we are comparing our results [4], there was no secondary displacement.
Anatomical reduction of the humeral head on the diaphysis facilitates anatomical reduction of the tuberosities, which naturally fall into place during tension band wiring. Given the natural bone environment, union of the tuberosities is achieved almost every time (Fig. 4). Union of the tuberosities is one of the characteristics of this method. In the present series there is only one case of lesser tuberosity pseudarthrosis. In terms of functional recovery, the tests carried out do not show a significant difference between the two series on the weighted CS, as much for the 3-PFs (p = 0.85) as for the 4-PFs (p = 0.28). The functional and radiological results are comparable regardless of whether the stem is fixed with or without cement. However, use of the cement to set the stem at the right height was probably an obstacle to widespread use of this method. Modulable and reversible distraction of the JUST cementless stem is easier, more didactic and makes learning easier.
With median anterior elevation of 125° and weighted CS of 86 % for 3-PFs and median anterior elevation of 110° and median weighted CS of 76 % for 4-PFs, our intra-focal distraction technique compares favourably with the publications on reduction and fixation mentioned previously [3, 19].
However, even if intrafocal distraction reduction and fixation provides a solution to the mechanical problem of 3-/4-PFs, it does not resolve the biological problem, that of humeral head avascular necrosis. In this series, we had one case of stage 3 necrosis among the 3-PFs and as in the cemented stem series, we saw five cases of necrosis (33 %) among 4-PFs cases. The low prevalence of avascular necrosis among the 3-PFs is the rule in our series. Our overall percentage of avascular necrosis remains within the range of that observed: 35 % for Gerber et al. [25] and 37 % in the meta-analysis by Lanting et al. [1].
Among the five 4-PF-related cases of avascular necrosis, that of stage 2 (case 9) occurring in a 59-year-old patient with excellent functional results needs to be set aside, as it was discovered on the X-rays. The four other cases of necrosis are three stage 4 and one stage 5, for which the functional results deteriorated after the 1st year, with radiologically obvious diagnosis from the 15th month. In the four cases, the predictors of poor prognosis factor according to Hertel et al. [9] are observed: no internal hinge, calcar segment absent or fragmented in three cases out of four. Out of the four cases of necrosis, two required hemiarthroplasty revision (13 %), which raised the question of the initial indication for hemiarthroplasty in the 3-/4-PFs.
However, despite the improvements in humeral head prosthesis and special care taken when repairing tuberosities, the hemiarthroplasty result in traumatology does yield better results than reduction and fixation [1, 3, 9, 29]. The use of implants specifically designed for traumatology does not appear to significantly improve the results [30].
Malposition or secondary displacement of the tuberosities is the main complication of hemiarthroplasty in traumatology [2, 31]. Plausinis et al. [32] reports that peri-operative complications are the main factor affecting the clinical result. Therefore, component misalignment can reach 40 %, tuberosity detachment or misalignment 23 % and 27 %, and tuberosity resorption varies from 0 to 7 %.
Due to the difficulties of achieving union of the tuberosities in hemiarthroplasties, use from the outset of a reverse prosthesis has been proposed in the treatment of 3- and 4-PFs [33, 34] and would appear to be increasingly popular [35, 36].
However, use of a reverse prosthesis for 3-/4-PFs is for us a therapeutic leap of faith with major uncertainty as to the long-term outcome of the implants [37, 38]. In reduction and fixation such as we suggest, the implant is no longer under strain after consolidation of the fracture and all complications inherent to any prostheses are avoided. Quasi-systematic union of the tuberosities in our study effectively shows that in a stable and low-metal environment, the outcome is regularly favourable. Nevertheless, where the humeral head has lost all attachment from the soft tissues, as is the case with 4-PFs with the line flush with the head, the risk of avascular necrosis is high and the choice of hemiarthroplasty from the outset would appear to be justified.
Conclusions
ORIF of 3-/4-PFs of the proximal humerus by intra-focal distraction using the JUST implant makes it possible to improve the mechanical difficulties relating to repairing these fractures, by producing stable fixation of the head and reliable healing of the tuberosities. However, this method does not prevent the risk of avascular necrosis of the humeral head. The cementless stem is more convenient but does not produce better results than the cemented stem.
References
Lanting B, MacDermid J, Drosdowech D, Faber KJ (2008) Proximal humeral fractures: a systematic review of treatment modalities. J Shoulder Elb Surg 17:42–54. doi:10.1016/j.jse.2007.03.016
Maier D, Jaeger M, Izadpanah K, Strohm PC, Suedkamp NP (2014) Proximal humeral fracture treatment in adults. J Bone Joint Surg Am 96:251–261. doi:10.2106/JBJS.L.01293
Solberg BD, Moon CN, Franco DP, Paiement GD (2009) Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am 91:1689–1697. doi:10.2106/JBJS.H.00133
Doursounian L, Kilinc A, Cherrier B, Nourissat G (2011) Complex proximal humeral fractures: a prospective study of 22 cases treated using the “Bilboquet” device. Orthop Traumatol Surg Res 97:58–66. doi:10.1016/j.otsr.2010.06.015
Doursounian L, Grimberg J, Cazeau C, Jos E, Touzard RC (2000) A new internal fixation technique for fractures of the proximal humerus—the Bilboquet device: a report on 26 cases. J Shoulder Elb Surg 9:279–288
Doursounian L, Grimberg J, Cazeau C, Touzard RC (1996) A new method of osteosynthesis in proximal humeral fractures: a new internal fixation device. Apropos of 17 cases followed over more than 2 years. Rev Chir Orthop Reparatrice Appar Mot 82:743–752
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Neer CS 2nd (2002) Four-segment classification of proximal humeral fractures: purpose and reliable use. J Shoulder Elb Surg 11:389–400
Hertel R, Hempfing A, Stiehler M, Leunig M (2004) Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elb Surg 13:427–433
Constant CR (1997) An evaluation of the Constant-Murley shoulder assessment. J Bone Joint Surg (Br) 79:695–696
Cruess RL (1986) Osteonecrosis of bone. Current concepts as to etiology and pathogenesis. Clin Orthop Relat Res 208:30–39
Lin J, Hou SM, Hang YS (1998) Locked nailing for displaced surgical neck fractures of the humerus. J Trauma 45:1051–1057
Zhu Y, Lu Y, Shen J, Zhang J, Jiang C (2011) Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Joint Surg Am 93:159–168. doi:10.2106/JBJS.J.00155
Mittlmeier TW, Stedtfeld HW, Ewert A, Beck M, Frosch B, Gradl G (2003) Stabilization of proximal humeral fractures with an angular and sliding stable antegrade locking nail (Targon PH). J Bone Joint Surg Am 85-A(Suppl 4):136–146
Cuny C, Scarlat MM, Irrazi M, Beau P, Wenger V, Ionescu N, Berrichi A (2008) The Telegraph nail for proximal humeral fractures: a prospective four-year study. J Shoulder Elb Surg 17:539–545. doi:10.1016/j.jse.2008.02.004
Sosef N, van Leerdam R, Ott P, Meylaerts S, Rhemrev S (2010) Minimal invasive fixation of proximal humeral fractures with an intramedullary nail: good results in elderly patients. Arch Orthop Trauma Surg 130:605–611. doi:10.1007/s00402-009-1027-1
Nolan BM, Kippe MA, Wiater JM, Nowinski GP (2011) Surgical treatment of displaced proximal humerus fractures with a short intramedullary nail. J Shoulder Elb Surg 20:1241–1247. doi:10.1016/j.jse.2010.12.010
Kettler M, Biberthaler P, Braunstein V, Zeiler C, Kroetz M, Mutschler W (2006) Treatment of proximal humeral fractures with the PHILOS angular stable plate. Presentation of 225 cases of dislocated fractures. Unfallchirurg 109:1032–1040
Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, Luo C, Plecko M, Wendt K, Köstler W, Konrad G (2009) Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am 91:1320–1328. doi:10.2106/JBJS.H.00006
Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P (2009) Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elb Surg 18:837–844. doi:10.1016/j.jse.2009.06.004
Sproul RC, Iyengar JJ, Devcic Z, Feeley BT (2011) A systematic review of locking plate fixation of proximal humerus fractures. Injury 42:408–413. doi:10.1016/j.injury.2010.11.058
Konrad G, Hirschmüller A, Audige L, Lambert S, Hertel R, Südkamp NP (2012) Comparison of two different locking plates for two-, three- and four-part proximal humeral fractures—results of an international multicentre study. Int Orthop 36:1051–1058. doi:10.1007/s00264-011-1410-8
Clement ND (2013) Can we decipher indications and outcomes of the PHILOS plate for fractures of the proximal humerus? Int Orthop 37:1199–1200. doi:10.1007/s00264-013-1863-z
Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG (2007) The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma 21:185–191
Gerber C, Werner CM, Vienne P (2004) Internal fixation of complex fractures of the proximal humerus. J Bone Joint Surg (Br) 86:848–855
Kim SH, Lee YH, Chung SW, Shin SH, Jang WY, Gong HS, Baek GH (2012) Outcomes for four-part proximal humerus fractures treated with a locking compression plate and an autologous iliac bone impaction graft. Injury 43:1724–1731. doi:10.1016/j.injury.2012.06.029
Lee CW, Shin SJ (2009) Prognostic factors for unstable proximal humeral fractures treated with locking-plate fixation. J Shoulder Elb Surg 18:83–88. doi:10.1016/j.jse.2008.06.014
Zhang L, Zheng J, Wang W, Lin G, Huang Y, Zheng J, Edem Prince GA, Yang G (2011) The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop 35:1655–1661. doi:10.1007/s00264-011-1227-5
Bastian JD, Hertel R (2009) Osteosynthesis and hemiarthroplasty of fractures of the proximal humerus: outcomes in a consecutive case series. J Shoulder Elb Surg 18:216–219. doi:10.1016/j.jse.2008.09.015
Loew M, Heitkemper S, Parsch D, Schneider S, Rickert M (2006) Influence of the design of the prosthesis on the outcome after hemiarthroplasty of the shoulder in displaced fractures of the head of the humerus. J Bone Joint Surg (Br) 88:345–350
Compito CA, Self EB, Bigliani LU (1994) Arthroplasty and acute shoulder trauma. Reasons for success and failure. Clin Orthop Relat Res 307:27–36
Plausinis D, Kwon YW, Zuckerman JD (2005) Complications of humeral head replacement for proximal humeral fractures. Instr Course Lect 54:371–380
Bufquin T, Hersan A, Hubert L, Massin P (2007) Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg (Br) 89:516–520
Cazeneuve JF, Cristofari DJ (2006) Grammont reversed prosthesis for acute complex fracture of the proximal humerus in an elderly population with 5 to 12 years follow-up. Rev Chir Orthop Reparatrice Appar Mot 92:543–548
Klein M, Juschka M, Hinkenjann B, Scherger B, Ostermann PA (2008) Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma 22:698–704. doi:10.1097/BOT.0b013e31818afe40
Sebastiá-Forcada E, Cebrián-Gómez R, Lizaur-Utrilla A, Gil-Guillén V (2014) Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elb Surg 23:1419–1426. doi:10.1016/j.jse.2014.06.035
Cazeneuve JF, Cristofari DJ (2011) Long term outcome following reverse shoulder arthroplasty in the elderly. Orthop Traumatol Surg Res 97:583–589. doi:10.1016/j.otsr.2011.03.025
Scarlat MM (2013) Complications with reverse total shoulder arthroplasty and recent evolutions. Int Orthop 37:843–851. doi:10.1007/s00264-013-1832-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Doursounian, L., Le Sant, A., Mauprivez, R. et al. Open reduction and internal fixation of three- and four-part proximal humeral fractures by intra-focal distraction: observational study of twenty five cases. International Orthopaedics (SICOT) 40, 2373–2382 (2016). https://doi.org/10.1007/s00264-015-3109-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3109-8