Abstract
Th1-type immunity is considered to be required for efficient response to BCG in bladder cancer, although Th2 predisposition of BCG responders has recently been reported. The aim was to evaluate the relationship of Th1 and Th2 components in 23 patients undergoing BCG treatment. Peripheral blood, serum and urine samples were prospectively collected at baseline, during and after BCG. Th1 (neopterin, tryptophan, kynurenine, kynurenine-to-tryptophan ratio (KTR), IL-12, IFN-γ, soluble TNF-R75 and IL-2Rα) and Th2 (IL-4, IL-10) biomarkers as well as CD4 expression in T helper (Th), effector and regulatory T cells were determined. Local immune cell subsets were measured on formalin-fixed, paraffin-embedded cancer tissue by immunohistochemistry to examine expression of transcription factors that control Th1 (T-bet) and Th2-type (GATA3) immunity. We confirmed a Th2 predisposition with a mean GATA3/T-bet ratio of 5.51. BCG responders showed significantly higher levels of urinary (p = 0.003) and serum neopterin (p = 0.012), kynurenine (p = 0.015), KTR (p = 0.005), IFN-γ (p = 0.005) and IL-12 (p = 0.003) during therapy, whereas levels of IL-10 decreased significantly (p < 0.001) compared to non-responders. GATA3/T-bet ratio correlated positively with serum neopterin (p = 0.008), IFN-γ (p = 0.013) and KTR (p = 0.018) after the first BCG instillation. We observed a significant increase in CD4 expression in the Th cell population (p < 0.05), with only a modest tendency toward higher frequency in responders compared to non-responders (p = 0.303). The combined assessment of GATA3/T-bet ratio, neopterin and KTR may be a useful biomarker in predicting BCG response. Th2-promoting factors such as GATA3 may trigger Th1-type immune responses and thus contribute to the BCG success.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After decades of skepticism, immunotherapy is poised to become a mainstay of cancer treatment [1]. Currently, the most promising approach in activating therapeutic antitumor immunity is the blockade of immune checkpoints [2] as well as the use of genetically engineered T cells with chimeric antigen receptor (CAR) directed against tumor-associated antigens [3]. Treatment with Bacillus Calmette–Guérin (BCG) belongs to the most successful cancer immunotherapies, and in high-risk, non-muscle-invasive bladder cancer (NMIBC), it is the standard adjuvant treatment according to the European Association of Urology (EAU) guidelines [4]. Forty years after its introduction [5], the exact immune mechanism of BCG-induced antitumor activity is still not fully understood. Following BCG instillations, intravesical BCG–fibronectin complexes are internalized at the tumor resection site [6]. Antigen-presenting cells in the urothelium can phagocytose BCG and present BCG-derived antigens to CD4+ T cells. In vitro work by Brandau et al. has demonstrated that BCG activates natural killer (NK) cells in a monocyte-dependent manner [7]. It is well established that innate lymphocytes including NK cells not only participate in the early innate response but also promote and shape the subsequent adaptive response by triggering dendritic cell maturation [8] and are therefore essential for effective BCG immunotherapy [9, 10]. Different cytokines such as interleukin (IL)-1, IL-2, IL-6, IL-7, IL-8, IL-10, IL-12, tumor necrosis factor-(TNF)-α and interferon (IFN)-γ are released and can be detected in patients treated with BCG [11–13]. Thus, BCG can induce the production of both Th1-type and Th2-type cytokines. This fact was confirmed in vitro showing that BCG stimulates cultured murine dendritic cells, which are able to induce both IL-12 and IL-10, resulting in a mixed, nontargeted Th1 and Th2 immune response [14]. However, a predominant Th1 cell-mediated immunity with an enhanced recognition of cancer cells through infiltrating effector cells into the bladder wall is required for subsequent BCG response [15]. IL-12- or IFN-γ-depleted animals were BCG-resistant with a poor cancer-specific survival [16], whereas therapeutic strategies administering BCG along with Th1 cytokines and concurrent blocking of Th2 cells may enhance BCG-induced IFN-γ production and BCG vaccine efficacy [17–20]. Moreover, significant increases in urine concentrations of Th1-type cytokines during treatment were noticed in BCG responders [21, 22].
IFN-γ is an important stimulus for the enzyme GTP cyclohydrolase (GCH-I) in human monocyte-derived macrophages and dendritic cells, which induces neopterin production reflecting cellular immune activation [23, 24]. In parallel, IFN-γ activates the enzyme indoleamine 2,3-dioxygenase (IDO1), which converts tryptophan to kynurenine resulting in increased tryptophan breakdown, and elevated kynurenine-to-tryptophan ratio (KTR), [23]. Therefore, neopterin production and tryptophan breakdown are surrogate markers of IFN-γ production and thus of an ongoing Th1-type immune response. Currently, only a letter to the editor reported monitoring of neopterin in bladder cancer patients during intravesical BCG therapy [25]. Moreover, intravesical instillations of autologous IFN-γ-activated macrophages resulted in an increase in urinary neopterin [26].
It is well known that differentiation of type 1 and type 2 Th cells [27] as well as innate lymphoid cells [28] is controlled by the transcription factors T-bet and GATA3. Interestingly, a genome-wide analysis has revealed that T-bet is sufficient to induce GATA3 binding at Th1 specific sites, indicating its direct influence and responsibility for the redistribution of GATA3 in Th1 cells [29].
Recently, we confirmed a Th2 predisposition (GATA3>T-bet) of tumor-infiltrating immune cells in high-risk NMIBC patients with response to BCG [30]. The aim of the present follow-up study was to examine the relation between such a Th2 predisposition and the actual functional phenotype during treatment as a potential biomarker of BCG response.
Materials and methods
Patients
This prospective study was approved by the local ethical committee of the Medical University of Innsbruck (study number AN2014-0121; 336/4.3), and written informed consent was obtained before study inclusion. All patients with primary NMIBC who had undergone transurethral resection of the bladder (TURB) from March 2014 to April 2015 with consecutive intravesical BCG immunotherapy were enrolled in this study. A second TURB was performed in all patients (except primary, isolated carcinoma in situ) before starting BCG induction and maintenance at our outpatient department. Each instillation contained 2 × 108–3 × 109 viable units from live attenuated BCG bacteria strain seed RIVM derived from seed 1173-P2 (BCG Medac, Wedel, Germany). Follow-up included cystoscopy and urinary cytology (voided urine and bladder washing) 3-monthly, and upper urinary tract imaging (CT urography or intravenous urography) once a year and in case of cancer recurrence [4]. A muscle-invasive bladder cancer detected during follow-up or a high-grade recurrence after completion of therapy was defined as BCG failure. BCG responders were defined as patients without any recurrence or evidence of disease based on follow-up cystoscopy and urinary cytology. A flowchart of the study design is shown in Fig. 1.
Sample collection, preparation and cryopreservation
Heparinized whole blood, serum and urinary samples were collected at 10 different time points: baseline (before first BCG instillation), during BCG induction (7 days after each of the six BCG instillations) as well as during follow-up (at 3, 6 and 9 months). Peripheral blood mononuclear cells (PBMCs) were prepared from heparinized whole blood by Ficoll density centrifugation, and aliquots (5 × 106 cells) were cryopreserved in liquid nitrogen. Serum samples were obtained under standard conditions, clotted at 4–8 °C and then centrifuged at 3200 rpm for 6 min. Aliquots of 1.8 ml were stored at −80 °C.
Measurement of Th1- and Th2-related inflammatory metabolites, cytokines and soluble cytokine receptors
Concentrations of serum neopterin were determined by a commercially available ELISA according to the manufacturer’s instructions (BRAHMS Diagnostica, Hennigsdorf, Germany). Determination of urinary neopterin was performed using reversed phase (e.g., C18) HPLC with Sörensen phosphate buffer (e.g., 0.015 M, pH = 6.4, flow rate = 1.0 ml/min). Urinary neopterin was detected by measurement of its natural fluorescence (excitation wavelength 353 nm, emission wavelength 438 nm). To exclude an inflammation as a cause of neopterin increase, serum levels of C-reactive protein (CRP) were measured at the same time points. Creatinine concentrations were measured in parallel in the same chromatographic run by detection of its UV absorption at 235 nm. Measurement of kynurenine and tryptophan levels was taken by HPLC as described previously [31, 32], using an UV-spectrometric detector (SPD-6A, Shimadzu), a fluorescence detector (model 360, Varian ProStar), a Varian ProStar HPLC system with a solvent delivery module 210 and an autosampler (model 400, Varian ProStar). Kynurenine and tryptophan standards were purchased from Sigma (Steinheim, Germany). KTR was calculated and expressed as μmol/mmol [31]. Levels of urinary sIL-2Rα, sTNF-R75 and serum IFN-γ, IL-12 and IL-10 were determined by ELISA (R&D Systems Europe, Ltd., Abingdon, UK) following the manufacturer’s protocol.
Flow cytometric analyses (FACS)
Subset analyses of freshly isolated non-activated PBMCs were performed to determine dynamic changes of the CD4 expression in Th cells, effector T cells (Teff) and regulatory T cells (Treg). CD3+ T cells were selectively analyzed for the expression of CD4 and CD25. Teff (CD4+CD25highCD161+) cells were identified by additional staining of CD161, a pan-cancer prognostic gene (http://precog.stanford.edu). CD161 defines T cells with a conserved transcriptional signature and the ability to perform T cell receptor-independent, innate-like IFN-γ production in response to IL-12 and IL-18 [33]. This is in line with our own recent work demonstrating that CD4+CD161+ T cells produce IFN-γ in response to dendritic cell stimulation [34]. In contrast, Treg cells were identified by high-level expression of CD25 and additional expression of CD39 (Treg cells: CD4+CD25+CD39+ cells), [35]. The following fluorophore-conjugated monoclonal antibodies were used for phenotyping of PBMCs: anti-CD3 (UCHT-1-BV510; BD Biosciences), anti-CD4 (MT466-FITC; Miltenyi Biotec), anti-CD25 (2A3-PE; BD Biosciences), anti-CD39 (TU66-BV421; BD Biosciences) and anti-CD161 (HP-3G10-PerCP-Cy5.5; eBioscience). Cells were stained in PBS containing 0.5% FCS and 50 μg/ml human IgG (Octapharma) to block Fc γ receptors. After incubation for 30 min at 4 °C, cells were washed two times, resuspended and analyzed in a FACSCanto II flow cytometer using the FACS Diva 6.1.2 as well as FlowJo V7.2.5 software (BD Biosciences). Fixable viability dye eFluor 780 was used to label dead cells, and eFluor 780-negative cells were gated for further analysis (live cell selection), Supplementary Figure. 1.
Immunohistochemistry (IHC)
To evaluate the predisposition for a Th1/Th2 tumor microenvironment prior to BCG, the density of Th1 and Th2 cells in tumor-infiltrating immune cells was measured on formalin-fixed, paraffin-embedded tissue sections of bladder cancer (in the lamina propria without invasion, at the invasive front, within the neoplastic urothelium and within the papillary stroma) by immunohistochemistry, using a T-bet antibody (monoclonal rabbit antihuman T-bet, MRQ-46, prediluted, Roche) and a GATA3 antibody (monoclonal mouse antihuman GATA3, L50-823, prediluted, Roche), which we had already validated in a recently work [30]. IHC staining was performed using an automated immunostainer (BenchMark ULTRA, Ventana Medical Systems, Tucson, US) according to the manufacturer’s protocol. We manually counted the total density of positive cells for each subset in up to 5 high-power fields (HPF) in each region, using the same field of view in consecutive slides. Microscope images were taken with an Olympus BX50 microscope (40x magnification) equipped with the ProgResC10plus camera (Jenoptik, Jena, Germany). IHC evaluation was performed by an experienced uropathologist.
Statistics
Descriptive statistics (absolute and relative frequencies for qualitative data; mean and standard deviation (SD) for quantitative data) are given for all variables of interest. Bias-corrected and accelerated 95% bootstrapping confidence intervals (CIs) based on 2000 iterations were calculated for the means of all biomarkers at all time points. Changes over time in parameters were assessed using the Skillings–Mack test designed for block designs with missing observations [36]. Differences between BCG responders and non-responders were evaluated using a mixed model for repeated measurements with BCG response, time point and the interaction term as fixed effects and an AR(1) model for the within-subject covariance structure. Differences between single time points were evaluated using Mann–Whitney U tests. Correlations between parameters were assessed with Spearman’s ρ correlation coefficient (r s). The predictive power of biomarker levels on BCG response was evaluated by plotting receiver operating characteristic (ROC) curves and calculating the area under the curve (AUC). Expression levels were compared between tumor areas with the Friedman test and Wilcoxon signed-rank tests for pairwise comparisons. A significance level of α = 0.05 (two-tailed) was applied for all p values. Statistical analyses were performed using SPSS version 22 software (IBM Corp., Armonk, NY). Graphics were produced with Microsoft Excel and GraphPad PrismTM6 (GraphPad Software Inc., La Jolla, CA).
Results
Patients’ characteristics
A total of 23 (20 male and 3 female) patients with a mean (range) age of 71.3 (55–80) years were included. Histopathological evaluation confirmed a primary, high-risk NMIBC according to the European Organization for Research and Treatment of Cancer (EORTC) scoring system and risk tables [37]. Three patients showed low-grade carcinomas, while 20 (87.0%) of 23 patients had a high-grade cancer according to the WHO 2004 classification. Second TURB was performed in 19 (82.6%) patients, with tumor-free status in 12 (63.1%) patients, respectively. Descriptive and histopathological characteristics are shown in Supplementary Table 1. During a mean (range) follow-up of 16.2 (13–25) months, 19 (82.6%) patients were classified as BCG responders, while four (17.4%) patients showed BCG failure (multifocal, pT1 high-grade urothelial carcinoma and concurrent CIS) after a mean (range) follow-up of 7.5 (4–10) months. All those patients with BCG failure subsequently underwent radical cystectomy.
Th2 predisposition of tumor-infiltrating immune cells prior to BCG therapy
IHC analysis showed a Th2 predisposition of tumor-infiltrating immune cells in therapy-naive patients: The mean (±SD, range) number of GATA3+ or T-bet+ immune cells and the GATA3/T-bet ratio was 340.2 (±288, 55–1258), 90.8 (±71.4, 12–289) and 5.5 (±5.3, 1.1–23.8) in all patients, respectively (Fig. 2a). Moreover, a GATA3/T-bet ratio >2 was confirmed in 20 (86.9%) of 23 patients and in 18 (94.7%) of 19 responders. Significant differences in the localization pattern and the density of immune cells between the four tumor regions were confirmed for T-bet (p < 0.001) and GATA3 (p < 0.001). The highest infiltration of GATA3+ (266.9 ± 226.8) and T-bet+ (56.4 ± 50.9) T cells was measured in the lamina propria without invasion, followed by the invasive front (48.3 ± 139.8 for GATA3; 15.2 ± 41 for T-bet; p < 0.001), the papillary tumor stroma (24.7 ± 22.7 for GATA3; 14.5 ± 16.7 for T-bet) and finally within the neoplastic urothelium (0.3 ± 1.0 for GATA3; 4.7 ± 6.3 for T-bet, p < 0.001), Fig. 2b, c. By analyzing differences in the expression of GATA3+ and T-bet+ immune cells between BCG response and failure, we found no statistically significant differences concerning GATA3, T-bet and GATA3/T-bet ratio. Nevertheless, BCG responders pointed out a clear tendency toward increased GATA3+ T cell counts (response vs. failure; 372.6 ± 303.6 vs. 186 ± 130.1, p = 0.218) and increased GATA3/T-bet ratio (6.2 ± 5.7 vs. 2.4 ± 1.1, p = 0.081), while the mean (±SD) T-bet+ cell expression was similar (94.1 ± 76.2 vs. 75 ± 45.6, p = 0.785), Fig. 2d. In BCG failure, post-BCG tumor tissue analysis revealed no dynamic changes (mean ± SD) for GATA3 (199 ± 91.7), T-bet (64 ± 30.8) and GATA3/T-bet ratio (2.1 ± 1.8) compared to baseline. Significant positive correlations between GATA3 and T-bet (r s = 0.74, p < 0.001) were identified, while T-bet correlated inversely with GATA3/T-bet ratio (r s = −0.44, p = 0.03), Fig. 2e, f. Representative IHC images of two patients with a higher density of GATA3+ T cells compared to T-bet+ T cell count are shown in Fig. 2g–j.
GATA3 and T-bet expression of tumor-infiltrating immune cells prior to BCG therapy. a Distribution of GATA3+, T-bet+ T cells and GATA3/T-bet ratio in all patients; data represent mean ± SEM. b, c Abundance of GATA3+ and T-bet+ T cells based on analyzed tumor areas. Data represent mean ± SEM. *p < 0.05; **p < 0.01; ***p < 0.001; Friedman’s tests and Wilcoxon’s signed-rank tests. d Frequency of GATA3+, T-bet+ tumor-infiltrating T cells and GATA3/T-bet ratio with respect to treatment outcome (response vs. failure). Data represent mean ± SEM; Mann–Whitney U test. e, f Correlation analysis (and confidence bands) of GATA3, T-bet and GATA3/T-bet ratio; *p < 0.05; **p < 0.01; ***p < 0.001. g Superficially invasive bladder cancer with a high count of GATA3+ tumor-infiltrating lymphocytes and h low expression of T-bet+ T cells; Scale bar ~40 µm; i carcinoma in situ with few GATA3+ T cells and j only one intravascular T-bet+ T cell (marked with *); Scale bar ~40 µm. LP lamina propria without invasion, IF invasive front, NU neoplastic urothelium, PS papillary stroma, r s Spearman’s rank correlation coefficient
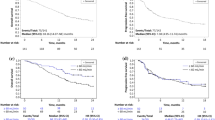
Responders displayed increased levels of Th1-related inflammatory metabolites and decreased concentrations of IL-10 compared to non-responders
Response to BCG has previously been linked to an increase in Th1-related cytokines during treatment [21, 22]. Neopterin production and tryptophan degradation, measurable in serum, are strongly inducible by the Th1-type cytokine IFN-γ [38] and thus may reflect Th1 signals induced locally within the bladder by BCG. In our study population, we observed significant time-dependent changes for serum tryptophan (p = 0.024), IFN-γ (p = 0.009), IL-12 (p = 0.005) and IL-10 (p = 0.048), and a tendency toward an increase in serum (nmol/l; p = 0.056) and urinary (µmol/mol creatinine; p = 0.059) neopterin production during BCG therapy. Dichotomizing into patients with BCG response and failure, we noticed significantly higher increases over the course of time in BCG responders compared to non-responders, for serum neopterin (p = 0.012), serum kynurenine (μmol/l; p = 0.015), serum KTR (μmol/mmol; p = 0.005), urinary neopterin (p = 0.003), serum IFN-γ (pg/ml; p = 0.005) and IL-12 (pg/ml; p = 0.003) concentrations, whereas the levels of Th2 cytokine IL-10 (pg/ml; p < 0.001) were significantly lower in responders compared to non-responders (Figs. 3, 4, 5). At baseline, only urinary neopterin levels were significantly higher in BCG responders compared to BCG failure (mean ± SD, 219 ± 133 vs. 107 ± 38.2; p = 0.021), Fig. 4. ROC analysis showed that the best cutoff (=highest Youden Index: 0.789) for urinary neopterin was ≥137.5 μmol/mol creatinine, with 78.9% sensitivity and 100% specificity in the prediction of BCG response [area under the curve (AUC) = 0.862; 95% CI 0.707–1.00; p = 0.026].
Levels of serum neopterin and tryptophan degradation at baseline, during and after BCG therapy. Patients were stratified by treatment outcome (BCG response vs. failure). Data represent mean ± 95% confidence interval (CI); *p < 0.05; **p < 0.01; ***p < 0.001; overall p value from a mixed model analysis for repeated measures between responders and non-responders; Mann–Whitney U tests for single time point comparisons. KTR kynurenine-to-tryptophan ratio
Levels of urinary neopterin, sTNF-R75 and sIL-2Rα (pro creatinine) at baseline, during and after BCG therapy. Patients were stratified by treatment outcome (BCG response vs. failure). Data represent mean ± 95% confidence interval (CI); *p < 0.05; **p < 0.01; ***p < 0.001; overall p value from a mixed model analysis for repeated measures between responders and non-responders; Mann–Whitney U tests for single time point comparisons. s soluble, TNF tumor necrosis factor, IL interleukin
Levels of serum IFN-γ, IL-12, IL-10 and IL-4 (pg/ml) at baseline, during and after BCG therapy. Patients were stratified by treatment outcome (BCG response vs. BCG failure). Data represent mean ± 95% confidence interval (CI); *p < 0.05; **p < 0.01; ***p < 0.001; overall p value for changes over time points by Skillings–Mack test; p value from a mixed model analysis for repeated measures between responders and non-responders; Mann–Whitney U tests for single time point comparisons between responders and non-responders. IL interleukin
With regard to changes from baseline to the time after the first BCG instillation, BCG responders could be identified by an increased level of serum neopterin (mean ± SD, 22.2 ± 25.9 vs. 7.9 ± 2.3; p = 0.044), serum KTR (mean ± SD, 51.8 ± 24.6 vs. 30.7 ± 7.2; p = 0.024), serum IFN-γ (mean ± SD, 15.9 ± 15.3 vs. 2.1 ± 1.1; p = 0.003) and urinary neopterin (mean ± SD, 328 ± 336 vs. 117 ± 17.6; p = 0.016). Dynamic changes in serum kynurenine concentrations were observed after completed BCG induction: BCG responders displayed a significant increase in 3 months (mean ± SD, 55.7 ± 19.9 vs. 27.6 ± 4.8; p = 0.001), 6 months (mean ± SD, 54.3 ± 19.2 vs. 33.1 ± 13.0; p = 0.014) and 9 months (mean ± SD, 60.9 ± 20.3 vs. 28.8 ± 6.4; p = 0.028) after BCG induction in comparison with BCG failure. In contrast, no significant differences of serum IL-4, urinary sIL-2Rα or sTNF-R75 levels could be noticed in response to BCG therapy, Figs. 3, 4 and 5.
Significant correlations between urinary and serum Th1-type immune response-associated markers at baseline
As a next step, we investigated the extent to which urinary and serum neopterin production correlated with tryptophan breakdown. Correlation analyses revealed significant associations of serum neopterin with urinary neopterin (r s = 0.761, p < 0.001), serum tryptophan (r s = -0.395, p = 0.069), serum kynurenine (r s = 0.783, p < 0.001), serum KTR (r s = 0.817, p < 0.001) and serum IFN-γ (r s = 0.462, p = 0.026). Moreover, urinary sTNF-R75 correlated significantly with urinary sIL-2Rα (r s = 0.744, p < 0.001), Supplementary Figure 2.
Intratumoral GATA3/T-bet ratio correlated with serum neopterin, IFN-γ and KTR levels after first BCG instillation
Consistent with the hypothesis that a predominant Th2 tumor microenvironment relates to a functional Th1 response during BCG treatment, we confirmed a positive correlation between GATA3/T-bet ratio prior BCG induction and levels of serum neopterin (r s = 0.533, p = 0.008), IFN-γ (r s = 0.505, p = 0.013) and KTR (r s = 0.508, p = 0.018) after the first BCG instillation, respectively.
CD4 expression in Th cells increased significantly during BCG therapy
CD3+ and CD4+ T cells as well as Treg cells have shown to differentially influence BCG vaccine efficacy [39, 40], being potential candidates for monitoring response to BCG immunotherapy. As shown in Fig. 6a, the CD4 expression in Th cells changed significantly during BCG induction (p = 0.049). In detail, the CD4 expression in Th cells increased steadily from baseline (mean ± SD, 2144.3 ± 1132.8) to the third BCG instillation (2770.2 ± 891.8), respectively (Fig. 6a). Based on therapy outcome, BCG responders showed a tendency toward an increased CD4 expression in Th cells during treatment compared to BCG failure, already after the first BCG instillation (2686.1 ± 995.3 vs. 1931.3 ± 261.1; p = 0.109), but without statistical significance, Fig. 6b. In contrast, the CD4 expression in CD4+CD25+CD39+ Treg and CD4+CD25highCD161+ Teff cell populations remained relatively stable in the total population as well as stratified by therapy response (Fig. 6c–f). Moreover, we noticed no significant differences neither in the CD4+/Treg ratio of the total study population (Fig. 6g) nor in the change of the CD4+/Treg ratio during therapy between responders and non-responders (Fig. 6h). However, BCG responders showed a trend toward increased CD4+/Treg ratio compared to BCG failure (after three instillations, 1.26 ± 0.85 vs. 0.69 ± 0.12, p = 0.571). In addition, we observed no significant correlations between the CD4 expression in Th cells, Treg and Teff cells, and the serum concentrations of neopterin and tryptophan degradation.
CD4 expression in the Th cell population, CD4+CD25+CD39+ Treg cells and CD4+CD25highCD161+ Teff cells, and CD4+/Treg ratio. a Significant changes in the CD4 expression in Th cells at baseline and during treatment in all patients; Skillings–Mack test; scatter dot plot. b CD4 expression in Th cells at baseline and throughout treatment, depending on therapeutic outcome (response vs. failure); mixed model analysis for repeated measures and Mann–Whitney U tests for single time point comparisons. Data represent mean ± SD; c no significant dynamic changes concerning the CD4 expression in Treg at baseline and during treatment in all patients; Skillings–Mack test; scatter dot plot. d CD4 expression in Treg cells at baseline and throughout treatment, depending on therapeutic outcome (response vs. failure); mixed model analysis for repeated measures and Mann–Whitney U tests for single time point comparisons. Data represent mean ± SD; e no significant dynamic changes concerning the CD4 expression in Teff cells at baseline and during treatment in all patients; Skillings–Mack test; scatter dot plot. f CD4 expression in Teff cells at baseline and throughout treatment, depending on therapeutic outcome (response vs. failure); mixed model analysis for repeated measures and Mann–Whitney U tests for single time point comparisons. Data represent mean ± SD; g no significant dynamic changes concerning the CD4 expression in total CD4+/Treg ratio at baseline and during treatment in all patients; Skillings-Mack test; Scatter dot plot. h CD4 expression in CD4+/Treg ratio at baseline and throughout treatment, depending on therapeutic outcome (response vs. failure); mixed model analysis for repeated measures and Mann–Whitney U tests for single time point comparisons. Data represent mean ± SD; *p < 0.05; **p < 0.01; ***p < 0.001; MFI mean fluorescence intensity
Discussion
Immunity to pathogens including mycobacteria is mediated by type 1 effector Th cells (Th1 cells), which produce IFN-γ [27]. Whereas the T cell transcription factor T-bet (encoded by Tbx21) has a fundamental role in coordinating a type 1 immune response, GATA3 is considered to be the master regulator of the Th2 cell differentiation program characterized by the production of IL-4, IL-5 and IL-13. T-bet also promotes Th1-type responses by preventing GATA3-mediated Th2 cell development [41, 42]. Despite this established concept of mutually exclusive Th cell differentiation, there is also evidence that Th2-type cytokines such as IL-4 are important for memory T cell generation [43] and for the development of CD8+ T cell immunity against intracellular parasites [44].
A Th2 (GATA3>T-bet) predisposition has been reported in different cancer entities and metastatic lymph nodes and was found to be associated with cancer recurrence, progression and poor survival [45–48]. This fact may support the hypothesis of an inverse correlation of GATA3 and T-bet expression, suggesting that the presence of Th2 immune cells limits functional Th1-type responses within the tumor microenvironment. In the present study, we observed a positive correlation between GATA3 and T-bet expression in tumor-infiltrating immune cells. In detail, when GATA3 expression was high, also T-bet was increased and vice versa. Our present findings together with results recently published by our study group [30] clearly indicate a Th2 predisposition of tumor-infiltrating immune cells in BCG responders. However, increased levels of GATA3 expression and GATA3/T-bet ratio were significantly associated with a prolonged, and not a poor recurrence-free survival [30]. Moreover, our current data also showed the tendency toward increased numbers of GATA3+ immune cells in BCG responders compared to BCG failure. These results are comparable with the trial by Nunez-Nateras et al. [49] analyzing the pretreatment immunologic tumor microenvironment within tumor-infiltrating lymphocytes. They also showed an increased pretherapeutic GATA3/T-bet ratio in responders in comparison with BCG failure.
Using real-time PCR to asses the gene expression of GATA3 and T-bet, a reduced Th2 phenotype (decreased GATA3 expression) correlated with disease aggressiveness (high-grade tumors and muscle-invasive status) and a poor cancer-specific survival in bladder cancer [50]. In line with this observation, we observed that the Th2 cytokine IL-4 can directly suppress the growth of tumor cells [51]. Whereas GATA3 expression remained mostly negative in prostate and renal cell carcinoma, up to 70% of invasive urothelial carcinomas were GATA3 positive in one study [52]. However, real-time PCR analysis confirmed higher expression of T-bet among BCG responders as compared to BCG failure (p = 0.02), whereas heavy smokers with low expression levels of GATA3 were poor responders to BCG (p = 0.01), [50].
Focusing on tumor cells, GATA3 has been shown to prevent bladder cancer progression and metastasis by inhibiting cell migration and invasion as well as epithelial-to-mesenchymal transition in vitro [53]. On the contrary, strong expression of GATA3 was associated with progression and poor cancer-specific survival in muscle-invasive bladder tumors [54]. Thus, the role of GATA3 has to be further validated and needs to be interpreted with caution. A possible explanation of these conflicting results may be the interaction of GATA3 with steroid hormone receptor signals influencing bladder cancer growth adversely by both stimulatory and inhibitory effects via androgen receptor (AR), estrogen receptor (ER)α and/or ERβ [55, 56]. For example, GATA3 expression correlated with a loss of ERβ as well as with AR/ERα overexpression in bladder cancer [54].
It is well established that Th1-type immunity is required for effective BCG-induced antitumor activity in bladder cancer. BCG efficacy may be increased by ex vivo tumor antigen-loading and dendritic cell activation as BCG stimulated dendritic cells to secrete TNF-α, which is responsible for phenotypic and functional changes [57]. Ponticiello et al. [58], for instance, noticed a significant increase in the CD4+ Th1 subsets during BCG therapy. Moreover, BCG resulted in an increase in Th1 cytokines and lower levels of Th2 cytokines during therapy in vitro and in humans [13, 21, 22, 59, 60]. Moreover, parenteral exposure to BCG before instillations triggered an accelerated T cell entry into the bladder in vitro, with an improved recurrence-free survival in patients [60]. Therefore, shifting the Th2 dominant immunologic landscape toward a Th1 response during therapy seems to be an important mechanism for adequate BCG response [61]. Another likely point of view is that a certain Th2 capacity is necessary for the generation of an adequate Th1 response. For instance, exposure to the Th2 cytokine IL-4 has been shown to result in an enhanced CD8+ T cell response to pathogens, improving a proinflammatory Th1 immune response [43]. However, the exact mechanism how IL-4 alters the frequency of CD8+ T cells in humans is still unclear. In mice, IL-4-producing NKT cells correlated with thymic innate memory CD8+ T cells [62]. In renal cell carcinoma, IL-4 and TNF-α synergistically induced apoptosis and cytokine production in vitro, promoting the recruitment of different immune effector cells [51]. Thus, simultaneous induction of both Th1 and Th2 response seems to be necessary for efficient systemic antitumor activity [63, 64]. As an example, a Th2-biased response to MAGE-6 epitopes prior to treatment shifted to a Th1-mediated response after therapy in two patients (renal cell carcinoma and melanoma) with complete therapeutic response [65]. Our present results confirm this view, since patients with Th2 predominant tumor-infiltrating immune cells displayed a Th1 functional phenotype during BCG induction.
IFN-γ-induced neopterin production and tryptophan breakdown are typical markers for Th1-activated cell-mediated immunity [23, 24]. So far, only a letter to the editor assessed changes in neopterin levels during BCG. Mack et al. [25] showed for the first time in 30 patients that BCG response was associated with a significant peak of serum and urinary neopterin after each BCG instillation as a sign of a Th1 cell-mediated immune activation. Our results are in line with these data as BCG responders also displayed higher levels of urinary and serum neopterin during intravesical BCG induction. In addition, we demonstrate for the first time enhanced tryptophan breakdown in the serum of BCG responders. Moreover, concentrations of neopterin correlated significantly with those for tryptophan breakdown at each time point confirming that IFN-γ induces simultaneously induces two different biochemical pathways: first, deprivation of tryptophan by IDO1; second, neopterin and reactive oxygen species (ROS) production by GCH-I [66]. Moreover, it is remarkable that neopterin and tryptophan metabolites can be detected in human serum as surrogate markers of a local IFN-γ response occurring in the bladder or the draining lymph nodes after BCG therapy.
As a result of a chronically activated immune system, also counter-regulatory and immunosuppressive mechanisms can be activated with decreased T cell responsiveness and development of immunodeficiency as a consequence of Treg cell expansion [67, 68]. A positive correlation was found between high IDO1 expression in bone marrow-derived mesenchymal stem cells and elevated percentage of Treg cells in acute myeloid leukemia [69]. Therefore, the proportion of CD4+CD25+CD39+ Treg cells was analyzed in PMBCs at baseline, during and after BCG therapy. However, we noticed no significant correlations between serum levels of neopterin or tryptophan degradation and distribution of Treg cells in PBMCs. Nevertheless, BCG responders showed the tendency toward increased Treg cells compared to BCG failure, but without statistical significance.
The obvious limitation of this prospective pilot study is the relatively small sample size of 23 patients, which restricts statistical methods of interpretation. Therefore, further prospective and multi-institutional randomized trials with sufficient statistical power and long-term follow-up are required to validate these preliminary findings and to verify in detail the prognostic role of Th1-related inflammatory metabolites in the context of Th2-driving transcription factor overexpression.
Conclusions
In patients receiving intravesical BCG therapy, a general intratumoral Th2 predisposition at the level of transcription factors (GATA3>T-bet) was combined with an increased productive Th1-type immunity in responders compared to non-responders. A better understanding of Th1 regulation by Th2 components at the molecular level would be helpful in developing a more efficient and targeted cancer immunotherapy, particularly in bladder cancer patients with BCG failure.
Abbreviations
- AR:
-
Androgen receptor
- AUC:
-
Area under the curve
- BCG:
-
Bacillus Calmette–Guérin
- CAR:
-
Chimeric antigen receptor
- ER:
-
Estrogen receptor
- ELISA:
-
Enzyme-linked immunosorbent assay
- FACS:
-
Fluorescence-activated cell sorting
- GCH-I:
-
GTP cyclohydrolase
- HPLC:
-
High-performance liquid chromatography
- IDO:
-
Indoleamine 2,3-dioxygenase
- IFN:
-
Interferon
- IL:
-
Interleukin
- KTR:
-
Kynurenine-to-tryptophan ratio
- NKT:
-
Natural killer T cell
- NMIBC:
-
Non-muscle-invasive bladder cancer
- PBMC:
-
Peripheral blood mononuclear cell
- ROC:
-
Receiver operating characteristic
- ROS:
-
Reactive oxygen species
- Th:
-
T helper
- Teff :
-
Effector T cell
- Treg :
-
Regulatory T cell
- TNF:
-
Tumor necrosis factor
- TURB:
-
Transurethral resection of the bladder
References
Couzin-Frankel J (2013) Breakthrough of the year 2013. Cancer immunotherapy. Science 342(6165):1432–1433. doi:10.1126/science.342.6165.1432
Pardoll DM (2012) The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 12(4):252–264
Spear TT, Nagato K, Nishimura MI (2016) Strategies to genetically engineer T cells for cancer immunotherapy. Cancer Immunol Immunother 65(6):631–649
Babjuk M, Burger M, Zigeuner R, Shariat SF, van Rhijn BW, Compérat E, Sylvester RJ, Kaasinen E, Böhle A, Palou Redorta J, Rouprêt M, European Association of Urology (2013) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2013. Eur Urol 64(4):639–653
Morales A, Eidinger D, Bruce AW (1976) Intracavitary Bacillus Calmette-Guerin in the treatment of superficial bladder tumors. J Urol 116(2):180–183
Zhao W, Schorey JS, Bong-Mastek M, Ritchey J, Brown EJ, Ratliff TL (2000) Role of a bacillus Calmette-Guérin fibronectin attachment protein in BCG-induced antitumor activity. Int J Cancer 86(1):83–88
Suttmann H, Jacobsen M, Reiss K, Jocham D, Böhle A, Brandau S (2004) Mechanisms of bacillus Calmette-Guerin mediated natural killer cell activation. J Urol 172(4 Pt 1):1490–1495
Münz C, Steinman RM, Fujii S (2005) Dendritic cell maturation by innate lymphocytes: coordinated stimulation of innate and adaptive immunity. J Exp Med 202(2):203–207
Brandau S, Böhle A (2001) Activation of natural killer cells by Bacillus Calmette-Guérin. Eur Urol 39(5):518–524
Brandau S, Riemensberger J, Jacobsen M, Kemp D, Zhao W, Zhao X, Jocham D, Ratliff TL, Böhle A (2001) NK cells are essential for effective BCG immunotherapy. Int J Cancer 92(5):697–702
Taniguchi K, Koga S, Nishikido M, Yamashita S, Sakuragi T, Kanetake H, Saito Y (1999) Systemic immune response after intravesical instillation of bacille Calmette-Guérin (BCG) for superficial bladder cancer. Clin Exp Immunol 115(1):131–135
Jackson AM, Alexandroff AB, Kelly RW, Skibinska A, Esuvaranathan K, Prescott S, Chisholm GD, James K (1995) Changes in urinary cytokines and soluble intercellular adhesion molecule-1 (ICAM-1) in bladder cancer patients after bacillus Calmette-Guérin (BCG) immunotherapy. Clin Exp Immunol 99(3):369–375
Kamat AM, Briggman J, Urbauer DL, Svatek R, Nogueras González GM, Anderson R, Grossman HB, Prat F, Dinney CP (2016) Cytokine Panel for Response to Intravesical Therapy (CyPRIT): nomogram of changes in urinary cytokine levels predicts patient response to Bacillus Calmette-Guérin. Eur Urol 69(2):197–200
Atkins H, Davies BR, Kirby JA, Kelly JD (2003) Polarisation of a T-helper cell immune response by activation of dendritic cells with CpG-containing oligonucleotides: a potential therapeutic regime for bladder cancer immunotherapy. Br J Cancer 89(12):2312–2319
Saint F, Patard JJ, Groux Muscatelli B, Lefrere Belda MA, Diez Gil, de Medina S, Abbou CC, Chopin DK (2001) Evaluation of cellular tumour rejection mechanisms in the peritumoral bladder wall after bacillus Calmette-Guérin treatment. BJU Int 88(6):602–610
Riemensberger J, Böhle A, Brandau S (2002) IFN-gamma and IL-12 but not IL-10 are required for local tumour surveillance in a syngeneic model of orthotopic bladder cancer. Clin Exp Immunol 127(1):20–26
Tham SM, Ng KH, Pook SH, Esuvaranathan K, Mahendran R (2011) Tumor and microenvironment modification during progression of murine orthotopic bladder cancer. Clin Dev Immunol 2011:865684
Loskog A, Dzojic H, Vikman S, Ninalga C, Essand M, Korsgren O, Totterman TH (2004) Adenovirus CD40 ligand gene therapy counteracts immune escape mechanisms in the tumor Microenvironment. J Immunol 172(11):7200–7205
O’Donnell MA, Luo Y, Chen X, Szilvasi A, Hunter SE, Clinton SK (1999) Role of IL-12 in the induction and potentiation of IFN-gamma in response to bacillus Calmette-Guérin. J Immunol 163(8):4246–4252
Chen X, O`Donnell MA, Luo Y (2007) Dose-dependent synergy of Th1-stimulating cytokines on bacille Calmette-Guérin-induced interferon-gamma production by human mononuclear cells. Clin Exp Immunol 149(1):178–185
Watanabe E, Matsuyama H, Matsuda K, Ohmi C, Tei Y, Yoshihiro S, Ohmoto Y, Naito K (2003) Urinary interleukin-2 may predict clinical outcome of intravesical bacillus Calmette-Guérin immunotherapy for carcinoma in situ of the bladder. Cancer Immunol Immunother 52(8):481–486
Saint F, Kurth N, Maille P, Vordos D, Hoznek A, Soyeux P, Patard JJ, Abbou CC, Chopin DK (2003) Urinary IL-2 assay for monitoring intravesical bacillus Calmette-Guérin response of superficial bladder cancer during induction course and maintenance therapy. Int J Cancer 107(3):434–440
Werner-Felmayer G, Werner ER, Fuchs D, Hausen A, Reibnegger G, Wachter H (1990) Neopterin formation and tryptophan degradation by a human myelomonocytic cell line (THP-1) upon cytokine treatment. Cancer Res 50(10):2863–2867
Wirleitner B, Reider D, Ebner S, Böck G, Widner B, Jaeger M, Schennach H, Romani N, Fuchs D (2002) Monocyte-derived dendritic cells release neopterin. J Leukoc Biol 72(6):1148–1153
Mack D, Gomahr A, Herold M, Frick J (1995) Neopterin as a monitoring parameter for treatment with BCG in superficial bladder cancer. Eur J Cancer 31A(6):1025–1026
Pagès F, Lebel-Binay S, Vieillefond A, Deneux L, Cambillau M, Soubrane O, Debré B, Tardy D, Lemonne JL, Abastado JP, Fridman WH, Thiounn N (2002) Local immunostimulation induced by intravesical administration of autologous interferon-gamma-activated macrophages in patients with superficial bladder cancer. Clin Exp Immunol 127(2):303–309
Amsen D, Spilianakis CG, Flavell RA (2009) How are T(H)1 and T(H)2 effector cells made? Curr Opin Immunol 21(2):153–160. doi:10.1016/j.coi.2009.03.010
Hoyler T, Connor CA, Kiss EA, Diefenbach A (2013) T-bet and Gata3 in controlling type 1 and type 2 immunity mediated by innate lymphoid cells. Curr Opin Immunol 25(2):139–147. doi:10.1016/j.coi.2013.02.007
Kanhere A, Hertweck A, Bhatia U, Gökmen MR, Perucha E, Jackson I, Lord GM, Jenner RG (2012) T-bet and GATA3 orchestrate Th1 and Th2 differentiation through lineage-specific targeting of distal regulatory elements. Nat Commun 3:1268
Pichler R, Fritz J, Zavadil C, Schäfer G, Culig Z, Brunner A (2016) Tumor-infiltrating immune cell subpopulations influence the oncologic outcome after intravesical Bacillus Calmette-Guérin therapy in bladder cancer. Oncotarget 7(26):39916–39930. doi:10.18632/oncotarget.9537
Widner B, Werner ER, Schennach H, Wachter H, Fuchs D (1997) Simultaneous measurement of serum tryptophan and kynurenine by HPLC. Clin Chem 43(12):2424–2426
Geisler S, Mayersbach P, Becker K, Schennach H, Fuchs D, Gostner JM (2015) Serum tryptophan, kynurenine, phenylalanine, tyrosine and neopterin concentrations in 100 healthy blood donors. Pteridines 26(1):31–36. doi:10.1515/pterid-2014-0015
Fergusson JR, Smith KE, Fleming VM, Rajoriya N, Newell EW, Simmons R, Marchi E, Björkander S, Kang YH, Swadling L, Kurioka A, Sahgal N, Lockstone H, Baban D, Freeman GJ, Sverremark-Ekström E, Davis MM, Davenport MP, Venturi V, Ussher JE, Willberg CB, Klenerman P (2014) CD161 defines a transcriptional and functional phenotype across distinct human T cell lineages. Cell Rep 9(3):1075–1088
Gruenbacher G, Gander H, Rahm A, Idzko M, Nussbaumer O, Thurnher M (2016) Ecto-ATPase CD39 inactivates isoprenoid-derived Vγ9 Vδ2 T cell phosphoantigens. Cell Rep 16(2):444–456. doi:10.1016/j.celrep.2016.06.009
Dwyer KM, Hanidziar D, Putheti P, Hill PA, Pommey S, McRae JL, Winterhalter A, Doherty G, Deaglio S, Koulmanda M, Gao W, Robson SC, Strom TB (2010) Expression of CD39 by human peripheral blood CD4 + CD25 + T cells denotes a regulatory memory phenotype. Am J Transpl 10(11):2410–2420
Skillings JH, Mack GA (1981) On the use of a Friedman-type statistic in balanced and unbalanced block designs. Technometrics 23(2):171–177
Sylvester RJ, van der Meijden AP, Oosterlinck W, Witjes JA, Bouffioux C, Denis L, Newling DW, Kurth K (2006) Predicting recurrence and progression in individual patients with stage Ta, T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49(3):466–477
Weiss G, Murr C, Zoller H, Haun M, Widner B, Ludescher C, Fuchs D (1999) Modulation of neopterin formation and tryptophan degradation by Th1- and Th2-derived cytokines in human monocytic cells. Clin Exp Immunol 116:435–440
Agarwal A, Verma S, Burra U, Murthy NS, Mohanty NK, Saxena S (2006) Flow cytometric analysis of Th1 and Th2 cytokines in PBMCs as a parameter of immunological dysfunction in patients of superficial transitional cell carcinoma of bladder. Cancer Immunol Immunother 55(6):734–743
Bhattacharya D, Dwivedi VP, Kumar S, Reddy MC, Van Kaer L, Moodley P, Das G (2014) Simultaneous inhibition of T helper 2 and T regulatory cell differentiation by small molecules enhances Bacillus Calmette-Guerin vaccine efficacy against tuberculosis. J Biol Chem 289(48):33404–33411
Zhou M, Ouyang W (2003) The function role of GATA-3 in Th1 and Th2 differentiation. Immunol Res 28(1):25–37
Hwang ES, Szabo SJ, Schwartzberg PL, Glimcher LH (2005) T helper cell fate specified by kinase-mediated interaction of T-bet with GATA-3. Science 307(5708):430–433
Renkema KR, Lee JY, Lee YJ, Hamilton SE, Hogquist KA, Jameson SC (2016) IL-4 sensitivity shapes the peripheral CD8 + T cell pool and response to infection. J Exp Med 213(7):1319–1329. doi:10.1084/jem.20151359 Epub 2016 Jun 13
Carvalho LH, Sano G, Hafalla JC, Morrot A, Curotto de Lafaille MA, Zavala F (2002) IL-4-secreting CD4 + T cells are crucial to the development of CD8 + T-cell responses against malaria liver stages. Nat Med 8(2):166–170
De Monte L, Reni M, Tassi E, Clavenna D, Papa I, Recalde H, Braga M, Di Carlo V, Doglioni C, Protti MP (2011) Intratumor T helper type 2 cell infiltrate correlates with cancer-associated fibroblast thymic stromal lymphopoietin production and reduced survival in pancreatic cancer. J Exp Med 208(3):469–478
Carvalho MI, Pires I, Prada J, Queiroga FL (2014) A role for T-lymphocytes in human breast cancer and in canine mammary tumors. Biomed Res Int. doi:10.1155/2014/130894
Feng Q, Wei H, Morihara J, Stern J, Yu M, Kiviat N, Hellstrom I, Hellstrom KE (2012) Th2 type inflammation promotes the gradual progression of HPV-infected cervical cells to cervical carcinoma. Gynecol Oncol 127(2):412–419
Okita Y, Ohira M, Tanaka H, Tokumoto M, Go Y, Sakurai K, Toyokawa T, Kubo N, Muguruma K, Sawada T, Maeda K, Hirakawa K (2015) Alteration of CD4 T cell subsets in metastatic lymph nodes of human gastric cancer. Oncol Rep 34(2):639–647
Nunez-Nateras R, Castle EP, Protheroe CA, Stanton ML, Ocal TI, Ferrigni EN, Ochkur SI, Jacobsen EA, Hou YX, Andrews PE, Colby TV, Lee NA, Lee JJ (2014) Predicting response to bacillus Calmette-Guérin (BCG) in patients with carcinoma in situ of the bladder. Urol Oncol 32(1):45.e23–45.e30. doi:10.1016/j.urolonc.2013.06.008
Bahria-Sediki IB, Yousfi N, Paul C, Chebil M, Cherif M, Zermani R, El Gaaied AB, Bettaieb A (2016) Clinical significance of T-bet, GATA-3, and Bcl-6 transcription factor expression in bladder carcinoma. J Transl Med 14(1):144
Falkensammer C, Jöhrer K, Gander H, Ramoner R, Putz T, Rahm A, Greil R, Bartsch G, Thurnher M (2006) IL-4 inhibits the TNF-alpha induced proliferation of renal cell carcinoma (RCC) and cooperates with TNF-alpha to induce apoptotic and cytokine responses by RCC: implications for antitumor immune responses. Cancer Immunol Immunother 55(10):1228–1237
Mohammed KH, Siddiqui MT, Cohen C (2016) GATA3 immunohistochemical expression in invasive urothelial carcinoma. Urol Oncol 34(10):432.e9-432.e13. doi:10.1016/j.urolonc.2016.04.016
Li Y, Ishiguro H, Kawahara T, Kashiwagi E, Izumi K, Miyamoto H (2014) Loss of GATA3 in bladder cancer promotes cell migration and invasion. Cancer Biol Ther 15(4):428–435. doi:10.4161/cbt.27631
Miyamoto H, Izumi K, Yao JL, Li Y, Yang Q, McMahon LA, Gonzalez-Roibon N, Hicks DG, Tacha D, Netto GJ (2012) GATA binding protein 3 is down-regulated in bladder cancer yet strong expression is an independent predictor of poor prognosis in invasive tumor. Hum Pathol 43(11):2033–2040
Miyamoto H, Yao JL, Chaux A, Zheng Y, Hsu I, Izumi K, Chang C, Messing EM, Netto GJ, Yeh S (2012) Expression of androgen and oestrogen receptors and its prognostic significance in urothelial neoplasm of the urinary bladder. BJU Int 109(11):1716–1726
Miyamoto H, Zheng Y, Izumi K (2012) Nuclear hormone receptor signals as new therapeutic targets for urothelial carcinoma. Curr Cancer Drug Targets 12(1):14–22
Thurnher M, Ramoner R, Gastl G, Radmayr C, Böck G, Herold M, Klocker H, Bartsch G (1997) Bacillus Calmette-Guérin mycobacteria stimulate human blood dendritic cells. Int J Cancer 70(1):128–134
Ponticiello A, Perna F, Maione S, Stradolini M, Testa G, Terrazzano G, Ruggiero G, Malerba M, Sanduzzi A (2004) Analysis of local T lymphocyte subsets upon stimulation with intravesical BCG: a model to study tuberculosis immunity. Respir Med 98(6):509–514
de Boer EC, Rooyakkers SJ, Schamhart DH, de Reijke TM, Kurth KH (2005) BCG dose reduction by decreasing the instillation frequency: effects on local Th1/Th2 cytokine responses in a mouse model. Eur Urol 48(2):333–338
Biot C, Rentsch CA, Gsponer JR, Birkhäuser FD, Jusforgues-Saklani H, Lemaître F, Auriau C, Bachmann A, Bousso P, Demangel C, Peduto L, Thalmann GN, Albert ML (2012) Preexisting BCG-specific T cells improve intravesical immunotherapy for bladder cancer. Sci Transl Med 4(137):137ra72
Agarwal A, Agrawal U, Verma S, Mohanty NK, Saxena S (2010) Serum Th1 and Th2 cytokine balance in patients of superficial transitional cell carcinoma of bladder pre- and post-intravesical combination immunotherapy. Immunopharmacol Immunotoxicol 32(2):348–356
Lee YJ, Holzapfel KL, Zhu J, Jameson SC, Hogquist KA (2013) Steady-state production of IL-4 modulates immunity in mouse strains and is determined by lineage diversity of iNKT cells. Nat Immunol 14(11):1146–1154
Schüler T, Kammertoens T, Preiss S, Debs P, Noben-Trauth N, Blankenstein T (2001) Generation of tumor-associated cytotoxic T lymphocytes requires interleukin 4 from CD8(+) T cells. J Exp Med 194(12):1767–1775
Schüler T, Qin Z, Ibe S, Noben-Trauth N, Blankenstein T (1999) T helper cell type 1-associated and cytotoxic T lymphocyte-mediated tumor immunity is impaired in interleukin 4-deficient mice. J Exp Med 189(5):803–810
Tatsumi T, Kierstead LS, Ranieri E, Gesualdo L, Schena FP, Finke JH, Bukowski RM, Mueller-Berghaus J, Kirkwood JM, Kwok WW, Storkus WJ (2002) Disease-associated bias in T helper type 1 (Th1)/Th2 CD4(+) T cell responses against MAGE-6 in HLA-DRB10401(+) patients with renal cell carcinoma or melanoma. J Exp Med 196(5):619–628
Sucher R, Schroecksnadel K, Weiss G, Margreiter R, Fuchs D, Brandacher G (2010) Neopterin, a prognostic marker in human malignancies. Cancer Lett 287(1):13–22
Yan Y, Zhang GX, Gran B, Fallarino F, Yu S, Li H, Cullimore ML, Rostami A, Xu H (2010) IDO upregulates regulatory T cells via tryptophan catabolite and suppresses encephalitogenic T cell responses in experimental autoimmune encephalomyelitis. J Immunol 185:5953–5961
Curran TA, Jalili RB, Farrokhi A, Ghahary A (2014) IDO expressing fibroblasts promote the expansion of antigen specific regulatory T cells. Immunobiology 219(1):17–24
Mansour I, Zayed RA, Said F, Latif LA (2016) Indoleamine 2,3-dioxygenase and regulatory T cells in acute myeloid leukemia. Hematology 21(8):447–453. doi:10.1080/10245332.2015.1106814
Acknowledgements
Open access funding provided by University of Innsbruck and Medical University of Innsbruck. This work was supported by a personal research grant to Renate Pichler by the Medical Research Foundation Tyrol (MFF Tirol, Project Number 256).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no competing financial interests to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Pichler, R., Gruenbacher, G., Culig, Z. et al. Intratumoral Th2 predisposition combines with an increased Th1 functional phenotype in clinical response to intravesical BCG in bladder cancer. Cancer Immunol Immunother 66, 427–440 (2017). https://doi.org/10.1007/s00262-016-1945-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-016-1945-z