Abstract
Rotation of the femoral component in total knee arthroplasty (TKA) is of high importance in respect of the balancing of the knee and the patellofemoral joint. Though it is shown that computer assisted surgery (CAOS) improves the anteroposterior (AP) alignment in TKA, it is still unknown whether navigation helps in finding the accurate rotation or even improving rotation. Therefore the aim of our study was to evaluate the postoperative femoral component rotation on computed tomography (CT) with the intraoperative data of the navigation system. In 20 navigated TKAs the difference between the intraoperative stored rotation data of the femoral component and the postoperative rotation on CT was measured using the condylar twist angle (CTA). This is the angle between the epicondylar axis and the posterior condylar axis. Statistical analysis consisted of the intraclass correlation coefficient (ICC) and Bland-Altman plot. The mean intraoperative rotation CTA based on CAOS was 3.5° (range 2.4–8.6°). The postoperative CT scan showed a mean CTA of 4.0° (1.7–7.2). The ICC between the two observers was 0.81, and within observers this was 0.84 and 0.82, respectively. However, the ICC of the CAOS CTA versus the postoperative CT CTA was only 0.38. Though CAOS is being used for optimising the position of a TKA, this study shows that the (virtual) individual rotational position of the femoral component using a CAOS system is significantly different from the position on a postoperative CT scan.
Similar content being viewed by others
Introduction
Total knee arthroplasty (TKA) malalignment is related to an unsatisfactory outcome, including patella maltracking, anterior knee pain, flexion instability and early loosening [24]. Furthermore, inadequate positioning particularly of the femoral component is a common indication for revision [2, 8]. Using the conventional and bony reference point methods, rotation of the femoral component can be determined intraoperatively by the use of the transepicondylar line, the posterior condylar line and/or the Whiteside line [5, 23].
With the need for more accurate alignment as an important outcome determinant in TKA, prosthesis positioning has been facilitated in recent years by computer assisted orthopaedic surgery (CAOS).
The (intraoperative) value of CAOS on coronal plane alignment of knee prostheses has been discussed in literature [27]. Some showed improved alignment using CAOS [12, 21, 22, 26], while others showed little difference in alignment [3, 31] and no significantly better results during follow-up [16]. The reason for the differences are both surgical and related to the intraoperative navigation using predetermined anatomical landmarks; furthermore, the CAOS software program may be relevant. In CAOS, the planned rotational position of the components can be determined using the transepicondylar, the posterior condylar and the Whiteside line.
Although the CAOS systems have been developed in an attempt to align implants more accurately and more consistently, it is unknown if navigation systems improve the accuracy of femoral rotational alignment as compared to the traditional techniques using mechanical guiding devices [10, 11, 28]. Whether the intraoperative positions of the knee prosthesis components, as shown on the CAOS screen, reflect the actual position of the knee prosthesis has not been evaluated.
The goal of this study was to determine the validity of the intraoperative CAOS position of knee prostheses compared to the postoperative rotational position of the knee prosthesis using a postoperative CT scan evaluation method [7, 15].
Materials and methods
Twenty imageless navigated total knee arthroplasties were performed at the department of orthopaedic surgery at the Leiden University Medical Centre. In a former study by Van Strien et al. [31], the CAOS system was evaluated using postoperative radiographs and CT scans as well as RSA. The protocol was approved by the institutional medical ethics committee. All patients gave informed consent.
The average age was 69 years (SD 9 years). The group consisted of eight male and 12 female patients. Fourteen of these 20 patients had primary osteoarthritis of the knee. Five patients had secondary osteoarthritis due to rheumatoid arthritis and one secondary to haemophilia. In 11 patients the left knee was operated upon, in nine the right knee. In all patients a NexGen LPS flex prosthesis (Zimmer Inc., Warsaw) was implanted.
The Vector Vision CT free computer navigation system, software version 1.6 (BrainLAB, Feldkirchen, Germany) was used in all operations. Before identification of the bone and rotational centres of the leg and knee, the surgeon chooses in the software which reference axis will be used for determining the correct rotational position of the femoral component. These reference axes in the BrainLAB system are the epicondylar line, the posterior condylar line or the Whitesides line [32].
During surgery, anatomical landmarks are used to build a virtual image of the tibia and femur in the Brainlab system. After attaching reference markers to the tibia and femur, hip rotations are made to determine centre of rotation of the hip. The intraoperative femoral anatomical registration points are: the most prominent points of the medial and lateral epicondyles, the anterior sulcus (Whitesides line), the femoral mechanical axis, a cloud of points of the anterior distal femur and a cloud of points of the posterior condyles.
After localisation of the landmarks is completed, the software calculates the ideal position of the femoral and tibial component based on the anatomical data input of axes and surfaces (i.e. femur and tibia). With respect to the rotation reference axes, the system uses one of the preoperative selected axes (in this study the epicondylar axis); it does not take into account all three axes. However, the CAOS software displays the displacement of the component with respect to all three axes on the screen (Fig. 1). Thus data is available for off-line analysis.
The definite femoral component was positioned as proposed by the navigation system, being the optimal CAOS femoral position. In these 20 cases we did not adjust the rotation as suggested by the navigation system. The anterior cut was verified with a plane-verifying marker tree after the bone cut so that there was no change in rotation caused by the saw blade. This plane was then stored in the Brainlab system (Fig. 2). Thus the postoperative measured bone cut along the femoral component is the same as made intraoperatively.
The postoperative multi-slice CT scan was made between six weeks and three months after the operation, according to a standard protocol. Based on availability, either a 16-slice (nine patients) or 64-slice (11 patients) machine was used (Aquilion, Toshiba, Otawara, Japan). CT protocols were developed based on recommendations by the BrainLAB company. For 16-slice CT, scanning parameters were beam collimation 16 x 1 mm and pitch 0.938; images were reconstructed using a medium-smooth kernel with 1-mm slice thickness and 1-mm reconstruction index. For 64-slice CT, scanning parameters were beam collimation 64 × 0.5 mm and pitch 0.828; images were reconstructed using a standard kernel with 1-mm slice thickness and 1-mm reconstruction index. Postoperative CT images were interactively viewed on a workstation (Vitrea2, Vital Images, Minnetonka, MN, USA) using an extended window scale (16-bit deep, up to a window width and level of 65,500). Therefore, no dedicated metal artefact reduction filtering techniques were needed.
Thin-slice (1-2 mm) images of the distal femur were used to measure the postoperative rotational axes.
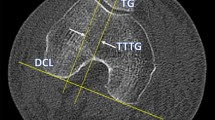
The senior author (RN) performed all the operations and was not involved in the postoperative measurements of component position. We used the condylar twist angle (CTA) to measure the rotational position of the femoral component. This is the angle between the epicondylar axis and the posterior condylar axis. This epicondylar line was drawn between the most prominent point of the medial epicondyle and the most prominent point of the lateral condyle of the distal femur. The most prominent point of the medial epicondyle which is required for the CTA is easier to identify than the medial sulcus which is required for the posterior condylar angle. Both are registered at the same time during the navigation registration process. The posterior condylar line was drawn along the posterior femoral cut (i.e. the inner border of the metal posterior condyles of the femoral component). At the CT scan viewer (Sectra workstation) two points were identified at the medial and lateral epicondyles for angle measurement (CTA). These points were marked at the CT workstation and were thus visible at the different CT slices (Fig. 3). Therefore, the angle between the medial and lateral epicondyle could be measured accurately without reconstructing a thick slice to visualise both most prominent epicondylar points at the same time.
The CTA was independently measured by two observers, at two separate time intervals two weeks apart. The observers were blinded for the intraoperative measured rotation.
These measurements were compared to the intraoperative registered rotation of the femoral component; the latter is stored in a therapy report by the CAOS system. This report is an overview of all registered femoral and tibial points, which are needed to register the specific morphology of both tibia and femur as well as the centre of the hip joint and the ankle joint. Furthermore, this report saves, during the several steps of the COAS procedure, final steps after bone cuts have been made (i.e. tibial cut, femoral bone cuts).
Statistical analysis was performed using repeated measure analysis (ANOVA). The intraclass correlations were calculated for the CT measurements for the different observers. The epicondylar axis which was obtained from the CAOS system was compared to the CT measurements of the femoral component using an intraclass correlation coefficient.
Limits of agreement were obtained for the different comparison according to Bland and Altman [6], a graphical tool to measure agreement between two methods. The interpretation of the ICC is similar to that of the Cohen’s Kappa, such that ICC = 0.40–0.59 is moderate interobserver reliability, 0.60–0.79 substantial and 0.80 outstanding [17]. For statistical analysis, SPSS 16.0 was used and the level of significance was set as 0.05.
Results
The rotational alignment of the femoral component was expressed with the CTA. The rotational alignment of the femoral component which was saved in the registry report of the CAOS system was 3.5° (range 2.4–9.6°). In none of the knee prostheses was a cement layer of more than 1 mm detected at the lateral radiograph on the anterior, posterior and/or distal cut.
The mean CTA measured on the postoperative CT scan was 4.0° (range 1.7–7.2°) for observer 1 and 4.4° (range 1.2–9.9, SD 1.5) for observer 2.
The measured CTA on the CT scan showed an intraclass correlation of 0.81 (p < 001) between the two observers. The intraclass correlation coefficient for differences within the observers was 0.84 and 0.82 (p < 0.001), respectively. However, when we compared the angles obtained from the CAOS navigation system with the CTA measurements by both observers on the postoperative CT scans, we found an intraclass correlation of only 0.38 (p = 0.15).
In Fig. 4 a histogram shows the difference between the CAOS and the postoperative CT scans. From this histogram we can see that all differences were between −6 and 6°, and 80% between −3 and 3°. The Bland-Altman plot (Fig. 5) shows no monotonic drift between the two measurements nor a systematic increase in error related to the value of the measurement. The 95% limits of agreement were −4.3 to 5.7°; thus, not only no correlation between CAOS and CT position could be found, but the differences between the two values were also relatively large.
Discussion
The intraoperative position of the femoral component of the knee prosthesis, as determined by the CAOS system, differs from the actual position of the knee prosthesis as measured on a postoperative CT scan. This difference between the intraoperative rotation registered by the navigation system and the actual postoperative CT position has not been published before. Accurate positioning of the components in TKA is very important. The rotation of the femoral component especially influences the final outcome due to its role in flexion stability, kinematics and patellar tracking. The use of navigation in TKA showed more accurate AP alignment; however, little is known about the effect of CAOS navigation systems on rotational alignment [19]. Furthermore, little is known about whether the intraoperative knee component angles are indicative for the actual postoperative component positions. Therefore, the purpose of this study was to evaluate the difference between this intraoperative computer guided femoral rotational alignment with the actual postoperative femoral position, measured using CT scans.
So far, only Han et al. performed a study on rotation and the use of navigation [14]. They found no difference in rotational alignment between CAOS and conventional placement of the femoral component. However, they used a Mann-Whitney U-test to compare the groups, and this test only analyses the mean and standard deviation of the two groups and not the agreement. We used an intraclass correlation coefficient in which the agreement is more important than the mean value of the two groups. Furthermore, in their patients treated with the conventional technique, the PCA was used, and in the navigation group a combination of the epicondylar axis and the flexion gap with the use of laminar spreaders was used; thus, two different techniques were applied.
In general, external rotation of the femoral component of 3° to a maximum of 5° with respect to the posterior condylar line or 0° placement with respect to the transepicondylar line is considered an optimal femoral component position [1, 18]. In this study, the mean intraoperative rotation of the femoral component was 3.5° according to the navigation software, and the mean postoperative rotation measured on CT was 4.2°. Taking this into account, as well as the mean rotational positions at first sight, suggests that there was no significant difference between the intraoperative data and the postoperative situation. However, comparison of each single measurement showed no correlation. Besides, there was still a considerable range of the measurements (2.4–9.6°) in this group of navigated TKAs.
There are several factors that could cause the difference between the intraoperative registered position and the definite postoperative measured position of the femoral component. These can be related to the navigation system, the intraoperative events after the bone cuts have been made and factors related to CT measurement errors.
With respect to the CAOS system, errors can occur during registration and during surgery by, for example, displacement of the markers. To achieve a precise rotational position, the determination of the epicondylar axis, posterior condylar line and Whiteside’s line is crucial. Whilst many opinions are expressed in the literature as to which axes are the most reliable and/or show the least intra-/inter-observer variability, neither one seems to be superior [25]. This supports our finding that CAOS provides information though does not replace clinical judgement. Benjamin et al. [4] compared the different axes and showed that the posterior condylar axis matched within 1° in 64% of the patients in contrast to epicondylar (32%) and Whitesides line (26%). In this navigation module, the planned position of the femoral component was based on the epicondylar axis
Yau et al. [33] also stated that landmark referencing of the axes shows variation because of intraobserver errors and anatomical differences, and thereby leads to variation of the navigation planned implant positioning. This variation is, for example, described for the epicondylar axis. A systematic error of 3° was found using the same navigation module by Van der Linden et al. [30]. Several authors [13, 20] concluded that, because of this problem, preoperative CT scanning is a more appropriate method because of the fact that using computer navigation, rotation is still based on a controversial intraoperative identification of the axes. Also, averaging the different alignment axes will not solve this problem. This was studied by Siston [25]; it will reduce the number of rotational alignment outliers, but they are still present.
To measure the postoperative position of the femoral component we used computed tomography. The most prominent point of the medial epicondyle is required for the CTA. This is much more easily identifiable than the medial sulcus which is required for the posterior condylar angle [29]. By measurement of the ICC within and between the observers, which was 0.84 and 0.82, respectively, it is shown that the measurements using CT had very good reproducibility.
Prosthesis placement might be changed after the bone cuts have been made due to small cement layers. To measure this alignment deviation caused by standard impaction of the components following bone resections, Catani et al. [9] measured the alignment of the bone resections during surgery. The alignment measure was repeated after final tibial and femoral component implantation with cement. The alignment deviation was >1° in the frontal plane of the femur in 20%. However, the rotational position was not evaluated and the influence of the thickness of the cement layer on femoral component position is therefore still unknown. Thus, the positioning of the components in total knee arthroplasty, which mainly involves cementation and impaction of the final components, can introduce an error in alignment, regardless of how accurately the resection planes are made.
In conclusion, the intraoperative CAOS measured rotation of the femoral component differs from the postoperative CT measured position and is therefore not reliable as an absolute value. CAOS can probably help to achieve the optimal position of the femoral component but continuous improvement in methods to accurately identify the rotational position and establish the ideal rotation of the components in total knee arthroplasty is still needed.
References
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Bauwens K, Matthes G, Wich M, Gebhard F, Hanson B, Ekkernkamp A, Stengel D (2007) Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Am 89:261–269
Benjamin J (2008) Determining femoral component position using CAS and measured resection. Clin Orthop Relat Res 466:2745–2750
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Boisgard S, Moreau PE, Descamps S, Courtalhiac C, Silbert H, Moreel P, Michel JL, Levai JP (2003) Computed tomographic study of the posterior condylar angle in arthritic knees: its use in the rotational positioning of the femoral implant of total knee prostheses. Surg Radiol Anat 25:330–334
Boldt JG, Stiehl JB, Munzinger U, Beverland D, Keblish PA (2006) Femoral component rotation in mobile-bearing total knee arthroplasty. Knee 13:284–289
Catani F, Biasca N, Ensini A, Leardini A, Bianchi L, Digennaro V, Giannini S (2008) Alignment deviation between bone resection and final implant positioning in computer-navigated total knee arthroplasty. J Bone Joint Surg Am 90:765–771
Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM (2004) Computer-assisted total knee replacement. A controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the Perth CT Protocol). J Bone Joint Surg Br 86:818–823
Chauhan SK, Scott RG, Breidahl W, Beaver RJ (2004) Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br 86:372–377
Decking R, Markmann Y, Fuchs J, Puhl W, Scharf HP (2005) Leg axis after computer-navigated total knee arthroplasty: a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty 20:282–288
Galaud B, Beaufils P, Michaut M, Abadie P, Fallet L, Boisrenoult P (2008) Distal femoral torsion: comparison of CT scan and intra operative navigation measurements during total knee arthroplasty. Rev Chir Orthop Reparatrice Appar Mot 94:573–579
Han HS, Seong SC, Lee S, Lee MC (2006) Rotational alignment of femoral components in total knee arthroplasty: nonimage-based navigation system versus conventional technique. Orthopedics 29:S148–S151
Jazrawi LM, Birdzell L, Kummer FJ, Di Cesare PE (2000) The accuracy of computed tomography for determining femoral and tibial total knee arthroplasty component rotation. J Arthroplasty 15:761–766
Kamat YD, Aurakzai KM, Adhikari AR, Matthews D, Kalairajah Y, Field RE (2009) Does computer navigation in total knee arthroplasty improve patient outcome at midterm follow-up? Int Orthop 33:1567–1570
Landis JR, Koch GG (1977) An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33:363–374
Laskin RS (1995) Flexion space configuration in total knee arthroplasty. J Arthroplasty 10:657–660
Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C (2007) A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am 89:236–243
Michaut M, Beaufils P, Galaud B, Abadie P, Boisrenoult P, Fallet L (2008) Rotational alignment of femoral component with computed-assisted surgery (CAS) during total knee arthroplasty. Rev Chir Orthop Reparatrice Appar Mot 94:580–584
Mullaji A, Kanna R, Marawar S, Kohli A, Sharma A (2007) Comparison of limb and component alignment using computer-assisted navigation versus image intensifier-guided conventional total knee arthroplasty: a prospective, randomized, single-surgeon study of 467 knees. J Arthroplasty 22:953–959
Oberst M, Bertsch C, Wurstlin S, Holz U (2003) CT analysis of leg alignment after conventional vs. navigated knee prosthesis implantation. Initial results of a controlled, prospective and randomized study. Unfallchirurg 106:941–948
Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE (1996) Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res 331:35–46
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002) Insall award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ (2005) The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am 87:2276–2280
Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A (2003) Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br 85:830–835
Stiehl JB (2009) Comparison of tibial rotation in fixed and mobile bearing total knee arthroplasty using computer navigation. Int Orthop 33:679–685
Stockl B, Nogler M, Rosiek R, Fischer M, Krismer M, Kessler O (2004) Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 426:180–186
Suter T, Zanetti M, Schmid M, Romero J (2006) Reproducibility of measurement of femoral component rotation after total knee arthroplasty using computer tomography. J Arthroplasty 21:744–748
van der Linden-van der Zwaag HM, Valstar ER, van der Molen AJ, Nelissen RG (2008) Transepicondylar axis accuracy in computer assisted knee surgery: a comparison of the CT-based measured axis versus the CAS-determined axis. Comput Aided Surg 13:200–206
van Strien T, van der Linden-van der Zwaag HM, Kaptein B, van EA, Valstar E, Nelissen RG (2009) Computer assisted versus conventional cemented total knee prostheses alignment accuracy and micromotion of the tibial component. Int Orthop 33:1255–1261
Whiteside LA, Arima J (1995) The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res 321:168–172
Yau WP, Leung A, Chiu KY, Tang WM, Ng TP (2005) Intraobserver errors in obtaining visually selected anatomic landmarks during registration process in nonimage-based navigation-assisted total knee arthroplasty: a cadaveric experiment. J Arthroplasty 20:591–601
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
van der Linden-van der Zwaag, H.M.J., Bos, J., van der Heide, H.J.L. et al. A computed tomography based study on rotational alignment accuracy of the femoral component in total knee arthroplasty using computer-assisted orthopaedic surgery. International Orthopaedics (SICOT) 35, 845–850 (2011). https://doi.org/10.1007/s00264-010-1082-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1082-9