Abstract
Purpose
To present data from an interim analysis of a Phase II trial designed to determine the feasibility, safety, and efficacy of individualising treatment based on renal dosimetry, by giving as many cycles as possible within a maximum renal biologically effective dose (BED).
Method
Treatment was given with repeated cycles of 7.4 GBq 177Lu-DOTATATE at 8-12-week intervals. Detailed dosimetry was performed in all patients after each cycle using a hybrid method (SPECT + planar imaging). All patients received treatment up to a renal BED of 27 ± 2 Gy (α/β = 2.6 Gy) (Step 1). Selected patients were offered further treatment up to a renal BED of 40 ± 2 Gy (Step 2). Renal function was followed by estimation and measurement of the glomerular filtration rate (GFR).
Results
Fifty-one patients were included in the present analysis. Among the patients who received treatment as planned, the median number of cycles in Step 1 was 5 (range 3-7), and for those who completed Step 2 it was 7 (range 5-8); 73% were able to receive >4 cycles. Although GFR decreased in most patients after the completion of treatment, no grade 3-4 toxicity was observed. Patients with a reduced baseline GFR seemed to have an increased risk of GFR decline. Five patients received treatment in Step 2, none of whom exhibited a significant reduction in renal function.
Conclusions
Individualising PRRT using renal dosimetry seems feasible and safe and leads to an increased number of cycles in the majority of patients. The trial will continue as planned.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Data from several clinical trials show peptide-receptor radionuclide therapy (PRRT) to be a well-tolerated and effective treatment of neuroendocrine tumours (NETs) [1–8]. Although PRRT has been used for the treatment of NETs for many years, there is still room for optimisation in some aspects, one of them being individualised treatment taking into account patient-specific factors to maximise efficacy and minimise toxicity. Dosimetry-based treatment is one way of achieving this.
The dose-limiting organs for PRRT are the bone marrow and the kidneys, the latter being a greater problem when using 90Y-DOTATOC than with 177Lu-DOTATATE [9, 10]. One way of optimising PRRT is to ensure that the tumour receives as many cycles of therapy as possible within reasonable limits for the risk organs. This individualised approach to PRRT has been previously evaluated by Sandstrom et al [11], demonstrating a high variability in the number of cycles achieved using this treatment strategy and a renal absorbed dose (AD) limit of 23 Gy. The current protocol is based on the same principle, but aims to explore the limits of bone marrow and renal dose by putting the dosimetric results in relation to clinical effects and using higher dose limits. This individualised approach demands detailed dosimetry which, in the case of 177Lu-DOTATATE, can be achieved using post-therapeutic scintigraphy, owing to its characteristic of emitting not only the (therapeutic) β--radiation, but also γ-radiation.
There are no established dose limits for bone marrow and kidneys for 177Lu-PRRT, so such data has to be extrapolated from external beam radiotherapy (EBRT) and PRRT with 90Y-DOTATOC. Data from external bilateral kidney irradiation indicate a 5% risk of renal dysfunction at 5 years (TD5/5) at a mean AD of 18-23 Gy and 0.5-1.25 Gy/fraction [12], or at an AD of 15-18 Gy and 2-Gy fractions [13]. The AD leading to a 50% risk of renal damage at 5 years (TD50/5) has been estimated to be 28 Gy [12, 13]. Data from EBRT cannot, however, be directly applied to PRRT due to what can be summarised as the intrinsic differences between external and systemic radiotherapy: different dose rates and fractionation schemes, an inhomogeneous absorbed dose distribution and possibly different radiobiological mechanisms of cytotoxicity resulting in varying biological effect, despite the same amount of energy deposited per unit mass. The linear-quadratic (LQ) radiobiological model is used to convert the AD to the biologically effective dose (BED), taking into account some of these differences [14]. Assuming that the LQ-model is valid for PRRT, the limits extrapolated from EBRT of 18 Gy and 28 Gy would correspond to BED limits of 32 Gy and 50 Gy,Footnote 1 respectively.
Data from clinical trials of PRRT with 90Y-DOTATOC that include dosimetric studies [15, 16] indicate a relationship between renal BED (estimated from pre-treatment scintigraphy or PET) and toxicity. According to MIRD pamphlet no. 20, the BED TD50/5 is 44 Gy (α/β = 2.5 Gy), and the threshold for radiation nephropathy is 33 Gy [14]. These results were applied in a prospective clinical trial [17], where 22 patients completed treatment with repeated cycles of 90Y-DOTATOC with the aim of not exceeding an accumulated renal BED of 37 Gy (α/β = 2.5 Gy), showing no grade 3-4 toxicity at 18-month follow-up.
When attempting to correlate outcomes to AD or BED, it is essential to use an accurate dosimetric method together with a precise definition of effect. So far, published data on the nephrotoxicity of 177Lu-PRRT have mainly been based on planar dosimetry [18, 19], which is known to have inherent limitations regarding the accuracy of activity quantification, and renal function calculated from plasma creatinine as a surrogate for measuring the glomerular filtration rate (GFR). Dose limits similar to those found for EBRT and 90Y-DOTATOC have not been determined. This may be because most patients have received the standard of 4x7.4 GBq, which, as shown below, in the majority of patients leads to a renal BED well below the above-mentioned limits, but also because inaccurate dosimetry and renal function estimates may obscure a relationship between dose and toxicity.
Another difficulty encountered when studying the effect of radiation on renal function is the co-existence of other factors that contribute to a decline in GFR. The classic risk factors for nephropathy (diabetes, hypertension, old age, previous nephrotoxic therapies or procedures) have been proposed to increase the risk of renal failure post-PRRT [9]. However, in a subsequent large meta-analysis, the predictive power of these risk factors was questioned [20]. Also, in a recent analysis of patients receiving a kidney dose of on average 19.3 Gy, none of the included risk factors had a significant effect on renal function [18]. The GFR at the start of PRRT could also affect the risk of subsequent renal failure, as suggested by an analysis of 51 patients treated with 177Lu-DOTATATE, showing that those who had a reduced initial GFR also received a higher renal AD/administered activity [19]. Renal insufficiency is a late occurring toxicity, and a follow-up time of at least 18 months after treatment is required.
Our group has previously compared the results of different dosimetric methods, including planar and SPECT-based methods, to determine the renal BED after 177Lu-DOTATATE treatment [21]. Based on our findings, and in accordance with the indications in MIRD pamphlet no. 26 [22], we designed a Phase II clinical trial using a hybrid planar- and SPECT-based method to continuously evaluate the cumulative renal BED after each cycle, which then guided the number of cycles given. Here, we present the results of an interim analysis of this trial.
The aims of this analysis are to describe how individualised dosimetry-based treatment planning affects the number of cycles each patient receives, and to describe the development of renal function during follow-up, to ensure an acceptable balance between the risks and benefits of therapy. It includes the first 51 patients enrolled in the trial, of 100 patients planned.
Patients and methods
Trial design
This is an interim analysis of a Phase II, multicentre, prospective clinical trial using 177Lu-DOTATATE to treat metastatic neuroendocrine tumours. The trial is being conducted at two Swedish university hospitals, and has been approved by the regional ethics review board and national regulatory authorities. Further details on the protocol can be found at www.clinicaltrials.gov (NCT01456078). All patients have given their written informed consent to participate.
The primary objective of the trial is to study the efficacy and safety of an individualised dosimetry-based treatment with 177Lu-DOTATATE up to a cumulative BED to the kidneys of 27(±2) Gy. Secondary objectives are to study the same aspects but in a selected group of patients without risk factors for renal or haematological toxicity, who may receive treatment up to 40(±2) Gy.
Study population
The basic eligibility criteria for inclusion are: adult patients with histologically verified, progressive metastatic neuroendocrine tumour with a Ki67 index ≤20%; tumour lesions must be measureable according to RECIST v1.1 and have an uptake on somatostatin receptor scintigraphy that is higher than that of normal liver parenchyma; WHO performance status ≤ 2; normal liver and bone marrow function and a baseline measured GFR ≥50 mL/min/1.73 m2, determined by iohexol or 51Cr-EDTA clearance. Risk factors for nephropathy are identified at baseline (diabetes, hypertension, age > 70 years, prior liver embolization, and prior chemotherapy).
Treatment
Each cycle of 177Lu-DOTATATE is given at a standard activity of 7.4 GBq at 8-12-week intervals. A reno-protective amino acid infusion is started 30 min before and continued until 8 h after the infusion of 177Lu-DOTATATE. The number of cycles received by each patient is determined by the accumulated renal BED, evaluation of renal function, haematological tolerance and trimestral radiological evaluations. All patients are offered treatment up to a BED of 27(±2) Gy (Step 1), as long as there is no progression of the disease or treatment-limiting toxicity. Thereafter, those who have no risk factors for haematological or renal toxicity, non-progressive disease and good tolerance, are offered continued treatment up to a cumulative renal BED of 40(±2) Gy (Step 2).
Post-therapy imaging and renal dosimetry
After each cycle, four whole-body anterior-posterior planar scintigraphies are performed (at nominal times 1, 24, 48 or 96 and 168 h post-injection). At 24 h post-injection SPECT/CT imaging and an X-ray scout are also acquired. Images are exported in DICOM format and further processed using the LundADose software for 2D/3D dosimetry developed at our department. The procedure for dosimetry is further described in supplemental data, including considerations related to the renal pharmacokinetics. The AD and BED of left and right kidney are calculated separately, and the mean values are determined. For calculation of BED from the time-dose rate curve, a numerical method is used, taking into account repair of sublethal damage during protracted irradiation [23]. A kidney α/β of 2.6 Gy and monoexponential repair with a half-time of 2.8 h are assumed, in analogy with previous publications [9].
Follow-up of renal function
Renal function is analysed at baseline by serum creatinine, estimation of GFR (eGFR) using the MDRD formula and the measured GFR (mGFR) determined by iohexol or 51Cr-EDTA clearance. Renal function is monitored between cycles using serum creatinine and eGFR before each cycle and mGFR is determined at least once a year, after completion of Step 1 and Step 2, and additionally according to investigator criteria. Follow-up time is defined as time from inclusion to point of last follow-up.
For the present analysis, the development of the median mGFR and the annual change in eGFR (ΔeGFR) are determined. The ΔeGFR is calculated for each patient individually by linear regression to eGFR versus time data and dividing the obtained slope by the initial mGFR value (mGFRi).
As an exploratory analysis, the projected time to a clinically significant reduction in renal function (GFR < 30 mL/min/1.73 m2) is also included, based on the observation that patients who experience radiation nephropathy tend to exhibit a continued decline in renal function [12]. Thus, as an approximation, the product of mGFRi and ΔeGFR is calculated and the time when the GFR reaches 30 mL/min/1.73 m2 (G3 toxicity) determined by extrapolation.
Results
Patient population
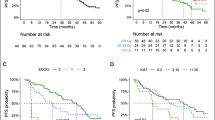
Inclusion of patients in the trial is ongoing, with 51 patients having been included at the time of analysis. The results presented are in part based on all included patients (median follow-up 18 months, range 1-43), in part based only on the patients who had reached end of treatment (EOT) at the time of analysis (EOTall, N = 41, median follow-up 24 months, range 1-43). The patients are further sub-grouped into those who terminated treatment because they had reached the protocol-specified BED limit (EOTdose, N = 22, median follow-up 28 months, range 13-39), or due to toxicity, adverse event or progressive disease (EOTtox/PD, N = 15) as indicated in the text. Treatment was ongoing in ten patients at the time of analysis, and four were excluded from the analysis of effect and toxicity due to protocol deviations. Five patients had received treatment within Step 2.
The baseline characteristics for all 51 patients are presented in Table 1. Half were women, and the median age at inclusion was 67 years (range 35-80). The most common primary tumour origins were small intestine (73%) and pancreas (10%), the rest being evenly distributed between pulmonary, colorectal and unknown origins. Two thirds of the tumours had a Ki67 index of 0-2% and the remaining one-third 3-20%, at the time of diagnosis. The baseline mGFR (mGFRi) median value was 71 mL/min/1.73 m2 (range 48-104), and the median eGFR 87 mL/min/1.73 m2 (range 43-159). One third of the patients had mGFRi >80 mL/min/1.73 m2 (G0 according to NCI CTCAE v4.0), 49% G1 (60-80 mL/min/1.73 m2), and 18% G2 (30-59 mL/min/1.73 m2). The prevalence of risk factors for nephropathy at baseline was as follows: none (39%), one (27%), two (25%), and more than two (8%). Two thirds of the patients had a performance status of ECOG 0-1, and one third had ECOG 2.
Renal dosimetry
The median AD and BED/cycle for all 51 patients were 4.5 Gy (range 2.2-14.3) and 4.9 Gy (range 2.3-19.1), respectively, calculated from a total of 199 cycles. The wide range was due to both inter- and intrapatient variability. The maximum values were attributable to a patient who was admitted to hospital due to intercurrent obstructive nephrolithiasis a few days after receiving treatment. As shown in Fig. 1, the median AD/administered activity was 0.61 Gy/GBq (range 0.3-1.98), and the median BED/AD was 1.09 (range 1.03-1.34). The median BED/administered activity was 0.67 Gy/GBq (range 0.3-2.6), and the median effective half-life was 51.6 h (range 38-69) (data not shown). The AD and BED of the left and right kidneys were generally similar in the same patient and cycle. The fractional BED deviation, calculated as the difference between the left and right kidney divided by the mean of the left and right kidney, was on average -1.8% for individual cycles and -0.2% for the whole treatment. No systematic difference in the BED of the left and right kidneys was seen, although in the above-mentioned patient with obstructive nephrolithiasis the BED differed for non-methodological reasons.
The median interval between cycles was 77 days (range 56-210). The median number of cycles received within Step 1 by the EOTdose patients was five (range 3-7) reaching a mean renal BED of 26.5 Gy (range: 22.6-32.1). The five patients who completed treatment within Step 2 received a median of seven cycles (range 5-8) reaching a mean renal BED of 37.3 Gy (range: 33.1-39.8). The individual results are illustrated in Fig. 2, where the considerable inter- and intrapatient variability regarding the BED/cycle and the total number of cycles is evident. As an illustrative example, we can compare patients 111 and 112, who both received treatment up to an accumulated BED of approximately 25 Gy, one after only three cycles, while the other required six cycles. Conversely, patients 015 and 016 received the same number of cycles, but very different total kidney BEDs (36 Gy vs. 26 Gy).
In the EOTdose group 16/22 patients (73%) received more and 2/22 (9%) received less than four cycles. As illustrated in Fig. 3, this leaves only four patients (18%) for whom four is the optimal number of cycles according to the BED limits used in this protocol. If all 22 patients had received four cycles, the mean renal BED would have been 22.7 (range 14.3-38.1) Gy (assuming the same BED in cycle 4 as in cycle 3 for the patients who only received three cycles).
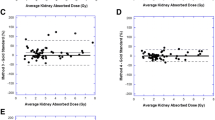
Renal function vs. cumulative renal BED
In the EOTall group, data on eGFR development ≥ 6 months from baseline were available for 32 patients (median follow-up 19 months), while follow-up data on mGFR were available for 22 (median follow-up 22 months). The contribution of cumulative BED, mGFRi, and pre-existing risk factors for nephrotoxicity was compared pair-wise (Fig. 4). Based on the observation that the EOTtox/PD patients were overrepresented in the group exhibiting a more rapid decline in GFR (see Table 2), these were analysed separately. The patients with the smallest GFR-loss were those with an mGFRi ≥ 80 mL/min/1.73 m2, including those treated to a BED of 40(±2) Gy, and those with the largest GFR loss was the EOTtox/PD group. All patients with a GFR loss > 10% either had mGFRi < 80 mL/min/1.73 m2 and/or risk factors for nephrotoxicity. The dose-limiting toxicity was haematological (Table 2).
Pair-wise comparisons of ΔeGFR for the EOTdose group (N = 22) and an eGFR follow-up >6 months categorized by initial mGFR (mL/min/1.73 m2), the existence or not of risk factors (Risk F) for nephrotoxicity, and the cumulative renal BED (Gy). The results for the EOTtox/PD group (N = 10) are presented in the column to the left
Renal function over time
As illustrated in Fig. 5a, median mGFR decreased with increasing follow-up, although the number of patients with a follow-up >24 months is small, making it difficult to draw any conclusions beyond this point in time. The mean absolute annual change in mGFR was -4.3 mL/min/1.73 m2 (range +11 to -30), while the mean annual GFR-loss in a normal population of a similar age range is between 0.4 ± 3.6 and 1.8 ± 2.6 mL/min [24]. The loss of renal function among the PRRT-treated patients was thus slightly more rapid, although no grade 3-4 toxicity (i.e. GFR < 30 mL/min/1.73 m2) was observed. As illustrated in Fig. 5b, four patients exhibited a decrease in eGFR >30% compared to baseline, one of whom was the patient with obstructive nephrolithiasis, two had progressive disease at the time the decrease in renal function was confirmed, and in the fourth patient the decline in eGFR improved, from -30% to -24%, with further follow-up.
Among the five patients who received treatment within Step 2, the mean change in mGFR from baseline to the last point of follow-up was -7% (range -14% to +5%), while the mean change in eGFR was -14% (range -25% to +7%). Two patients exhibited a reduction in renal function from G0 to G1, while G0 renal function was maintained in three patients throughout follow-up (data not shown). The median mGFR follow-up for this subgroup was 29 months (range 24-37).
Figure 6 shows results of the exploratory analysis of the time when significant renal toxicity would be reached (grade 3, GFR <30 mL/min/1.73 m2). Six patients (19%) actually showed an improvement in GFR during follow-up, five of which had risk factors for nephrotoxicity. None had a projected decline to GFR < 30 mL/min/1.73 m2 within 1 year, but it was projected within 2-5 years for six patients (34%). The projected time to GFR <30 mL/min/1.73 m2 was 6-10 years in five patients (22%) and longer than 10 years in seven patients (25%).
Discussion
In the present trial, we have prospectively collected data on renal function and dosimetry after 177Lu-DOTATATE PRRT and individualised treatment based on an assumed maximum tolerable dose to risk organs, with the aim of maximising the AD to tumour tissue and thus the probability of antitumor effect. When seeking to define a relationship between absorbed dose and toxicity, it is essential to have accurate measurements of both. In this trial, we used an ambitious dosimetric method together with regular measurement and estimation of renal function, to be able to draw firm conclusions as the number of patients and follow-up time increases.
A challenge when designing the trial was to define the BED limits in a way that increased the likelihood of therapeutic gain without venturing patient safety. As summarised in the introduction, the evidence available would indicate a threshold for long-term nephrotoxicity of 32-33 Gy, without taking into account clinical risk factors. Based on Bodei et al [9] risk factors for nephrotoxicity seemed to clearly affect the recommendable BED limits. Based on this, we defined the renal BED-limits to 27 for patients with risk factors and 40 Gy for those without.
When the physician sees a patient after X cycles and a cumulated renal BED of Y Gy, aware that the renal dose varies from one cycle to another, he/she has to attempt to predict the cumulative BED with additional cycles. Certain variability in the final dose (±2 Gy) was, therefore, added as a compromise with clinical reality. In a previous study we also investigated the combined uncertainties in SPECT/CT-based renal dosimetry in 177Lu-PRRT, using the same SPECT/CT methods as in this study, and were able to quantify one standard deviation to 6% [25]. Currently we are performing uncertainty analyses for the hybrid planar-SPECT method used in this trial. The results are beyond the scope of this work and will, therefore, be presented separately.
One may object to there being no upper dose limit for the bone marrow (BM) in this trial. Sandstrom et al, however, found that the BM AD/cycle was <0.2 Gy and concluded that it was the renal AD that was dose-limiting in 98% of the patients, even when permitting a renal AD up to 29 Gy [11]. The acute BM toxicity is monitored using blood sampling at regular intervals during treatment. Since acute BM toxicity is easily detected, and the limit of BM AD is yet undefined for PRRT, we decided to study BM AD in an exploratory substudy, the results of which will be presented separately. For a majority of the patients the whole-body AD has been determined (see Table 2).
A fundamental difficulty with dosimetry in PRRT is the lack of radiobiological data regarding dose-response relationships for tumour and normal tissues. The data that does exist suffers from considerable variability in radionuclides, dosimetric methods, and clinical data making pooling of results difficult. We are obliged to extrapolate from EBRT and the LQ-model without knowing its applicability to PRRT when taking into account the numerous physical and biological differences between the treatment modalities. To be able to go forward with studies incorporating rigorous dosimetry and clinical follow-up which may add to the knowledge base, we inevitably have to make certain assumptions a priori based on the best available evidence, and continuously re-evaluate the correctness of these assumptions as results become available.
Estimation of GFR based on plasma creatinine is subject to inaccuracies which vary depending on the method used. The MDRD and the Cockcroft-Gault formulas are the most commonly used, and recent reviews support MDRD as being somewhat more reliable [26, 27]. Superior to any estimation of GFR is its measurement, limited on the other hand by its more invasive nature. In this trial we followed renal function using both estimated and measured values. We used the less invasive method (eGFR) for close follow-up of changes in renal function, with regular mGFR measurements to calibrate the eGFR values. Assuming that the difference between eGFR and mGFR data is constant over time for the same patient, the possible bias in eGFR values will not affect the rate of the change. The percent change on the other hand depends on the value used for normalization, for which the initial mGFR value was used.
In our patient material renal function gradually declined after treatment with 177Lu-DOTATATE, at a rate that seemed slightly higher than what could be expected in a corresponding normal population. The decline was moderate, with no grade 3-4 toxicity observed so far. Patients with risk factors for nephrotoxicity, or a moderately reduced mGFRi, seemed at risk of a more rapid decline in renal function than their healthier counterparts. A possible explanation is that risk factor patients have a lower number of functioning nephrons at baseline than their no-risk factor counterparts and are, therefore, at greater risk of suffering a clinically significant reduction in GFR as a result of nephrotoxic therapies such as PRRT. The patients showing the highest risk of GFR decline were actually those who were not able to complete PRRT as planned, due to non-renal toxicity/adverse event or progressive disease. This suggests that factors other than the radiation dose to the kidneys caused their nephropathy. Our results support the dose limit proposed in this trial for high-risk patients (27 ± 2 Gy), while indicating that low-risk patients may well tolerate further treatment.
The primary objective of PRRT in patients with progressive NETs is to bring the tumour under control. Some deterioration in renal function is acceptable, as long as it does not affect the patients’ quality of life for the remainder of their lifetime. Patients with radiation nephropathy tend to have a continuous progressive decline in renal function. Although the rate of this decline is unknown, it is valuable from the clinician’s point of view to have some idea of the prognosis for toxic effects in relation to the expected therapeutic effects of the treatment and survival of the patient. For this reason we have attempted to predict the long-term effects on renal function by extrapolating the rate of change of eGFR calculated for each patient to give an approximate time to significant renal insufficiency, defined as ≥ G3. As for any exploratory analysis, the results have to be interpreted with caution.
Our findings clearly show that individualising treatment based on patient selection and detailed dosimetry results in considerable variability in the number of cycles each patient is able to receive within the pre-specified BED limits. Not only does the AD/cycle vary between patients, but also between cycles in the same patient. The reason for the intra-individual variations is presently unclear, although it may be that blood pressure and degree of hydration, and thus renal perfusion, varied between cycles secondarily affecting the residence time in the kidney and thereby the AD. Previous authors [18] have stated that the risk of nephrotoxicity after standard PRRT with four cycles is minimal, rendering dosimetry superfluous. However, if the goal is the optimization of efficacy vs. toxicity, or if retreatment is being considered, we maintain that dosimetry is necessary, based on the findings in the present analysis.
Conclusions
Individualised dosimetry-based PRRT is feasible and safe, with the BED limits used in this protocol, with the caveat of the limited follow-up inherent to an interim analysis. The trial will continue as planned.
Notes
If not otherwise specified, an α/β value of 2.6 Gy has been used for the BED-calculations.
References
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, et al. Treatment with the radiolabeled somatostatin analog [177 Lu-DOTA 0, Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol: Off J Am Soc Clin Oncol. 2008;26(13):2124–30. doi:10.1200/JCO.2007.15.2553.
Imhof A, Brunner P, Marincek N, Briel M, Schindler C, Rasch H, et al. Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol: Off J Am Soc Clin Oncol. 2011;29(17):2416–23. doi:10.1200/JCO.2010.33.7873.
Bodei L, Cremonesi M, Grana CM, Fazio N, Iodice S, Baio SM, et al. Peptide receptor radionuclide therapy with 177Lu-DOTATATE: the IEO phase I-II study. Eur J Nucl Med Mol Imaging. 2011;38(12):2125–35. doi:10.1007/s00259-011-1902-1.
Kunikowska J, Krolicki L, Hubalewska-Dydejczyk A, Mikolajczak R, Sowa-Staszczak A, Pawlak D. Clinical results of radionuclide therapy of neuroendocrine tumours with 90Y-DOTATATE and tandem 90Y/177Lu-DOTATATE: which is a better therapy option? Eur J Nucl Med Mol Imaging. 2011;38(10):1788–97. doi:10.1007/s00259-011-1833-x.
Filice A, Fraternali A, Frasoldati A, Asti M, Grassi E, Massi L, et al. Radiolabeled somatostatin analogues therapy in advanced neuroendocrine tumors: a single centre experience. J Oncol. 2012;2012:320198. doi:10.1155/2012/320198.
Villard L, Romer A, Marincek N, Brunner P, Koller MT, Schindler C, et al. Cohort study of somatostatin-based radiopeptide therapy with [(90)Y-DOTA]-TOC versus [(90)Y-DOTA]-TOC plus [(177)Lu-DOTA]-TOC in neuroendocrine cancers. J Clin Oncol: Off J Am Soc Clin Oncol. 2012;30(10):1100–6. doi:10.1200/JCO.2011.37.2151.
Danthala M, Kallur KG, Prashant GR, Rajkumar K, Raghavendra RM. (177)Lu-DOTATATE therapy in patients with neuroendocrine tumours: 5 years’ experience from a tertiary cancer care centre in India. Eur J Nucl Med Mol Imaging. 2014;41(7):1319–26. doi:10.1007/s00259-014-2710-1.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 Trial of 177Lu-Dotatate for Midgut Neuroendocrine Tumors. N Engl J Med. 2017;376(2):125–35. doi:10.1056/NEJMoa1607427.
Bodei L, Cremonesi M, Ferrari M, Pacifici M, Grana CM, Bartolomei M, et al. Long-term evaluation of renal toxicity after peptide receptor radionuclide therapy with 90Y-DOTATOC and 177Lu-DOTATATE: the role of associated risk factors. Eur J Nucl Med Mol Imaging. 2008;35(10):1847–56. doi:10.1007/s00259-008-0778-1.
Valkema R, Pauwels SA, Kvols LK, Kwekkeboom DJ, Jamar F, de Jong M, et al. Long-term follow-up of renal function after peptide receptor radiation therapy with (90)Y-DOTA(0), Tyr(3)-octreotide and (177)Lu-DOTA(0), Tyr(3)-octreotate. J Nucl Med: Off Publ, Soc Nucl Med. 2005;46 Suppl 1:83S–91S.
Sandstrom M, Garske-Roman U, Granberg D, Johansson S, Widstrom C, Eriksson B, et al. Individualized dosimetry of kidney and bone marrow in patients undergoing 177Lu-DOTA-octreotate treatment. J Nucl Med: Off Publ, Soc Nucl Med. 2013;54(1):33–41. doi:10.2967/jnumed.112.107524.
Dawson LA, Kavanagh BD, Paulino AC, Das SK, Miften M, Li XA, et al. Radiation-associated kidney injury. Int J Radiat Oncol Biol Phys. 2010;76(3 Suppl):S108–15. doi:10.1016/j.ijrobp.2009.02.089.
Marks LB, Yorke ED, Jackson A, Ten Haken RK, Constine LS, Eisbruch A, et al. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys. 2010;76(3 Suppl):S10–9. doi:10.1016/j.ijrobp.2009.07.1754.
Wessels BW, Konijnenberg MW, Dale RG, Breitz HB, Cremonesi M, Meredith RF, et al. MIRD pamphlet No. 20: the effect of model assumptions on kidney dosimetry and response--implications for radionuclide therapy. J Nucl Med: Off Publ, Soc Nucl Med. 2008;49(11):1884–99. doi:10.2967/jnumed.108.053173.
Barone R, Borson-Chazot F, Valkema R, Walrand S, Chauvin F, Gogou L, et al. Patient-specific dosimetry in predicting renal toxicity with (90)Y-DOTATOC: relevance of kidney volume and dose rate in finding a dose-effect relationship. J Nucl Med: Off Publ, Soc Nucl Med. 2005;46 Suppl 1:99S–106S.
Bodei L, Cremonesi M, Grana C, Rocca P, Bartolomei M, Chinol M, et al. Receptor radionuclide therapy with 90Y-[DOTA]0-Tyr3-octreotide (90Y-DOTATOC) in neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2004;31(7):1038–46. doi:10.1007/s00259-004-1571-4.
Van Binnebeek S, Baete K, Vanbilloen B, Terwinghe C, Koole M, Mottaghy FM, et al. Individualized dosimetry-based activity reduction of 90Y-DOTATOC prevents severe and rapid kidney function deterioration from peptide receptor radionuclide therapy. Eur J Nucl Med Mol Imaging. 2014;41(6):1141–57. doi:10.1007/s00259-013-2670-x.
Bergsma H, Konijnenberg MW, van der Zwan WA, Kam BL, Teunissen JJ, Kooij PP, et al. Nephrotoxicity after PRRT with Lu-DOTA-octreotate. Eur J Nucl Med Mol Imaging. 2016. doi:10.1007/s00259-016-3382-9.
Svensson J, Berg G, Wangberg B, Larsson M, Forssell-Aronsson E, Bernhardt P. Renal function affects absorbed dose to the kidneys and haematological toxicity during 177Lu-DOTATATE treatment. Eur J Nucl Med Mol Imaging. 2015;42(6):947–55. doi:10.1007/s00259-015-3001-1.
Bodei L, Kidd M, Paganelli G, Grana CM, Drozdov I, Cremonesi M, et al. Long-term tolerability of PRRT in 807 patients with neuroendocrine tumours: the value and limitations of clinical factors. Eur J Nucl Med Mol Imaging. 2015;42(1):5–19. doi:10.1007/s00259-014-2893-5.
Garkavij M, Nickel M, Sjogreen-Gleisner K, Ljungberg M, Ohlsson T, Wingardh K, et al. 177Lu-[DOTA0, Tyr3] octreotate therapy in patients with disseminated neuroendocrine tumors: Analysis of dosimetry with impact on future therapeutic strategy. Cancer. 2010;116(4 Suppl):1084–92. doi:10.1002/cncr.24796.
Ljungberg M, Celler A, Konijnenberg MW, Eckerman KF, Dewaraja YK, Sjogreen-Gleisner K. MIRD Pamphlet No. 26: Joint EANM/MIRD Guidelines for Quantitative 177Lu SPECT Applied for Dosimetry of Radiopharmaceutical Therapy. J Nucl Med: Off Publ, Soc Nucl Med. 2016;57(1):151–62. doi:10.2967/jnumed.115.159012.
Gustafsson J, Nilsson P, Gleisner KS. On the biologically effective dose (BED)-using convolution for calculating the effects of repair: II. Numerical considerations. Phys Med Biol. 2013;58(5):1529–48. doi:10.1088/0031-9155/58/5/1529.
Shlipak MG, Katz R, Kestenbaum B, Fried LF, Newman AB, Siscovick DS, et al. Rate of kidney function decline in older adults: a comparison using creatinine and cystatin C. Am J Nephrol. 2009;30(3):171–8. doi:10.1159/000212381.
Gustafsson J, Brolin G, Cox M, Ljungberg M, Johansson L, Gleisner KS. Uncertainty propagation for SPECT/CT-based renal dosimetry in (177)Lu peptide receptor radionuclide therapy. Phys Med Biol. 2015;60(21):8329–46. doi:10.1088/0031-9155/60/21/8329.
Erbas B, Tuncel M. Renal Function Assessment During Peptide Receptor Radionuclide Therapy. Semin Nucl Med. 2016;46(5):462–78. doi:10.1053/j.semnuclmed.2016.04.006.
Methods to Estimate and Measure Renal Function (Glomerular Filtration Rate): A Systematic Review (2011) SBU Systematic Review Summaries. Stockholm
Acknowledgements
The authors wish to acknowledge the contribution to this work from medical physicists Cecilia Hindorf and Erik Larsson, technologists Nadja Mortensen and Rebecca Hermann and research nurses Charlotte Fogelström and Kajsa Holgersson.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
This trial is made possible by research grants from the Swedish Research Council (grant # 621-2014-6187), Swedish Cancer Society, Mrs. Berta Kamprad’s Foundation, Gunnar Nilsson’s Foundation, Swedish Radiation Safety Authority and Jubilee Clinic Cancer Research Foundation.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 35 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sundlöv, A., Sjögreen-Gleisner, K., Svensson, J. et al. Individualised 177Lu-DOTATATE treatment of neuroendocrine tumours based on kidney dosimetry. Eur J Nucl Med Mol Imaging 44, 1480–1489 (2017). https://doi.org/10.1007/s00259-017-3678-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3678-4