Abstract
A phase I/II study was conducted to test the feasibility and safety of the adoptive transfer of tumor-reactive T cells and daily injections of interferon-alpha (IFNα) in metastatic melanoma patients with progressive disease. Autologous melanoma cell lines were established to generate tumor-specific T cells by autologous mixed lymphocyte tumor cell cultures using peripheral blood lymphocytes. Ten patients were treated with on average 259 (range 38–474) million T cells per infusion to a maximum of six infusions, and clinical response was evaluated according to the response evaluation criteria in solid tumors (RECIST). Five patients showed clinical benefit from this treatment, including one complete regression, one partial response, and three patients with stable disease. No treatment-related serious adverse events were observed, except for the appearance of necrotic-like fingertips in one patient. An IFNα-related transient leucopenia was detected in 6 patients, including all responders. One responding patient displayed vitiligo. The infused T-cell batches consisted of tumor-reactive polyclonal CD8+ and/or CD4+ T cells. Clinical reactivity correlated with the functional properties of the infused tumor-specific T cells, including their in vitro expansion rate and the secretion of mainly Th1 cytokines as opposed to Th2 cytokines. Our study shows that relatively low doses of T cells and low-dose IFNα can lead to successful treatment of metastatic melanoma and reveals a number of parameters potentially associated with this success.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Melanoma has long been acknowledged to be a susceptible target for immunotherapy. A high number of melanomas are infiltrated by T cells, and the strength, phenotype, and activation status of infiltrated cells are associated with survival [1].
Adoptive cell transfer (ACT), i.e., the infusion of ex vivo expanded tumor-specific T cells, resulted in objective tumor responses in melanoma patients [2]. Previous ACT trials have demonstrated that clinical success required lymphodepletion prior to T-cell infusion and concomitant administration of high-dose interleukin-2 (IL-2) to maintain cell proliferation and activation status [3].
In allogeneic stem cell transplantation, interferon-alpha (IFNα) is routinely used to replace the far more toxic IL-2 to sustain the activation status of infused donor cells [4]. In addition, IFNα displays the capacity to upregulate HLA class I expression on tumor cells [5]. These molecules are critical for tumor cell recognition by T cells and often (partially) downregulated in melanoma [6]. Furthermore, IFNα is described to drive DC maturation required for generation of tumor-specific effector- and central-memory CD8+ T cells [7, 8].
Therefore, we studied the feasibility and potential of ACT in combination with IFNα for the treatment of metastatic melanoma. Tumor-reactive T cells were obtained from PBMC, as highly effective melanoma reactive CTL are readily induced from PBMC [9, 10] following stimulation with autologous tumor cells established from tumor biopsies.
Patients and methods
Melanoma patients
Patients with histologically proven cutaneous melanoma with verified progressive metastatic disease stage IV or unresectable stage III refractory to treatment before the start of the study and with at least one measurable target lesion were eligible for this phase I/II study. The protocol was approved by the Medical Ethics Committee of the Leiden University Medical Center and conducted in accordance with the Declaration of Helsinki. All patients gave written informed consent. Patients with brain metastases who are neurologically unstable and/or require use of dexamethasone and patients who are on continued chemo- or radiotherapy until 4 weeks before the start of IFNα injections were excluded from the study. The primary objective of this study was to investigate the feasibility and safety of adoptive T-cell transfer in combination with IFNα. Secondary endpoints include the best overall response defined as disease control (CR, PR, and SD) and evaluation of immunological parameters as predictors for response.
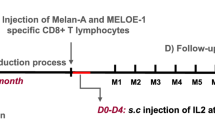
Treatment protocol
Patients received T cells as three consecutive infusions of on average 259 (range 38–474) million cells with a 3-week interval in combination with low-dose IFNα (3 million IU Roferon, Roche, Woerden, The Netherlands, subcutaneously daily) starting at day 7 before the first T-cell infusion and for a total of 12 weeks. Cryopreserved T cells were thawed and diluted to a total volume of 300 ml in PBS/2% human serum albumin (Albuman, Sanquin, Amsterdam, the Netherlands) and a final concentration of less than 1% DMSO. Then, the cells were administered intravenously over a time period of 30–60 min. At various time points before, during and after treatment, the tumor response was assessed by physical examination and tumor imaging (CT and MRI) and evaluated according to the Response Evaluation Criteria in Solid Tumors 1.0 (RECIST) [11] and according to the immune-related response criteria (irRC) [12]. Toxicity was scored using the CTC scale version 3.0.
Establishment of GMP-grade primary melanoma lines
Autologous melanoma cell lines were initiated and cultured using authorized Standard Operating Procedures (SOPs). Tumor tissue obtained by surgery was directly processed by mechanical dissociation and cultured in tumor medium consisting of Dulbecco’s MEM (DMEM, Lonza, Veriers, Belgium) supplemented with 8% irradiated, heat-inactivated GMP-grade pre-tested FCS, penicillin (50 U/ml), streptomycin (50 μg/ml), and l-glutamine (4 mM) (all from Lonza). A stable cell line could be established (usually within 4–12 weeks) for approximately 50% of the patients that was subsequently used as a stimulator line for the generation of tumor-reactive T-cell cultures. Before the initiation of T-cell cultures, the melanoma origin of the used autologous tumor cells was confirmed by RT–PCR [13–20] and they were shown to express at least three of the eleven melanoma-associated antigens studied (data not shown).
Furthermore, genotyping of HLA alleles was performed in all melanoma cell lines and corresponding PBMC to confirm their origin and revealed in addition that none of the used melanoma cell lines showed complete or partial genetic loss of HLA alleles. In addition, the surface expression of HLA class I and class II molecules was assessed by flow cytometry using Alexa-648-conjugated W6/32 HLA class I A/B/C (Serotec, Dusseldorf, Germany) and FITC-conjugated Bu26 HLA-DR/DP/DQ-specific antibodies (Bio-connect, Huissen, the Netherlands). The samples were measured on a FACSCalibur and analyzed using CellQuest Software and showed that HLA class I surface expression was not downregulated on the cell lines used for the induction of T cells and that all IFNγ-stimulated melanoma cells, except Mel AB and Mel CT, displayed variable surface expression of HLA class II (data not shown).
Generation and release of T-cell batches for infusion
Tumor-reactive T cells were cultured using a mixed lymphocyte tumor cell culture (MLTC) as described [21]. Briefly, PBMC were isolated from heparinized venous blood and cryopreserved until use. Approximately 50 million PBMC were thawed, washed, counted and resuspended (1–2 × 10e6 cells per ml) in T-cell medium; Iscoves MDM (Lonza) supplemented with 8% heat-inactivated pooled human serum (Sanquin Bloodbank, Dordrecht, The Netherlands), penicillin (50 U/ml), streptomycin (50 μg/ml), and l-glutamine (4 mM) (all GMP-grade from Lonza) and plated 1 ml per well in a 24-well culture plate. Next, autologous tumor cells were lethally irradiated (100 Gy) and resuspended (1 × 10e5 cells per ml) in T-cell medium. One milliliter of this tumor cell suspension was added per well containing PBMC. Human recombinant IL-4 (5 ng/ml, Cellgenix, Sieversen, Germany and Gentaur, Brussels Belgium) was added at day 0. Starting from day 2, low-dose (150 IU/ml) IL-2 (Aldesleukin, Novartis, Arnhem, The Netherlands) was added. Culture medium containing IL-2 was refreshed every 2–3 days. The T cells were cultured for a total of 4 weeks and stimulated weekly with irradiated tumor cells as described above. After 4 weeks of culture, the T-cell batches were evaluated for sterility, phenotype, and tumor reactivity before they were released for infusion. Phenotypic analysis was performed using a FACSCalibur and CellQuest software (BD Pharmingen, San Jose, CA, USA). T cells were released when they consist of more than 80% of T cells (CD3+CD4+ and CD3+CD8+) or NK cells (CD3-CD56+) (All conjugated-mAb were from BD Pharmingen except CD8-APC from DAKO, Heverlee, Belgium). In addition, the frequency of Treg CD4+CD25+FoxP3+ T cells was evaluated in the T-cell batches using CD4-APC and CD25-FITC mAb (both from BD Pharmingen) in combination with the human Treg/FoxP3-PE staining kit (eBiosciences, Vienna, Austria). Tumor reactivity was assessed by a 51Cr-cytotoxicity assay [22], and in order to be released for infusion, T cells were required to specifically lyse autologous tumor cells but not autologous EBV-LCL or PHA blasts (difference >10% at an E/T ratio of 30). Alternatively, tumor reactivity was assessed by IFNγ ELISA (Sanquin, Amsterdam, The Netherlands) where T-cell batches were required to secrete >200 pg/ml IFNγ in response to autologous tumor cells and at least twice the amount induced by the negative controls, i.e., autologous EBV-LCL or PHA blasts [23].
Analysis of T-cell specificity, polyclonality, and cytokine secretion by multiparameter flow cytometry
To examine T-cell reactivity, 0.5–1 × 10e6 T cells were seeded in a 24-well plate in T-cell medium and stimulated with 0.5–1 × 10e6 autologous melanoma cells. After 1 h, Brefeldin-A (10 μg/ml) was added and stimulation was continued overnight. The next day T cells were harvested, and part of the cells were stained with a mix of antibodies to CD154-PECy5, CD137-APC, CD4-PECy7, CD8-APCCy7, IFNγ-FITC, and IL-2-PE (all from BD Pharmingen) and CD3-Pacific Blue (DAKO) see [24]. Non-stimulated T cells or T cells stimulated with PHA (5 μg/ml) served as controls. Responses were considered positive when the percentage of tumor-stimulated CD154+ and/or CD137+ T cells was at least three times the medium control (see Fig 1. of the on-line available supplementary materials).
Polyclonality of the T-cell batches was evaluated by the anti-IFNγ-FITC and IL-2-PE Ab by either one of the 8 different mixes of FITC- and/or PE-conjugated anti-TCRVβ mAb (BETAmark, Beckman Coulter) as previously described [25]. The different T-cell clones were operationally defined as the percentage of activated tumor-specific CD4+ or CD8+ T cells expressing the same TCRVβ-chain, within the population of tumor-specifically activated CD154+ and/or CD137+ T cells, respectively. All samples were measured on a calibrated LSRII and analyzed using DIVA software (BD). A TCRVβ was considered dominant (>10%), subdominant (3–10%), or minor (<3%) based on the percentage of tumor-specific cells using the same TCRVβ [25].
In parallel, T cells were stimulated with autologous melanoma cell lines in the absence of Brefeldin-A, and supernatant was harvested after 24 h in order to analyze the cytokine secretion using the human Th1/Th2 cytometric bead array (BD Pharmingen). T cells stimulated with PHA (5 μg/ml), medium alone, and autologous EBV-LCL or PHA blasts were included as controls. Antigen-specific cytokine production was defined by a cytokine concentration above the cut-off value (IFNγ 50 pg/ml; other cytokines 10 pg/ml) and >2 × the concentration of the medium control [26].
Statistics
The overall survival was analyzed using Kaplan–Meier and SPSS version 2.0. The Cox regression could not performed due to the low patient number, and therefore no confidence interval and hazard ratio could be provided. Post hoc statistical analyses were performed to determine potential correlates with clinical responsiveness using the non-parametric Mann–Whitney Test or Wilcoxon Signed Ranks Test. All p values are two-sided and are considered significant when they are less than 0.05.
Results
Patient characteristics
Ten patients with metastatic melanoma were treated with adoptive transfer of tumor-reactive T cells (ACT) in combination with low-dose IFNα. Two additional patients were not treated although we obtained tumor-specific T cells, because they continued using chemotherapy or required dexamethasone to control brain metastasis-related edema, respectively, and therefore had to be taken of study. The characteristics of the ten treated patients are shown in Table 1. All patients had stage IV melanoma with visceral metastases, including liver, spleen, soft tissue, or bone metastases, in addition to metastasis in lymph nodes, lungs, or skin. Prior to ACT, all but one patient (GM) were treated with radiotherapy and/or chemotherapy (Table 1) and had progressive disease (PD) refractory to treatment. Seven out of ten patients had brain metastasis (Table 1). Patients FB and GM had high levels of serum LDH (>2 × upper normal limit (UNL)) correlating with a bad prognosis and high tumor load before the start of T-cell infusions, and patient CT had elevated LDH (i.e., >UNL but <2 × UNL). Eight patients completed at least one infusion cycle.
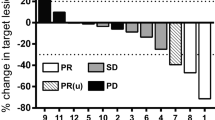
Clinical response
An objective clinical response was observed in two out of ten patients according to irRC and RECIST, and in three additional patients, clinical benefit was manifested as SD. One patient (BO) exhibits an ongoing complete response with duration of more than 45 months that was established after two cycles of ACT (Fig. 1a). Notably, this patient had an incompletely resected brain metastasis that completely disappeared after treatment. A second patient (DK) displayed an ongoing PR with complete regression of all but one mesenterial lesion, including a brain lesion, 4 skin lesions, and 4 LN-lesions. Two patients (EN, see Fig. 1a, and CT) showed SD (durations of 3+ and 3 months, respectively) but the latter received only one infusion cycle since treatment had to be discontinued due to a SAE. One other patient (AB) showed SD with duration of 6 months when evaluated according to irRC, whereas the duration was 3 month according to RECIST. However, this patient progressed very slowly resulting in an unexpected long survival (Fig. 1b; Table 1). Non-responders were defined as patients with PD by evaluation of CT and MRI scans according to RECIST and irRC or by death due to PD.
Clinical response. a ACT-induced regression of metastatic lesions before (upper panels) and after (lower panels) T-cell infusions. CT scans showing complete regression of two lung lesions obtained 6 month after T-cell infusion in the CR patient BO are depicted in the left two panels. Regression of a subcutaneous lesion obtained 3 months after start of the infusions in patient EN is depicted in the right panel. b Kaplan–Meier plot comparing the overall survival of the responder and non-responder patients. c IFNα treatment induced a mild leucopenia. From day 7 before infusion of the first T-cell dose, patients were treated with 3.10e6 U IFNα s.c daily for a total of 12 weeks. The absolute leukocyte count (x10e9/L) measured 1 week after the start of IFNα injections (i.e., day 0) is depicted. The values measured before treatment are shown as a black arrowhead. Absolute leukocyte counts of the responder patients are depicted as filled bars and those of the non-responders as open bars. The best overall clinical response of the individual patients is given in brackets behind the patient ID. Normal leukocyte counts range between 4 and 12 as is indicated by the light gray area. d The percentage reduction in peripheral neutrophil counts obtained after 7 days of IFNα treatment (i.e., day 0) of the non-responder (open circles) and responder (closed circles) patients correlates with their overall survival
Adverse events
In half of the patients (5/10), fever (grade 1) was observed up to 20 h and one patient displayed transient hypertension (grade 1) after T-cell infusion. No other adverse symptoms were observed immediately after infusion.
Five out of ten patients suffered from grade 1 (n = 4) to grade 2 (n = 1) psychological symptoms associated with the administration of IFNα (Roferon), resulting in the reduction and/or discontinuation of the daily dose of IFNα given in patient CT, DK, and JS. One patient (EN) experienced numbness of fingers after 7 weeks of IFNα treatment. This disappeared after discontinuation of IFNα treatment and was previously described as a rare side effect of high-dose IFNα [27]. One patient (CT) developed acral vasculitis with necrotic-like lesions in her fingertips without inflammatory cell infiltrate or microorganisms. Also a folliculitis-like inflammation of the skin was seen after the first infusion of the second treatment cycle. Skin biopsies were taken, and since a role of T cells could not be completely ruled out, the therapy was discontinued. One responding patient (DK) experienced grade 1 vitiligo. All serious adverse events are listed in Table 1 of the on-line available supplementary materials.
Five out of ten patients showed grade 2 IFNα-induced leucopenia, and six patients had leukocyte counts below 4 × 10e9 c/l at the start of T-cell infusions (Fig. 1c). The leukocyte numbers usually remained reduced throughout the full period that IFNα was administered and returned to pretreatment values after cessation of IFNα injections. Importantly, the absolute leukocyte count dropped below the normal number of leukocytes (4 × 10e9/l) in all patients which showed a clinical response, whereas it remained within the normal range of leukocytes 4–12 × 10e9/L in 4 of the 5 non-responding patients (Fig. 1c) resulting in a significantly lower number of leukocytes in responder patients compared to non-responder patients (P = 0,016). Differential blood counts showed that especially neutrophil (42% reduction, range 0–89%) and to a lesser extend lymphocyte numbers (29% reduction, range 2–56%) were decreased after IFNα treatment and the percentage reduction of the neutrophil counts correlated with prolonged survival (P = 0.022; Fig. 1d). Neutrophil counts prior to IFNα treatment did not significantly differ between responder and non-responder patients (6.9 vs. 4.1 × 10e9/l, P = 0.15).
The tumor-reactive T cells in the group of clinical responders display a strong in vitro expansion rate
PBMC were stimulated 4 times with autologous tumor cells in vitro. The number of T cells obtained for each patient differed and ranged from 5.9 to 465 × 107, reflecting a 2.1–70-fold increase in cell number.
A comparison of the weekly expansion of T cells of the groups of responder and non-responder patients clearly revealed that tumor-stimulated PBMC of the clinical responders expanded faster than those of the non-responders, albeit not quite significant (P = 0.056; Fig. 2). Indeed many more MLTC’s were required to obtain sufficient numbers of cells to transfuse the non-clinical responders.
Proliferation of T cells during MLTC. T cells were produced by MLTC using autologous tumor cells as stimulator cells at day 0 and every week thereafter. The proliferation was assessed weekly after harvesting and counting of viable cell numbers using trypan blue. The proliferation rate is expressed as fold expansion of cells compared to cell number at day 0. The median and 25th percentile deviation of the weekly proliferation rate of responding (filled circle, n = 5) and non-responding (open circle, n = 5) patients are depicted
The differences in expansion were not associated with the level of HLA class I or II surface expression or the pattern of melanoma antigens expressed by the melanoma cells (data not shown).
Characteristics of infused T cells
All T-cell batches were shown to consist mainly of CD3+CD4+ and CD3+CD8+ T cells (Fig. 3) but the ratio of CD8+/CD4+ T cells varied considerably between patients. The majority of the T cells were CD45RA, CD62L, and CCR7 negative (effector memory T cells; data not shown). T-cell batches from patient DK, GM, HL, and JS showed expansion of CD3+CD4+ T cells (Fig. 3). T-cell batches from three of these patients (responder patient DK and non-responder patients HL and JS) contained a relatively high-frequency CD4+CD25+FoxP3+ T cells, respectively, 9, 6, and 23%, whereas all other batches contained a mean of only 2.6 ± 1.7% of CD4+CD25+FoxP3+ T cells (data not shown). Furthermore, while in all other patients, the percentage of CD3+CD8+CD56+ T cells was low (median 1%, range 0–8%), this was the main subset present in the T-cell batch of patient CT (not shown).
Activation of infused T cells. T-cell batches were stimulated with autologous tumor cells and stained for phenotypic and activation markers as described in the Methods section. The percentage CD4+ and CD8+ T cells are given in the squares on the left of each plot. The CD154+CD4+ and CD137+CD8+ T cells (gated on CD3+ cells) are plotted, and percentages of tumor-specific activated cells (i.e., at least three times the medium control, see Fig. 1 of the on-line available supplementary materials) are given in the plots. The best overall clinical response of the individual patients is given in brackets behind the patient ID
On average, the T-cell batches induced 19% specific tumor cell lysis in a 51Cr-cytotoxicity assay (at an effector to target ratio of 30 and after subtraction of autologous B-LCL/PHA-blasts lysis) and did not significantly differ between T cells administered to responding and non-responding patient (Fig. 4). T cells from patient DK and JS contained mainly CD3+CD4+ T cells and did not show specific lysis in a short-term cytotoxicity assay, but specifically released IFNγ upon stimulation with the patients’ tumor cells and not when stimulated with EBV-LCL or PHA blasts (data not shown).
Reactivity of infused T cells. The specific reactivity of the T-cell batches was analyzed by cytotoxicity assay. Effector T cells were added in increasing ratios to radioactively 51Cr-labeled target cells (E/T) and incubated for 4 h at 37°C. Specific lysis of target cells was calculated after measuring the 51Cr release as described [22]. The percentage-specific lysis of autologous melanoma cells (black bars) and corresponding PHA blasts or EBV-LCL control cells (white bars) at different E/T ratios is depicted. The patient ID of the different T-cell batches is given in the upper right corner of the corresponding graphs. Results for the responder and non-responder patients are shown in the left and right panels, respectively
Based on the tumor-induced expression of the T-cell activation markers CD154/CD137, the infused T-cell batches constituted a median of 27.6% (mean 29.3%, range 0–61.1%) tumor-specific T cells comprising a median of 2.5% (range 0–22.6) tumor-specific CD3+CD4+ T cells and 16.5% (range 0–57.3%) tumor-specific CD3+CD8+ T cells (Fig. 3). Comparison of the tumor reactivity between the T-cell batches revealed that there was no significant difference (P = 0.55) in frequencies of tumor-specific activated CD3+CD4+CD154+ or CD3+CD8+CD137+ T cells administered to responding or non-responding patients. Assessment of the polyclonality of the tumor-specific T-cell batches, operationally defined as the cohort of CD4+ or CD8+ T cells expressing the same TCRVβ-chain within the population of tumor-activated CD154+ and/or CD137+ T cells, revealed on average the involvement of 8 TCRVβ families (range 0–15) indicating that the infused tumor-specific T-cell population is highly polyclonal. No significant differences were observed in this respect between clinical responders and non-responders (Table 2).
The polyfunctionality of the tumor-specific T cells, defined by the percentage of cells secreting IFNγ and/or IL-2 within the fraction of tumor-specific T cells (see Fig. 2 of the supplementary materials available on-line), was not overtly different between the T-cell batches from the groups of clinically responding and non-responding patients. However, the cytokine profile produced by the infused T cells varied from predominantly Th1-type cytokines (IFNγ, IL-2 and TNFα) in four clinically responding patients to predominantly Th2 cytokines (IL-4, IL-5 and IL-10, patient IV and JS), a mix of Th1 and Th2 cytokines (patient HL) or no cytokines at all (patient FB and GM) in patients without a clinical response (Fig. 5). All together these data suggest that a predominant Th1 cytokine profile is beneficial for the clinical outcome.
Th1 and Th2 cytokine profile of T cells used for infusion. T cells were stimulated with autologous tumor cells overnight, and the supernatant was analyzed for the production of Th1 (IFNγ, IL-2 and TNFα) and Th2 (IL-10, 4 and 5) cytokines. The cytokine production after subtraction of background production after culture in medium alone is depicted for responder (black bars) and non-responder (white bars) patients, respectively. The best overall clinical response of the individual patients is given in brackets behind the patient ID. ND is not detectable
Discussion
The results of this phase I/II study clearly demonstrate that adoptive transfer of PBMC-derived tumor-specific T cells in combination with low-dose INFα is feasible and safe and can induce a disease control (CR, PR, and SD) in 50% of the treated patients displaying progressive metastatic melanoma before treatment without any major adverse events related to the infusion of T cells. Analyses of several different immune-related parameters, which are discussed in more detail below, resulted in a number of hypotheses that could explain clinical reactivity or the lack thereof. All together, these data warrant the conduct of a controlled clinical trial to confirm or reject our current observations.
All responding patients experienced an IFNα -induced mild and transient leucopenia including both reduced lymphocyte and in particular neutrophil numbers. Interestingly, high peripheral neutrophil numbers are described to be an independent prognostic factor for worse outcome of IL-2-based therapy in melanoma patients [28]. Here, we observe that the level of neutrophil reduction after IFNα-conditioning correlates with increased survival and that all clinically responding patients display a clear reduction in peripheral neutrophil numbers after IFNα treatment. Notably, there was no difference in neutrophil numbers between these groups before treatment that could explain a difference in survival. Since expansion of IL-10-secreting immunosuppressive neutrophils has recently been shown to correlate with disease progression in melanoma [29], the observed IFNα-mediated reduction in neutrophil numbers may have resulted in lower IL-10 levels but unfortunately this could not be tested in our current patient group because we did not obtain serum of all patients prior to therapy. A recent study in melanoma patients reported the reduction in regulatory T cells (Treg) following high-dose IFNα treatment [30]. Whether the leucopenia observed in our study after a much lower dose of IFNα treatment also reduces the frequency of Treg or creates space for infused T cells and/or induces homeostatic cytokines IL-7 and IL-15, as has been suggested as mechanism to explain the beneficial effect of other lymphodepleting-conditioning regimens [2], remains to be elucidated. Although IFNα is a pleiotropic cytokine and its use may contribute to the eventual clinical effect via a variety of pathways, a direct inhibitory effect of IFNα on the tumor is unlikely since single-agent IFNα treatment is only effective in much higher doses than the low dose used in our study, which was proven to be not effective in phase I/II studies [31, 32].
To unravel potential mechanisms underlying the clinical responsiveness of patients, we performed a detailed characterization of the infused T-cell batches and observed that the expansion rate of T cells during the production phase was higher for cells infused in patients with a clinical response. This cannot be attributed to a reduced frequency of tumor-specific T cells in the PBMC or lack of antigen expression on autologous cell lines used to obtain the T-cell batches, since tumor-specific polyclonal T-cell populations were obtained in all patients. Whether the reduced expansion rate of T cells infused to non-responding patients is due to expression and/or secretion of immunosuppressive factors by their autologous tumor cells is subject of our current investigations. Alternatively, the reduced proliferation in the non-responding patients may be due to an intrinsic lack of proliferative capacity of their PBMC. Indeed, the proliferative capacity of ex vivo expanded tumor-infiltrating lymphocytes has been associated with tumor regression and has been linked to telomere length in these T cells [33]. The reduced proliferation of T cells may also be due to the selective expansion of Treg, since at least in some cases (patient HL and JS), relatively high frequencies of CD4+CD25+FoxP3+ T cells were detected in the T-cell batches. Indeed, the accumulation of Treg in peripheral blood and locally in the tumor environment and metastatic lymph nodes of melanoma patients has previously been associated with impaired T-cell responsiveness [34] and as such supports this idea. However, functional studies are required to appreciate their suppressive role during the mixed tumor T-cell cultures in vitro.
The stimulation of patients’ PBMC with autologous tumor cells, expressing the full spectrum of relevant HLA molecules and tumor antigens, leads to expansion of polyclonal CD4+ as well as CD8+ T cells, which may contribute to the current success. Although a recent case report shows that treatment of a melanoma patient with clonal NY-ESO-1-specific CD4+ T cells can be successful [35], we aim at infusion of polyclonal T cells, thus preventing the appearance of antigen-loss variants frequently found after transfer of single-antigen-specific T cells [36, 37]. Since polyclonal tumor-reactive T cells are infused in all patients but the clinical response does not merely correlate to the percentage or ratio of specific CD8+ versus CD4+ T cells, we conclude that the presence of a broad repertoire of tumor-reactive T cells by itself is not sufficient to induce a clinical effect but relies on other factors including their functional activity. Our patient number is too small to reach significance, but our results are in line with previous observations [38–40], indicating that infusion of T cells that predominantly produce Th1 cytokines results in a better clinical outcome compared to infusion of T cells that produce mainly Th2 cytokines or no Th1/Th2 cytokines at all and that the presence of both tumor-specific Th1 cells and CTL mediates an effective anti-tumor response [41].
In summary, the adoptive transfer of polyclonal tumor-specific T cells obtained after stimulation of PBMC with autologous tumor cells in combination with low-dose IFNα can result in durable clinical responses in stage IV melanoma patients supporting the idea to explore IFNα as an alternative conditioning regimen and cytokine for ACT trials. Although the use of IFNα also comes with some side effects, including the beneficial leukopenia and controllable psychological symptoms, it is far less toxic than high-dose IL-2, commonly used to support transferred T cells. The clinical responses reported here are associated with IFNα-induced lympho- and neutropenia and the proliferative capacity as well as the Th1/Th2 cytokine profile of the T cells used for infusion, underscoring the importance of measuring parameters that are associated with clinical reactivity of the infused T-cell batches to fully appreciate their in vivo effectiveness. Eventual combination of this approach with other treatment options may even further enhance the clinical outcome. One possibility is the combined use of ACT/IFNα with ipilimumab or negative immunoregulatory human cell surface receptor PD-1 (programmed death-1). These immune activating antibodies may result in further in vivo expansion of tumor-specific T cells and improved clinical effect after ACT/IFNα.
References
Oble DA, Loewe R, Yu P, Mihm MC Jr (2009) Focus on TILs: prognostic significance of tumor infiltrating lymphocytes in human melanoma. Cancer Immun 9:3
Dudley ME, Yang JC, Sherry R, Hughes MS, Royal R, Kammula U, Robbins PF, Huang J, Citrin DE, Leitman SF, Wunderlich J, Restifo NP, Thomasian A, Downey SG, Smith FO, Klapper J, Morton K, Laurencot C, White DE, Rosenberg SA (2008) Adoptive cell therapy for patients with metastatic melanoma: evaluation of intensive myeloablative chemoradiation preparative regimens. J Clin Oncol 26:5233–5239
Dudley ME, Rosenberg SA (2007) Adoptive cell transfer therapy. Semin Oncol 34:524–531
Posthuma EF, Marijt EW, Barge RM, van Soest RA, Baas IO, Starrenburg CW, van Zelderen-Bhola SL, Fibbe WE, Smit WM, Willemze R, Falkenburg JH (2004) Alpha-interferon with very-low-dose donor lymphocyte infusion for hematologic or cytogenetic relapse of chronic myeloid leukemia induces rapid and durable complete remissions and is associated with acceptable graft-versus-host disease. Biol Blood Marrow Transplant 10:204–212
Cangemi G, Morandi B, D’Agostino A, Peri C, Conte R, Damonte G, Ferlazzo G, Biassoni R, Melioli G (2003) IFN-alpha mediates the up-regulation of HLA class I on melanoma cells without switching proteasome to immunoproteasome. Int Immunol 15:1415–1421
Mendez R, Aptsiauri N, Del CA, Maleno I, Cabrera T, Ruiz-Cabello F, Garrido F, Garcia-Lora A (2009) HLA and melanoma: multiple alterations in HLA class I and II expression in human melanoma cell lines from ESTDAB cell bank. Cancer Immunol Immunother 58:1507–1515
Gigante M, Blasi A, Loverre A, Mancini V, Battaglia M, Selvaggi FP, Maiorano E, Napoli A, Castellano G, Storkus WJ, Gesualdo L, Ranieri E (2009) Dysfunctional DC subsets in RCC patients: Ex vivo correction to yield an effective anti-cancer vaccine. Mol Immunol 46:893–901
Ramos HJ, Davis AM, Cole AG, Schatzle JD, Forman J, Farrar JD (2009) Reciprocal responsiveness to IL-12 and IFN-{alpha} specifies human CD8+ effector versus central memory T cell fates. Blood 113:5516–5525
Bouquie R, Bonnin A, Bernardeau K, Khammari A, Dreno B, Jotereau F, Labarriere N, Lang F (2009) A fast and efficient HLA multimer-based sorting procedure that induces little apoptosis to isolate clinical grade human tumor specific T lymphocytes. Cancer Immunol Immunother 58:553–566
Hinrichs CS, Spolski R, Paulos CM, Gattinoni L, Kerstann KW, Palmer DC, Klebanoff CA, Rosenberg SA, Leonard WJ, Restifo NP (2008) IL-2 and IL-21 confer opposing differentiation programs to CD8+ T cells for adoptive immunotherapy. Blood 111:5326–5333
Tsuchida Y, Therasse P (2001) Response evaluation criteria in solid tumors (RECIST): new guidelines. Med Pediatr Oncol 37:1–3
Wolchok JD, Hoos A, O’Day S, Weber JS, Hamid O, Lebbe C, Maio M, Binder M, Bohnsack O, Nichol G, Humphrey R, Hodi FS (2009) Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res 15:7412–7420
Brouwenstijn N, Slager EH, Bakker AB, Schreurs MW, van der Spek CW, Adema GJ, Schrier PI, Figdor CG (1997) Transcription of the gene encoding melanoma-associated antigen gp100 in tissues and cell lines other than those of the melanocytic lineage. Br J Cancer 76:1562–1566
Adema GJ, de Boer AJ, Vogel AM, Loenen WA, Figdor CG (1994) Molecular characterization of the melanocyte lineage-specific antigen gp100. J Biol Chem 269:20126–20133
Brasseur F, Marchand M, Vanwijck R, Herin M, Lethe B, Chomez P, Boon T (1992) Human gene MAGE-1, which codes for a tumor-rejection antigen, is expressed by some breast tumors [letter]. Int J Cancer 52:839–841
De Plaen E, Arden K, Traversari C, Gaforio JJ, Szikora JP, De SC, Brasseur F, van der Bruggen P, Lethe B, Lurquin C (1994) Structure, chromosomal localization, and expression of 12 genes of the MAGE family. Immunogenetics 40:360–369
Takase H, Yu CR, Mahdi RM, Douek DC, Dirusso GB, Midgley FM, Dogra R, Allende G, Rosenkranz E, Pugliese A, Egwuagu CE, Gery I (2005) Thymic expression of peripheral tissue antigens in humans: a remarkable variability among individuals. Int Immunol 17:1131–1140
Aarnoudse CA, van den Doel PB, Heemskerk B, Schrier PI (1999) Interleukin-2-induced, melanoma-specific T cells recognize CAMEL, an unexpected translation product of LAGE-1. Int J Cancer 82:442–448
Ikeda H, Lethe B, Lehmann F, van Baren N, Baurain JF, De Smet C, Chambost H, Vitale M, Moretta A, Boon T, Coulie PG (1997) Characterization of an antigen that is recognized on a melanoma showing partial HLA loss by CTL expressing an NK inhibitory receptor. Immunity 6:199–208
Godet Y, Moreau-Aubry A, Guilloux Y, Vignard V, Khammari A, Dreno B, Jotereau F, Labarriere N (2008) MELOE-1 is a new antigen overexpressed in melanomas and involved in adoptive T cell transfer efficiency. J Exp Med 205:2673–2682
Herin M, Lemoine C, Weynants P, Vessiere F, Van Pel A, Knuth A, Devos R, Boon T (1987) Production of stable cytolytic T-cell clones directed against autologous human melanoma. Int J Cancer 39:390–396
Verdegaal EME, Huinink DB, Hoogstraten C, Marijnissen AK, Gorsira MB, Claas FH, Osanto S (1999) Isolation of broadly reactive, tumor-specific, HLA Class-I restricted CTL from blood lymphocytes of a breast cancer patient. Hum Immunol 60:1195–1206
Besser MJ, Shapira-Frommer R, Treves AJ, Zippel D, Itzhaki O, Hershkovitz L, Levy D, Kubi A, Hovav E, Chermoshniuk N, Shalmon B, Hardan I, Catane R, Markel G, Apter S, Ben-Nun A, Kuchuk I, Shimoni A, Nagler A, Schachter J (2010) Clinical responses in a phase II study using adoptive transfer of short-term cultured tumor infiltration lymphocytes in metastatic melanoma patients. Clin Cancer Res 16:2646–2655
Speetjens FM, Kuppen PJ, Welters MJ, Essahsah F, Voet van den Brink AM, Lantrua MG, Valentijn AR, Oostendorp J, Fathers LM, Nijman HW, Drijfhout JW, van de Velde CJ, Melief CJ, van der Burg SH (2009) Induction of p53-specific immunity by a p53 synthetic long peptide vaccine in patients treated for metastatic colorectal cancer. Clin Cancer Res 15:1086–1095
de Vos-van Steenwijk PJ, Heusinkveld M, Ramwadhdoebé TH, Lowik MJ, van der Hulst JM, Goedemans R, Piersma SJ, Kenter GG, van der Burg SH (2010) An unexpectedly large polyclonal repertoire of HPV-specific T cells is poised for action in patients with cervical cancer. Cancer Res 70:2707–2717
de Jong A, van Poelgeest MI, van der Hulst JM, Drijfhout JW, Fleuren GJ, Melief CJ, Kenter G, Offringa R, van der Burg SH (2004) Human papillomavirus type 16-positive cervical cancer is associated with impaired CD4+ T-cell immunity against early antigens E2 and E6. Cancer Res 64:5449–5455
Taguchi T (1986) Clinical studies of recombinant interferon alfa-2a (Roferon-A) in cancer patients. Cancer 57:1705–1708
Schmidt H, Suciu S, Punt CJ, Gore M, Gore M, Kruit W, Patel P, Lienard D, von der MH, Eggermont AM, Keilholz U (2007) Pretreatment levels of peripheral neutrophils and leukocytes as independent predictors of overall survival in patients with American Joint Committee on cancer stage IV melanoma: results of the EORTC 18951 biochemotherapy trial. J Clin Oncol 25:1562–1569
De Santo C, Arscott R, Booth S, Karydis I, Jones M, Asher R, Salio M, Middleton M, Cerundolo V (2010) Invariant NKT cells modulate the suppressive activity of IL-10-secreting neutrophils differentiated with serum amyloid A. Nat Immunol 11:1039–1046
Ascierto PA, Napolitano M, Celentano E, Simeone E, Gentilcore G, Daponte A, Capone M, Caraco C, Calemma R, Beneduce G, Cerrone M, De Rosa V, Palmieri G, Castello G, Kirkwood JM, Marincola FM, Mozzillo N (2010) Regulatory T cell frequency in patients with melanoma with different disease stage and course, and modulating effects of high-dose interferon-alpha 2b treatment. J Transl Med 8:76–88
Lens MB, Dawes M (2002) Interferon alfa therapy for malignant melanoma: a systematic review of randomized controlled trials. J Clin Oncol 20:1818–1825
Agarwala SS, Kirkwood JM (1996) Interferons in melanoma. Curr Opin Oncol 8:167–174
Zhou J, Shen X, Huang J, Hodes RJ, Rosenberg SA, Robbins PF (2005) Telomere length of transferred lymphocytes correlates with in vivo persistence and tumor regression in melanoma patients receiving cell transfer therapy. J Immunol 175:7046–7052
Correll A, Tuettenberg A, Becker C, Jonuleit H (2010) Increased regulatory T-cell frequencies in patients with advanced melanoma correlate with a generally impaired T-cell responsiveness and are restored after dendritic cell-based vaccination. Exp Dermatol 19:e213–e221
Hunder NN, Wallen H, Cao J, Hendricks DW, Reilly JZ, Rodmyre R, Jungbluth A, Gnjatic S, Thompson JA, Yee C (2008) Treatment of metastatic melanoma with autologous CD4+ T cells against NY-ESO-1. N Eng J Med 358:2698–2703
Mackensen A, Meidenbauer N, Vogl S, Laumer M, Berger J, Andreesen R (2006) Phase I study of adoptive T-cell therapy using antigen-specific CD8+ T cells for the treatment of patients with metastatic melanoma. J Clin Oncol 24:5060–5069
Ribas A, Comin-Anduix B, Economou JS, Donahue TR, de la RP, Morris LF, Jalil J, Dissette VB, Shintaku IP, Glaspy JA, Gomez-Navarro J, Cochran AJ (2009) Intratumoral immune cell infiltrates, FoxP3, and indoleamine 2,3-dioxygenase in patients with melanoma undergoing CTLA4 blockade. Clin Cancer Res 15:390–399
Rosenberg SA, Dudley ME, Restifo NP (2008) Cancer immunotherapy. N Engl J Med 359:1072
Riddell SR, Greenberg PD (1995) Principles for adoptive T cell therapy of human viral diseases. Annu Rev Immunol 13:545–586
Hamilton D, Ismail N, Kroeger D, Rudulier C, Bretscher P (2009) Macroimmunology and immunotherapy of cancer. Immunotherapy 1:367–383
Ostrand-Rosenberg S (2005) CD4+ T lymphocytes: a critical component of antitumor immunity. Cancer Invest 23:413–419
Acknowledgments
The authors wish to thank Dr. Els Persijn-van Meerten for experienced evaluation of CT and MRI scans and Prof. Hein Putter for statistical evaluation of the data. We also want to thank Conny Hoogstraten, Hannah Wensink, Inonge van Twillert and Loes van Eijk for their technical assistance.
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Verdegaal, E.M.E., Visser, M., Ramwadhdoebé, T.H. et al. Successful treatment of metastatic melanoma by adoptive transfer of blood-derived polyclonal tumor-specific CD4+ and CD8+ T cells in combination with low-dose interferon-alpha. Cancer Immunol Immunother 60, 953–963 (2011). https://doi.org/10.1007/s00262-011-1004-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-011-1004-8