Abstract
Background
There is growing evidence suggesting that the occurrence of immune-related adverse events (irAEs) may be a predictor of immune checkpoint inhibitor efficacy. Whether this association extends to all irAEs or just those within particular organs/systems is yet to be resolved. As immune-related thyroid dysfunction (thyroid irAE) is one of the most commonly reported irAEs, this study aims to summarize the available data and determine if thyroid irAE is a surrogate marker for improved cancer outcomes during ICI therapy.
Methods
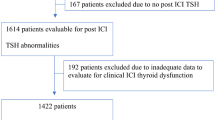
PubMed, EMBASE and Cochrane Library were searched up to July 1st 2021 for studies assessing the relationship between thyroid irAE development during ICI therapy and cancer outcomes. Outcome measures of interest include overall survival (OS) and progression free survival (PFS). Sub-group analyses based on cancer type and adjustment for immortal time bias (ITB) were also performed.
Results
Forty-seven studies were included in the systematic review. Twenty-one studies were included in the OS meta-analysis whilst 15 were included in the PFS meta-analysis. Development of thyroid irAE during ICI therapy was associated with improved OS and PFS (OS: HR 0.52, CI 0.43–0.62, p < 0.001; PFS: HR 0.58, CI 0.50–0.67, p < 0.001). Sub-group analyses involving non-small cell lung cancer populations and studies where ITB was accounted for, observed similar results (HR 0.37, CI 0.24–0.57, p < 0.001) and (HR 0.51, CI 0.39–0.69, p < 0.001), respectively.
Conclusion
Despite the heterogeneity and biases identified, the evidence does suggest that the development of thyroid irAE is associated with anti-tumor effects of ICIs and therefore, can be used as a surrogate marker for clinical response.




Similar content being viewed by others
References
Wolchok JD, Chiarion-Sileni V, Gonzalez R et al (2018) Overall survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med 377:1345–1356
Antonia SJ, Villegas A, Daniel D et al (2017) Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med 377:1919–1929
Borghaei H, Paz-Ares L, Horn L et al (2015) Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 373:1627–1639
Overman MJ, McDermott R, Leach JL et al (2017) Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 18:1182–1191
Yamauchi I, Yasoda A, Matsumoto S et al (2019) Incidence, features, and prognosis of immune-related adverse events involving the thyroid gland induced by nivolumab. PLoS One 14:e0216954
Shankar B, Zhang J, Naqash AR et al (2020) Multisystem immune-related adverse events associated with immune checkpoint inhibitors for treatment of non-small cell lung cancer. JAMA Oncol 6:1952–1956
Zhou X, Yao Z, Yang H et al (2020) Are immune-related adverse events associated with the efficacy of immune checkpoint inhibitors in patients with cancer? A systematic review and meta-analysis. BMC Med 18:87
Hussaini S, Chehade R, Boldt RG et al (2020) Association between immune-related side effects and efficacy and benefit of immune checkpoint inhibitors: a systematic review and meta-analysis. Cancer Treat Rev 92:102134
Cortellini A, Buti S, Agostinelli V et al (2019) A systematic review on the emerging association between the occurrence of immune-related adverse events and clinical outcomes with checkpoint inhibitors in advanced cancer patients. Semin Oncol 45:362–371
Fujii T, Naing A, Rolfo C et al (2018) Biomarkers of response to immune checkpoint blockade in cancer treatment. Crit Rev Oncol Hematol 130:108–120
Gleiss A, Oberbauer R, Heinze G (2018) An unjustified benefit: immortal time bias in the analysis of time-dependent events. Transpl Int 31:125–213
Sterne JAC, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
DerSimonian R, Kacker R (2007) Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 28:105–114
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Kim HI, Kim M, Lee SH et al (2017) Development of thyroid dysfunction is associated with clinical response to PD-1 blockade treatment in patients with advanced non-small cell lung cancer. Oncoimmunology 7:e1375642
Fujisawa Y, Yoshino K, Otsuka A et al (2017) Fluctuations in routine blood count might signal severe immune-related adverse events in melanoma patients treated with nivolumab. J Dermatol Sci 88:225–231
Osorio JC, Ni A, Chaft JE et al (2017) Antibody-mediated thyroid dysfunction during T-cell checkpoint blockade in patients with non-small-cell lung cancer. Ann Oncol 28:583–589
Grangeon M, Tomasini P, Chaleat S et al (2019) Association between immune-related adverse events and efficacy of immune checkpoint inhibitors in non-small-cell lung cancer. Clin Lung Cancer 30:201–207
Haratani K, Hayashi H, Chiba Y et al (2018) Association of immune-related adverse events with nivolumab efficacy in non-small-cell lung cancer. JAMA Oncol 4:374–378
Owen DH, Wei L, Bertino EM et al (2018) Incidence, risk factors, and effect on survival of immune-related adverse events in patients with non-small-cell lung cancer. Clin Lung Cancer 19:e893–e900
Ricciuti B, Genova C, De Giglio A et al (2019) Impact of immune-related adverse events on survival in patients with advanced non-small cell lung cancer treated with nivolumab: long-term outcomes from a multi-institutional analysis. J Cancer Res Clin Oncol 145:479–485
Cortellini A, Chiari R, Ricciuti B et al (2019) Correlations between the immune-related adverse events spectrum and efficacy of anti-PD1 immunotherapy in NSCLC patients. Clin Lung Cancer 20:237-247.e1
Funazo TY, Nomizo T, Ozasa H et al (2019) Clinical impact of low serum free T4 in patients with non-small cell lung cancer treated with nivolumab. Sci Rep 9:17085
Koyama J, Horiike A, Yoshizawa T et al (2019) Correlation between thyroid transcription factor-1 expression, immune-related thyroid dysfunction, and efficacy of anti-programmed cell death protein-1 treatment in non-small cell lung cancer. J Thorac Dis 11:1919–1928
Lei M, Michael A, Patel S et al (2019) Evaluation of the impact of thyroiditis development in patients receiving immunotherapy with programmed cell death-1 inhibitors. J Oncol Pharm Pract 25:1402–1411
Maeda T, Yoshino K, Nagai K et al (2019) Development of endocrine immune-related adverse events and improved survival in advanced melanoma patients treated with nivolumab monotherapy. Eur J Cancer 115:13–16
Peiró I, Palmero R, Iglesias P et al (2019) Thyroid dysfunction induced by nivolumab: searching for disease patterns and outcomes. Endocrine 64:605–613
Sakakida T, Ishikawa T, Uchino J et al (2019) Clinical features of immune-related thyroid dysfunction and its association with outcomes in patients with advanced malignancies treated by PD-1 blockade. Oncol Lett 18:2140–2147
Verzoni E, Cartenì G, Cortesi E et al (2019) Real-world efficacy and safety of nivolumab in previously-treated metastatic renal cell carcinoma, and association between immune-related adverse events and survival: the Italian expanded access program. J Immunother Cancer 7:99
Basak EA, van der Meer JWM, Hurkmans DP et al (2020) Overt thyroid dysfunction and anti-thyroid antibodies predict response to anti-PD-1 immunotherapy in cancer patients. Thyroid 30(7):966–973
Cortellini A, Friedlaender A, Banna GL et al (2020) Immune-related adverse events of pembrolizumab in a large real-world cohort of patients With NSCLC with a PD-L1 expression ≥ 50% and their relationship with clinical outcomes. Clin Lung Cancer 21:498-508.e2
Economopoulou P, Kotsantis I, Papaxoinis G et al (2020) Association of autoimmunity with survival in patients with recurrent/metastatic head and neck squamous cell carcinoma treated with nivolumab. Oral Oncol 111:105013
Eggermont AMM, Kicinski M, Blank CU et al (2020) Association between immune-related adverse events and recurrence-free survival among patients with stage III melanoma randomized to receive pembrolizumab or placebo: a secondary analysis of a randomized clinical trial. JAMA Oncol 6:519–527
España S, Montes Pérez, de Oca A, Marques-Pamies M et al (2020) Endocrine adverse events related to immune-oncology agents: retrospective experience of a single institution. Transl Lung Cancer Res 9:103–110
Lima Ferreira J, Costa C, Marques B et al (2020) Improved survival in patients with thyroid function test abnormalities secondary to immune-checkpoint inhibitors. Cancer Immunol Immunother. https://doi.org/10.1007/s00262-020-02664-y
Kelly K, Manitz J, Patel MR et al (2020) Efficacy and immune-related adverse event associations in avelumab-treated patients. J Immunother Cancer 8:e001427
Kijima T, Fukushima H, Kusuhara S et al (2020) Association between the occurrence and spectrum of immune-related adverse events and efficacy of pembrolizumab in Asian patients with advanced urothelial cancer: multicenter retrospective analyses and systematic literature review. Clin Genitourin Cancer S1558–7673:30163–30164
Kotwal A, Kottschade L, Ryder M (2020) PD-l1 inhibitor-induced thyroiditis is associated with better overall survival in cancer patients. Thyroid 30:177–184
Maillet D, Corbaux P, Stelmes JJ et al (2020) Association between immune-related adverse events and long-term survival outcomes in patients treated with immune checkpoint inhibitors. Eur J Cancer 132:61–70
Bai R, Li L, Chen X et al (2021) Correlation of peripheral blood parameters and immune-related adverse events with the efficacy of immune checkpoint inhibitors. J Oncol 10:9935076
Frelau A, Jali E, Campillo-Gimenez B et al (2021) Prognostic impact of thyroid dysfunctions on progression-free survival in patients with metastatic melanoma treated with anti-PD-1 antibodies. Melanoma Res 31:208–217
Luongo C, Morra R, Gambale C et al (2021) Higher baseline TSH levels predict early hypothyroidism during cancer immunotherapy. J Endocrinol Invest 44:1927–1933
Muir CA, Clifton-Bligh RJ, Long GV et al (2021) Thyroid immune-related adverse events following immune checkpoint inhibitor treatment. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgab263
Street S, Chute D, Strohbehn I et al (2021) The positive effect of immune checkpoint inhibitor-induced thyroiditis on overall survival accounting for immortal time bias: a retrospective cohort study of 6596 patients. Ann Oncol 32:1050–1051
Thuillier P, Joly C, Alavi Z et al (2021) Thyroid dysfunction induced by immune checkpoint inhibitors is associated with a better progression-free survival and overall survival in non-small cell lung cancer: an original cohort study. Cancer Immunol Immunother. https://doi.org/10.1007/s00262-020-02802-6
Zhou Y, Xia R, Xiao H et al (2020) Thyroid function abnormality induced by PD-1 inhibitors have a positive impact on survival in patients with non-small cell lung cancer. Int Immunopharmacol 91:107296
Al Ashi SI, Thapa B, Flores M et al (2021) Endocrine toxicity and outcomes in patients with metastatic malignancies treated with immune checkpoint inhibitors. J Endocr Soc 5:bvab100
Ahn BC, Pyo KH, Xin CF et al (2019) Comprehensive analysis of the characteristics and treatment outcomes of patients with non-small cell lung cancer treated with anti-PD-1 therapy in real-world practice. J Cancer Res Clin Oncol 145:1613–1623
Campredon P, Mouly C, Lusque A et al (2019) Incidence of thyroid dysfunctions during treatment with nivolumab for non-small cell lung cancer: retrospective study of 105 patients. Presse Med 48:e199–e207
Ksienski D, Wai ES, Croteau N et al (2019) Efficacy of nivolumab and pembrolizumab in patients with advanced non-small-cell lung cancer needing treatment interruption because of adverse events: a retrospective multicenter analysis. Clin Lung Cancer 20:e97–e106
Freeman-Keller M, Kim Y, Cronin H et al (2016) Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res 22:886–894
Matsuo M, Yasumatsu R, Masuda M et al (2020) Relationship between immune-related adverse events and the long-term outcomes in recurrent/metastatic head and neck squamous cell carcinoma treated with nivolumab. Oral Oncol 101:104525
Al Mushref M, Guido PA, Collichio FA et al (2020) Thyroid dysfunction, recovery, and prognosis in melanoma patients treated with immune checkpoint inhibitors: a retrospective review. Endocr Pract 26:36–42
D’Aiello A, Lin J, Gucalp R et al (2021) Thyroid dysfunction in lung cancer patients treated with immune checkpoint inhibitors (ICIs): outcomes in a multiethnic urban cohort. Cancers (Basel) 13:1464
Rubino R, Marini A, Roviello G et al (2021) Endocrine-related adverse events in a large series of cancer patients treated with anti-PD1 therapy. Endocrine. https://doi.org/10.1007/s12020-021-02750-w
Paderi A, Giorgione R, Giommoni E et al (2021) Association between immune related adverse events and outcome in patients with metastatic renal cell carcinoma treated with immune checkpoint inhibitors. Cancers (Basel) 13:860
Morimoto K, Yamada T, Takumi C et al (2021) Immune-related adverse events are associated with clinical benefit in patients with non-small-cell lung cancer treated with immunotherapy plus chemotherapy: a retrospective study. Front Oncol. https://doi.org/10.3389/fonc.2021.630136
Lui DTW, Lee CH, Tang V, et al (2021) Thyroid immune-related adverse events in patients with cancer treated with anti-PD1/anti-CTLA4 immune checkpoint inhibitor combination: clinical course and outcomes. Endocr Pract S1530-891X(21)00030-6
Holstead RG, Kartolo BA, Hopman WM et al (2021) Impact of the development of immune related adverse events in metastatic melanoma treated with PD -1 inhibitors. Melanoma Res 31:258–263
Fujisawa Y, Yoshino K, Otsuka A et al (2018) Retrospective study of advanced melanoma patients treated with ipilimumab after nivolumab: Analysis of 60 Japanese patients. J Dermatol Sci 89:60–66
Cortellini A, Friedlaender A, Banna GL et al (2020) Immune-related adverse events of pembrolizumab in a large real-world cohort of patients with NSCLC with a PD-L1 expression ≥ 50% and their relationship with clinical outcomes. Clin Lung Cancer 21:498.e2-508
Paderi A, Giorgione R, Giommoni E et al (2021) Association between immune related adverse events and outcome in patients with metastatic renal cell carcinoma treated with immune checkpoint inhibitors. Cancers (Basel) 13:860
Lisberg A, Tucker DA, Goldman JW et al (2018) Treatment-related adverse events predict improved clinical outcome in NSCLC patients on KEYNOTE-001 at a single center. Cancer Immunol Res 6:288–294
de Filette J, Andreescu CE, Cools F et al (2019) A systematic review and meta-analysis of endocrine-related adverse events associated with immune checkpoint inhibitors. Horm Metab Res 51:145–156
Park R, Lopes L, Saeed A (2021) Anti-PD-1/L1-associated immune-related adverse events as harbinger of favorable clinical outcome: systematic review and meta-analysis. Clin Transl Oncol 23:100–109
Barroso-Sousa R, Barry WT, Garrido-Castro AC et al (2018) Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens: a systematic review and meta-analysis. JAMA Oncol 4:173–182
Hussaini S, Chehade R, Boldt RG et al (2021) Association between immune-related side effects and efficacy and benefit of immune checkpoint inhibitors: a systematic review and meta-analysis. Cancer Treat Rev 92:102134
Cortellini A, Buti S, Agostinelli V et al (2019) A systematic review on the emerging association between the occurrence of immune-related adverse events and clinical outcomes with checkpoint inhibitors in advanced cancer patients. Semin Oncol 46:362–371
Ye Y, Jing Y, Li L et al (2020) Sex-associated molecular differences for cancer immunotherapy. Nat Commun 11:1779
Network NCC (2021) NCCN guidelines version 4.2021 management of immune checkpoint inhibitor-related toxicity https://www.nccn.org/professionals/physician_gls/pdf/immunotherapy.pdf
Chang LS, Barroso-Sousa R, Tolaney SM et al (2019) Endocrine toxicity of cancer immunotherapy targeting immune checkpoints. Endocr Rev 40:17–65
Funding
This work was conducted with support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Y-MMC had substantial contribution in the conception and design of the manuscript, along with its methodology. She also conducted the statistical analyses and was primarily responsible for drafting the manuscript. She was one of two reviewers responsible for the review and selection of studies for both the systematic review and meta-analysis, as well as for the extracting of data from the selected studies. WW had substantial contribution in overseeing and supervising all statistical analyses performed for the meta-analysis. She also contributed to the revisions of the manuscript. BM had substantial contribution in the drafting and revisions of the manuscript. O-PRH had substantial contribution in the conception and design of the manuscript, along with its methodology. He also contributed to the drafting and revisions of the manuscript. He was one of two reviewers responsible for the review and selection of studies for both the systematic review and meta-analysis, as well as for the extracting of data from the selected studies. He also provided supervision and oversight of the project. All authors have given approval for this version of the manuscript to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors (YC, BM, WW and OH) do not have any disclosures or conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheung, YM.M., Wang, W., McGregor, B. et al. Associations between immune-related thyroid dysfunction and efficacy of immune checkpoint inhibitors: a systematic review and meta-analysis. Cancer Immunol Immunother 71, 1795–1812 (2022). https://doi.org/10.1007/s00262-021-03128-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-021-03128-7