Abstract
Objective
Determine normal T1 and extracellular volume (ECV) of the pancreas in subjects with no pancreas disease and correlate with age and gender.
Subjects and methods
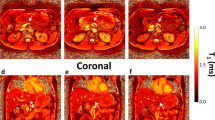
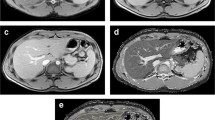
We imaged 120 healthy subjects (age range 20–78 years) who are on annual screening with MRI/MRCP for the possibility of pancreatic cancer. Subjects had a predisposition to develop pancreatic cancer, but no history of pancreas disease or acute symptoms. Equal number (n = 60) of subjects were scanned on either 1.5 T or 3 T scanner using dual flip angle spoiled gradient echo technique incorporating fat suppression and correction for B1 field inhomogeneity. Optimization of imaging parameters was performed using a T1 phantom. ECV was calculated using pre- and post-contrast T1 of the pancreas and plasma. Regression analysis and Mann–Whitney tests were used for statistical analysis.
Results
Median T1 on 1.5 T was 654 ms (IQR 608–700); median T1 on 3 T was 717 ms (IQR 582–850); median ECV on 1.5 T was 0.28 (IQR 0.21–0.33), and median ECV on 3 T was 0.25 (IQR 0.19–0.28). Age had a mild positive correlation with T1 (r = 0.24, p = 0.009), but not with ECV (r = 0.06, p = 0.54). T1 and ECV were similar in both genders (p > 0.05).
Conclusion
This study measured the median T1 and ECV of the pancreas in subjects with no pancreas disease. Pancreas shows longer T1 relaxation times in older population, whereas extracellular fraction remains unchanged. Median T1 values were different between two magnet strengths; however, no difference was seen between genders and ECV fractions.



Similar content being viewed by others
Abbreviations
- ECV:
-
Extracellular volume
- MRCP:
-
Magnetic resonance cholangiopancreatography
- MRI:
-
Magnetic resonance imaging
- 3D:
-
Three-dimensional
References
Rosenkrantz AB, Mendiratta-Lala M, Bartholmai BJ, Ganeshan D, Abramson RG, Burton KR, Yu JP, Scalzetti EM, Yankeelov TE, Subramaniam RM, Lenchik L (2015) Clinical utility of quantitative imaging. Acad Radiol 22 (1):33-49. https://doi.org/10.1016/j.acra.2014.08.011
Messroghli DR, Greiser A, Frohlich M, Dietz R, Schulz-Menger J (2007) Optimization and validation of a fully-integrated pulse sequence for modified look-locker inversion-recovery (MOLLI) T1 mapping of the heart. J Magn Reson Imaging 26 (4):1081-1086. https://doi.org/10.1002/jmri.21119
Moon JC, Messroghli DR, Kellman P, Piechnik SK, Robson MD, Ugander M, Gatehouse PD, Arai AE, Friedrich MG, Neubauer S, Schulz-Menger J, Schelbert EB, Society for Cardiovascular Magnetic Resonance I, Cardiovascular Magnetic Resonance Working Group of the European Society of C (2013) Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR Working Group of the European Society of Cardiology consensus statement. J Cardiovasc Magn Reson 15:92. https://doi.org/10.1186/1532-429x-15-92
Ou HY, Bonekamp S, Bonekamp D, Corona-Villalobos CP, Torbenson MS, Geiger B, Kamel IR (2013) MRI arterial enhancement fraction in hepatic fibrosis and cirrhosis. AJR Am J Roentgenol 201 (4):W596-602. https://doi.org/10.2214/ajr.12.10048
Tirkes T, Lin C, Cui E, Deng Y, Territo PR, Sandrasegaran K, Akisik F (2018) Quantitative MR Evaluation of Chronic Pancreatitis: Extracellular Volume Fraction and MR Relaxometry. AJR Am J Roentgenol 210 (3):533-542. https://doi.org/10.2214/ajr.17.18606
Kim KA, Park MS, Kim IS, Kiefer B, Chung WS, Kim MJ, Kim KW (2012) Quantitative evaluation of liver cirrhosis using T1 relaxation time with 3 tesla MRI before and after oxygen inhalation. J Magn Reson Imaging 36 (2):405-410. https://doi.org/10.1002/jmri.23620
Curtis WA, Fraum TJ, An H, Chen Y, Shetty AS, Fowler KJ (2019) Quantitative MRI of Diffuse Liver Disease: Current Applications and Future Directions. Radiology 290 (1):23-30. https://doi.org/10.1148/radiol.2018172765
Luetkens JA, Klein S, Traber F, Schmeel FC, Sprinkart AM, Kuetting DLR, Block W, Uschner FE, Schierwagen R, Hittatiya K, Kristiansen G, Gieseke J, Schild HH, Trebicka J, Kukuk GM (2018) Quantification of Liver Fibrosis at T1 and T2 Mapping with Extracellular Volume Fraction MRI: Preclinical Results. Radiology 288 (3):748-754. https://doi.org/10.1148/radiol.2018180051
Tirkes T, Lin C, Fogel EL, Sherman SS, Wang Q, Sandrasegaran K (2017) T1 mapping for diagnosis of mild chronic pancreatitis. J Magn Reson Imaging 45 (4):1171-1176. https://doi.org/10.1002/jmri.25428
Huang Y, Sadowski EA, Artz NS, Seo S, Djamali A, Grist TM, Fain SB (2011) Measurement and comparison of T1 relaxation times in native and transplanted kidney cortex and medulla. J Magn Reson Imaging 33 (5):1241-1247. https://doi.org/10.1002/jmri.22543
Kellman P, Wilson JR, Xue H, Bandettini WP, Shanbhag SM, Druey KM, Ugander M, Arai AE (2012) Extracellular volume fraction mapping in the myocardium, part 2: initial clinical experience. J Cardiovasc Magn Reson 14:64. https://doi.org/10.1186/1532-429x-14-64
Ugander M, Oki AJ, Hsu LY, Kellman P, Greiser A, Aletras AH, Sibley CT, Chen MY, Bandettini WP, Arai AE (2012) Extracellular volume imaging by magnetic resonance imaging provides insights into overt and sub-clinical myocardial pathology. Eur Heart J 33 (10):1268-1278. https://doi.org/10.1093/eurheartj/ehr481
Axon AT, Classen M, Cotton PB, Cremer M, Freeny PC, Lees WR (1984) Pancreatography in chronic pancreatitis: international definitions. Gut 25 (10):1107-1112
Zou KH, Tuncali K, Silverman SG (2003) Correlation and simple linear regression. Radiology 227 (3):617-622. https://doi.org/10.1148/radiol.2273011499
Lin LI (1989) A concordance correlation coefficient to evaluate reproducibility. Biometrics 45 (1):255-268
de Bazelaire CM, Duhamel GD, Rofsky NM, Alsop DC (2004) MR imaging relaxation times of abdominal and pelvic tissues measured in vivo at 3.0 T: preliminary results. Radiology 230 (3):652-659. https://doi.org/10.1148/radiol.2303021331
Rinck PA, Muller RN (1999) Field strength and dose dependence of contrast enhancement by gadolinium-based MR contrast agents. Eur Radiol 9 (5):998-1004. https://doi.org/10.1007/s003300050781
Soher BJ, Dale BM, Merkle EM (2007) A review of MR physics: 3T versus 1.5T. Magn Reson Imaging Clin N Am 15 (3):277-290, v. https://doi.org/10.1016/j.mric.2007.06.002
Stanisz GJ, Odrobina EE, Pun J, Escaravage M, Graham SJ, Bronskill MJ, Henkelman RM (2005) T1, T2 relaxation and magnetization transfer in tissue at 3T. Magn Reson Med 54 (3):507-512. https://doi.org/10.1002/mrm.20605
Winston CB, Mitchell DG, Outwater EK, Ehrlich SM (1995) Pancreatic signal intensity on T1-weighted fat saturation MR images: clinical correlation. J Magn Reson Imaging 5 (3):267-271
Balci NC, Smith A, Momtahen AJ, Alkaade S, Fattahi R, Tariq S, Burton F (2010) MRI and S-MRCP findings in patients with suspected chronic pancreatitis: correlation with endoscopic pancreatic function testing (ePFT). J Magn Reson Imaging 31 (3):601-606. https://doi.org/10.1002/jmri.22085
Tirkes T, Fogel EL, Sherman S, Lin C, Swensson J, Akisik F, Sandrasegaran K (2017) Detection of exocrine dysfunction by MRI in patients with early chronic pancreatitis. Abdom Radiol (NY) 42 (2):544-551. https://doi.org/10.1007/s00261-016-0917-2
Watanabe H, Kanematsu M, Tanaka K, Osada S, Tomita H, Hara A, Goshima S, Kondo H, Kawada H, Noda Y, Tanahashi Y, Kawai N, Yoshida K, Moriyama N (2014) Fibrosis and postoperative fistula of the pancreas: correlation with MR imaging findings–preliminary results. Radiology 270 (3):791-799. https://doi.org/10.1148/radiol.13131194
Kimelman T, Vu A, Storey P, McKenzie C, Burstein D, Prasad P (2006) Three-dimensional T1 mapping for dGEMRIC at 3.0 T using the Look Locker method. Invest Radiol 41 (2):198-203
Chen Y, Lee GR, Aandal G, Badve C, Wright KL, Griswold MA, Seiberlich N, Gulani V (2016) Rapid volumetric T1 mapping of the abdomen using three-dimensional through-time spiral GRAPPA. Magn Reson Med 75 (4):1457-1465. https://doi.org/10.1002/mrm.25693
Ma D, Gulani V, Seiberlich N, Liu K, Sunshine JL, Duerk JL, Griswold MA (2013) Magnetic resonance fingerprinting. Nature 495 (7440):187-192. https://doi.org/10.1038/nature11971
Chen Y, Jiang Y, Pahwa S, Ma D, Lu L, Twieg MD, Wright KL, Seiberlich N, Griswold MA, Gulani V (2016) MR Fingerprinting for Rapid Quantitative Abdominal Imaging. Radiology 279 (1):278-286. https://doi.org/10.1148/radiol.2016152037
Bandula S, Banypersad SM, Sado D, Flett AS, Punwani S, Taylor SA, Hawkins PN, Moon JC (2013) Measurement of Tissue interstitial volume in healthy patients and those with amyloidosis with equilibrium contrast-enhanced MR imaging. Radiology 268 (3):858-864. https://doi.org/10.1148/radiol.13121889
Funding
Dr. Tirkes is supported by National Cancer Institute and National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award numbers 1R01DK116963 and U01DK108323 (Consortium for the Study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Li is supported by National Cancer Institute and National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award numbers U01DK108323 and 1R01DK116963. Dr. Li also receives support from MD Anderson Cancer Center under grant number P30CA016672.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
This study was approved by the Institutional Review Board and the requirement for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tirkes, T., Mitchell, J.R., Li, L. et al. Normal T1 relaxometry and extracellular volume of the pancreas in subjects with no pancreas disease: correlation with age and gender. Abdom Radiol 44, 3133–3138 (2019). https://doi.org/10.1007/s00261-019-02071-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02071-7