Abstract
Purpose
Radionuclide therapy with 177Lu-DOTATATE is well established for patients with advanced somatostatin receptor–positive neuroendocrine tumors with a standard schedule of 7.4 GBq at four occasions. However, this approach does not consider individual variability affecting the tumor radiation dose or dose to organs at risk. Therefore, it is important to assess more personalized strategies. The aim of this phase II trial was to evaluate individualized 177Lu-DOTATATE for which the number of cycles varied based on renal dosimetry.
Methods
Patients were eligible if they had a progressive, somatostatin receptor–positive neuroendocrine tumor with a Ki 67 labeling index < 20%. They received cycles of 7.4 GBq of 177Lu-DOTATATE at 10 ± 2-week intervals until a predefined radiation dose to the kidneys was reached. The primary endpoint was objective tumor response (RECIST v 1.1). Secondary endpoints included progression-free survival (PFS), overall survival (OS), and toxicity (CTCAE v. 4.0).
Results
Ninety-six patients who had received a median of 5 cycles (range 1–9) were evaluable for efficacy. The objective tumor response was 16% partial response, 66% stable disease, and 19% progressive disease. The median PFS and OS were 29 months and 47 months, respectively, and were significantly associated with kidney dose, performance status, and Ki 67 levels but not with tumor origin. The overall toxicity was mild, and the most common events were grade 1–2 anemia, thrombocytopenia, fatigue, nausea, and diarrhea. Grade 3–4 toxicity occurred in < 10% of patients and was mostly hematological, with no grade 3–4 renal toxicity.
Conclusion
Individualized treatment with 177Lu-DOTATATE based on renal dosimetry is clearly feasible with low toxicity and promising efficacy, showing the potential to further improve outcome beyond the standard approach, and should be further assessed in randomized trials.
Trial registration
EudraCT 2011–000,240-16. NCT01456078. https://clinicaltrials.gov/ct2/show/NCT01456078
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peptide receptor radionuclide therapy (PRRT) using 177Lu-DOTATATE is a valuable treatment option for patients with somatostatin receptor–positive neuroendocrine tumors (NETs). A somatostatin analog (octreotate) coupled to the radionuclide 177Lu binds to somatostatin receptors overexpressed on tumor cells, thus delivering ionizing radiation in a molecularly targeted radiotherapy approach. The treatment effect is due to DNA damage by the beta-particles emitted from 177Lu, whereas gamma radiation enables imaging for uptake mapping and dosimetry.
PRRT is endorsed by the major neuroendocrine societies [1,2,3] and approved for treatment of gastroenteropancreatic tumors (GEPNETs) (by the European Medicines Agency and the US Food and Drug Administration). The evidence of the efficacy and safety of 177Lu-DOTATATE was long based on retrospective and single-arm studies [4, 5]. In 2017, this evidence was complemented with the results from the NETTER-1 trial, a randomized phase III trial where the superiority of 177Lu-DOTATATE over somatostatin analogs (SSAs) was demonstrated for small intestinal NETs (SiNETs), the largest subgroup of GEPNETs [6].
The approved treatment approach of using a fixed activity of 7.4 GBq 177Lu-DOTATATE in four cycles is safe but not necessarily the most effective treatment for individual patients, nor is it in line with current European legislation [7]. In radiotherapy, dose–response relationships are proven for most tumors [8], and the aim is to deliver a sufficiently high dose to the tumor with acceptable exposure to the organs at risk. The same type of dose–response/dose-toxicity relationships can be applied to radionuclide therapy, as is being confirmed by a growing body of evidence through the use of image-based dosimetry in prospective clinical trials [9,10,11,12,13,14].
The main organs at risk are the kidneys and bone marrow. While bone marrow toxicity presents early and is therefore readily detected, renal toxicity occurs months to years after treatment. The exposure of the kidneys in PRRT is due to an active reabsorption of 177Lu-DOTATATE in the renal proximal tubules [15], which can be partially inhibited by a parallel infusion of amino acids [16]. Previous experience with PRRT using 90Y has demonstrated dose-dependent renal toxicity at a biologically effective dose (BED) of 28 Gy for patients with risk factors for renal toxicity and 40 Gy for those without risk factors [17]. A renal BED above 45 Gy was correlated with a high risk of rapid decline in renal function [18]. The radiation exposure of the kidneys therefore needs to be monitored. Carrying out as many treatment cycles as possible within a predefined dose limit to the kidneys is a first step towards dosimetry-based, individualized PRRT.
To improve the efficacy of 177Lu-DOTATATE, the concept of an individually optimized treatment strategy needs to be further pursued and could be developed by adjusting the injected activity, modifying the treatment intervals, or increasing the total number of cycles. The latter strategy was assessed in the present phase II trial (ILUMINET), where the safety and efficacy of individualized 177Lu-DOTATATE treatment based on the estimated renal BED were evaluated. Here we present the final results.
Material and methods
Patients
The main eligibility criteria were histologically verified irresectable neuroendocrine tumors irrespective of origin, with a Ki 67 labeling index of ≤ 20% and an ECOG performance status (PS) of 0, 1, or 2. The disease had to be progressive on CT scan during the last 14 months. Tumor uptake higher than basal liver uptake on a 111In-Octreotide scan was required. Other inclusion criteria were measurable disease according to RECIST v 1.1 criteria, adequate bone marrow and liver function, a measured glomerular filtration rate (GFR) of > 50 ml/min, and a stable dose of somatostatin analog (SSA) during the last 3 months prior to inclusion. Key exclusion criteria were chemotherapy or local treatment during the last 3 months, concomitant nephrotoxic drugs, and previous external beam radiotherapy to > 25% of the bone marrow.
Patients entering step 2 (see “Study design and treatment”) had to have maintained a GFR > 50 ml/min with a maximum decrease of 40% from baseline, no grade 3–4 toxicity, and a maximum age of 70 years. Furthermore, patients were excluded from step 2 if they had a history of diabetes or uncontrolled hypertension or if they previously had received liver embolization or chemotherapy.
The trial was conducted in accordance with ICH GCP and the Declaration of Helsinki and was approved by the regional ethics review board (EPN Lund 2011/287).
Study design and treatment
The ILUMINET trial was a single-arm, phase II trial conducted at two tertiary referral centers in Sweden. The safety and efficacy of individualized 177Lu-DOTATATE treatment based on renal dosimetry were evaluated with the hypothesis that treatment may be optimized by adjusting the number of cycles to the individually estimated renal BED [17, 19]. All patients were planned for treatment up to a cumulative renal BED of 27 ± 2 Gy (step 1). Thereafter, patients complying with the inclusion and exclusion criteria for step 2 (see “Patients”) were offered further treatment up to a renal BED of 40 ± 2 Gy.
Treatment was administered as intravenous infusions of 7.4 GBq 177Lu-DOTATATE, at 10 ± 2-week intervals, preceded by antiemetics and co-administered with a kidney-protective amino acid infusion (2 L VAMIN® 14 g N/l starting 30 min before treatment and continued for 8 h). Long-acting SSA was withheld at least 4 weeks before the administration of each cycle. For dosimetry, four planar whole-body scintigraphies (1 h, 24 h, 48 or 96 h, and 168 h post infusion) and one combined SPECT/CT (24 h) were performed, from which the BED was calculated as previously described [20].
Endpoints and assessments
The primary endpoint was objective tumor response 3 months after completing step 1, based on RECIST v 1.1 criteria. The main secondary endpoints were progression-free survival (PFS), overall survival (OS), toxicity according to CTCAE v. 4.0 criteria, and health-related quality of life. Renal toxicity was considered an adverse event (AE) of special interest and is therefore explained separately. Exploratory endpoints included the effect of renal BED, Ki 67, PS, and tumor origin on PFS and OS, as well as best overall response, time to maximum response, and time to progression (TTP). All time-to-event endpoints were estimated from date of inclusion. For comparison of efficacy based on renal BED, the delivered (rather than the targeted) BED was used to group the patients into “ < 25 Gy,” “25–29 Gy,” and “ > 29 Gy.”
Patients were followed during the treatment phase and follow-up with CT scans of the thorax and abdomen every 3 months, including RECIST evaluation. Plasma creatinine and an estimated GFR were determined at each follow-up visit, and a GFR measurement was performed yearly. Peripheral blood values were assessed weekly for 6 weeks after each treatment cycle, before each new cycle, and at 3-month intervals during follow-up. Toxicity was analyzed separately for early (from the start of therapy to 3 months after completing step 1) and late (6 and 12 months after the last treatment) adverse events.
Bone marrow (BM) dosimetry was also conducted with a previously described image-based methodology, and health-related quality of life was assessed with the EORTC QLQ-C30 and EORTC QLQ-GI NET21 questionnaires. These data will be analyzed and reported separately.
Statistical analysis
Based on an expected objective response rate of 20–40%, 100 patients were needed to obtain a 95% confidence interval with a margin of error of 10%.
Descriptive statistics are presented using the median and range for continuous variables and the count and percentage for categorical variables. Univariate analysis was performed on PFS and OS dependence on stratification on kidney BED, ECOG and Ki 67.
Confidence intervals for proportions were calculated using the Wald method. Kaplan–Meier curves were used to evaluate OS and PFS. Log rank tests were used to test for differences in OS and PFS between subgroups. All statistical analyses were performed in R version 4.0.2 [21].
Results
Patients and treatment
Between October 2011 and June 2018, 97 patients were enrolled. One patient never received treatment due to withdrawal of consent. The baseline characteristics of the remaining 96 patients are shown in Table 1.
Because there were five deaths before radiologic assessment and one case of protocol deviation, 90 patients were evaluable for the primary endpoint of objective tumor response. The total population of 96 patients was evaluable for OS and toxicity, and 94 patients were evaluated for PFS and TTP. Ninety patients were evaluable for the exploratory objectives of time to maximum response and best overall tumor response.
Thirty-two patients terminated treatment before completing step 1. The reasons for termination were death (n = 7), toxicity (n = 13), and progressive disease (n = 12). Of the 64 patients completing step 1, nine continued to receive additional treatment in step 2. The median number of treatment cycles for all patients was 5 (1–9), with 51 patients (53%) receiving more than four cycles. For comparison of efficacy, patients were grouped based on received renal BED: < 25 Gy (n = 61), 25–29 Gy (n = 24), and > 29 Gy (n = 11).
Efficacy
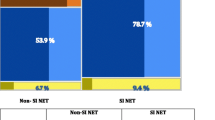
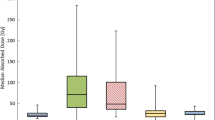
The median follow-up at the time of analysis was 42 months. The objective tumor response 3 months after step 1 was 16% partial response (PR) (95% CI, 8.1 to 23%), 66% stable disease (SD) (95% CI, 56 to 75%), and 19% progressive disease (PD) (95% CI, 11 to 27%). The PFS and OS were 29 months and 47 months, respectively (Figs. 1a and 2a), with a 5-year survival of 41% (95% CI, 31 to 54%). When analyzing PFS and OS, there were significant differences according to renal BED and ECOG (Figs. 1b, c and 2b, c), while for Ki67, there were differences for PFS but not for OS (Figs. 1d and 2d). There were no significant differences in median PFS or OS according to tumor origin (data not shown). The best overall response (including step 2) was 2% complete response (CR) (95% CI, none to 5%), 32% PR (95% CI, 23 to 42%), 61% SD (95% CI, 51 to 71%), and 4% PD (none to 9%) (Fig. 3).
The median time to maximum response was 18 months for all patients (95% CI, 16 to 22) and 13 (95% CI, 11 to 19 months), 23 (95% CI, 18 to 31 months), and 28 months (95% CI, 17 to 36 months) for the three renal BED groups < 25 Gy, 25–29 Gy, and > 29 Gy, respectively. The median TTP was 41 months (95% CI, 29 to 48 months) for all patients and 31 (95% CI, 22 to 46 months), 46 (95% CI, 26 months to not reached), and 48 months (95% CI, 36 months to not reached) for the renal BED groups < 25 Gy, 25–29 Gy, and > 29 Gy, respectively. The differences in TTP based on stratification were not significant.
Safety
The overall toxicity was mild, with few grade 3–4 adverse events (AEs). AEs are summarized in Table 2.
In terms of early AE, the most common (> 5%) clinical AEs were grade 1–2 fatigue, nausea, pain, diarrhea, abdominal pain, flushing, and alopecia. Grade 3 events were reported in single patients experiencing thromboembolic disease, nausea, and pain. No grade 4 clinical AEs were registered. Hematological AEs were common, with grade 1–2 anemia and thrombocytopenia occurring in more than half of the patients. Grade 3–4 laboratory findings were observed in 1–9% of patients, including hematological AEs and liver enzyme increase.
Regarding late AEs, the only clinical AE occurring in > 5% of the patients and persisting 12 months after treatment was grade 1 fatigue. There was one grade 3–4 clinical AE, a thromboembolic event. The only persisting laboratory findings were grade 1–2 hematological AEs, whereas all grade 3–4 AEs occurred in < 5% of the patients at 12 months. During follow-up, two patients were diagnosed with acute myeloid leukemia 2 and 4 years after the first cycle of 177Lu-DOTATATE. The patients were 69 and 76 years old, had received no systemic treatment other than SSA against their SiNETs, and were treated with 4 and 6 cycles, respectively.
Among the seven patients who completed treatment in step 2, there was no grade 3–4 AE, neither early nor late clinical or hematological/biochemical. All seven patients had a GFR > 60 ml/min at baseline, and four of them maintained this level at the time of last follow-up. The remaining three patients had a last measured GFR of 30–60 ml/min. Median follow-up for this subgroup was 45 months.
Twelve patients terminated the study before completing step 1 due to AEs, 11 due to hematological toxicity (10 had grade 1–3 thrombocytopenia together with either grade 2–3 neutropenia or grade 1–3 anemia; one patient had grade 3 neutropenia as the only reason for early termination of treatment). Three of the 11 patients had received 5 cycles of treatment, and the remaining eight had received only 2–3 cycles, with three of these having been pre-treated with radiation- or chemotherapy. The patients that terminated treatment early did not have a higher median age nor had they received more lines of treatment before entering the trial. The presence of bone metastases may have influenced the tolerability due to higher mean absorbed doses, as shown earlier [22], but this remains to be confirmed in the present patient material.
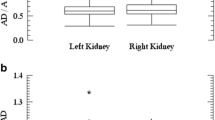
Measured GFR values after terminating the treatment phase were available for 71 patients, with a median follow-up of 29 months. At this point, 59% of patients had a GFR > 60 ml/min (grade 0–1) compared to 82% at baseline, and 39% of patients had a GFR of 30–60 ml/min (grade 2) compared to 18% at baseline. There was one case of grade 3 toxicity related to intercurrent nephrolithiasis. Plasma creatinine levels increased over time, leading to an increase in the frequency of grade 1 toxicity (i.e., p-creatinine 100–150 µmol/L) during follow-up: 17% at baseline vs. 47% at 36 months of follow-up. There was one case of grade 2 renal toxicity and no grade 3–4 events.
Discussion
The results of this trial show that dosimetry-based PRRT for NET patients is safe and effective. Direct comparisons to the standard treatment used in the NETTER-1 trial are difficult since there are significant differences in the patient populations and trial designs, e.g., the proportion of low-grade NETs (2/3 in NETTER-1 and 1/3 in ILUMINET) and the time to progression prior to trial entry (36 months in NETTER-1 and 14 months in ILUMINET). Despite the higher risk population in ILUMINET, the best overall response rate of 34% compares favorably and the PFS and OS of 29 and 47 months repectively is simular to the results of NETTER-1 (18%, 28 and 48 months, respectively) [23].
Dosimetry-based PRRT has been conducted and reported by two other groups. The Uppsala observational study [24] had a design similar to ILUMINET, but the patient population included high-grade tumors. The number of cycles they administered was 1–10, median not reported, with 48% receiving more than four cycles. They reported a PFS of 27 months, with a response rate of 24%.
A Canadian trial used the same renal dose limit as the Uppsala study (23 Gy), but instead of varying the number of treatment cycles, they adjusted the injected activity in such a way that the renal dose limit was reached in four cycles [25]. This group reported a high response rate of 59% but a surprisingly short PFS of 16 months, and a high rate of, mainly hematological, grade 3–4 toxicity. This raises the question of the importance of the fractionation schedule—is it better to give smaller, repeated doses over a longer period of time than to give the same amount of activity over a shorter period? In the current study, the total median injected activity/patient was 37 GBq, compared to 36 GBq in the study by Del Prete et al. The duration of treatment was up to 97 weeks (median 44) in the current study, and up to 30 weeks in the latter. So, even though the protocol-specified dose constraint to the kidneys differed between the two trials, the total injected activity/patient was similar. There was, however, a large difference in the duration of the treatment period which could theoretically be a reason for the large difference in PFS. In our own material, there is a strong correlation (R2 = 0.9, p < 0.01, data not shown) between cumulative BED and duration of treatment period, so we are not able to differentiate between these two potential explanatory factors for PFS.
The significant differences in PFS when subgrouped by Ki 67, ECOG, and renal BED are challenging to interpret since there are obvious confounders (such as treatment-related toxicity, prognosis, and selection bias). The fact that there was very limited toxicity in the highest BED group, and the poorer results for the patients with the highest Ki 67, would support a strategy in future trials to intensify treatment for the higher grade tumors with the hope of improving outcomes. No significant differences in PFS or OS were seen for different origins; however, pNET patients had a higher Ki 67% than SiNET patients (Table 3). This result has also been reported by others [4] and may reflect that pNETs are more responsive to radiation therapy in general than the more indolent group of SiNETs.
The results of the analysis of PFS and OS by renal BED beg the question of whether more cycles of treatment result in a higher dose to the tumor and thereby a better and more durable response. This question cannot be definitively answered in a nonrandomized setting, but the fact that the time to maximum response also increased by BED level from 12 months (BED < 25 Gy) to 23 and 28 months (BED 25–29 and > 29 Gy, respectively) implies that with increasing number of cycles the tumor shrinkage continues for a longer time.
When designing the trial, we expected a larger proportion of patients to be able to continue treatment in step 2. Sixty patients (62%) were excluded from step 2 because of earlier chemotherapy or liver-directed treatment (Table 1), and 7 patients (7%) were excluded solely based on age > 70 years. Given the limited toxicity noted in this trial, it seems safe to offer treatment beyond the proposed renal dose limits with less restrictive criteria, with the goal of a better long-term effect and survival.
When designing the trial, it had to be decided which renal dose limits to use based on existing evidence. The commonly used renal absorbed dose limit of 23 Gy originates from external beam radiotherapy (EBRT) and is based on delivering 2 Gy fractions at a dose rate of approximately 1 Gy/min, which has a very different biological effect than the dose rate achieved with PRRT. Assuming that the linear-quadratic model is valid for both EBRT and PRRT, 23 Gy given in 2 Gy fractions corresponds to approximately 40 Gy BED, while an absorbed dose of 23 Gy at the typical dose rate of PRRT corresponds to approximately 25 Gy BED (4.5 Gy/cycle, \(\alpha /\beta =2.6\), and repair half-life of 2.8 h assumed) [20]. Furthermore, the renal BED thresholds of 27 and 40 Gy used in the current trial may have been overly conservative, since 90Y-PRRT has a more uniform energy deposition pattern than 177Lu [26], possibly explaining the more pronounced renal toxicity. Renal function did seem to decline slightly during follow-up, however, which will be further studied in an ad hoc analysis with the goal of determining the relevant renal dose limit for 177Lu-PRRT. An important step towards making dosimetry-based treatment generally available is to simplify the imaging procedure on which the dosimetry is based. Single or dual time-point SPECT imaging has been explored by our group and others and found to give reliable dosimetric estimates for the kidneys, especially when the last imaging time-point is at least 72 h after therapy [27,28,29,30,31].
The biological effects of the absorbed radiation dose on tumor lesions and normal tissue in PRRT are likely influenced by several factors governed both by patient (size, renal function, risk factors for toxicity, etc.) and tumor (volume, proliferation rate, intrinsic radiation sensitivity) characteristics. To achieve a truly personalized PRRT, we need to understand which of them have the greatest impact on treatment outcomes and design the treatment accordingly [32]. Regardless of strategy, a personalized approach motivates dosimetry evaluations of organs at risk and ideally of the tumor as well. There are several situations when this information would facilitate treatment decisions, e.g., retreatment with 177Lu-DOTATATE, treatment of patients with reduced kidney function or bone marrow reserve, and intensified treatment to more rapidly progressing tumors, e.g., NET G3 with a Ki 67 labeling index > 20%.
For many patients, the standard regimen of four cycles of 177Lu-DOTATATE will provide valuable responses and survival benefits. The current results confirm that by individualizing the therapeutic approach the response rate can increase considerably, without causing clinically significant acute or late toxicity. This raises the question whether it is still justifiable to treat according to the currently approved, non-individualized regime. It is possible that it leads to a significant proportion of patients being undertreated, exposing them to the much greater threat to their survival than low-grade toxicity, namely tumor progression. Further improvement of the individualized treatment approach may be achieved by offering patients with more aggressive tumors higher intensity treatment, including combinations of PRRT with other systemic anti-cancer therapies, while patients with low-grade tumors continue to receive a therapy with minimal toxicity and impact on their everyday life. Thus, there is currently a high unmet need for well-designed randomized trials in PRRT, through which the risks and benefits of personalized vs. standard therapy can be demonstrated and quantified.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Pavel M, Oberg K, Falconi M, Krenning EP, Sundin A, Perren A, et al. Gastroenteropancreatic neuroendocrine neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(7):844–60.
DelleFave G, O’Toole D, Sundin A, Taal B, Ferolla P, Ramage JK, et al. ENETS Consensus Guidelines update for gastroduodenal neuroendocrine neoplasms. Neuroendocrinology. 2016;103(2):119–24.
Hope TA, Bodei L, Chan JA, El-Haddad G, Fidelman N, Kunz PL, et al. NANETS/SNMMI consensus statement on patient selection and appropriate use of (177)Lu-DOTATATE peptide receptor radionuclide therapy. J Nucl Med. 2020;61(2):222–7.
Brabander T, van der Zwan WA, Teunissen JJM, Kam BLR, Feelders RA, de Herder WW, et al. Long-term efficacy, survival, and safety of [(177)Lu-DOTA(0), Tyr(3)]octreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors. Clin Cancer Res. 2017;23(16):4617–24.
Zhang J, Song Q, Cai L, Xie Y, Chen Y. The efficacy of (177)Lu-DOTATATE peptide receptor radionuclide therapy (PRRT) in patients with metastatic neuroendocrine tumours: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2020;146(6):1533–43.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of (177)Lu-DOTATATE for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125–35.
Stokke C, Gabina PM, Solny P, Cicone F, Sandstrom M, Gleisner KS, et al. Dosimetry-based treatment planning for molecular radiotherapy: a summary of the 2017 report from the Internal Dosimetry Task Force. EJNMMI Phys. 2017;4(1):27.
Okunieff P, Morgan D, Niemierko A, Suit HD. Radiation dose-response of human tumors. Int J Radiat Oncol Biol Phys. 1995;32(4):1227–37.
Strigari L, Konijnenberg M, Chiesa C, Bardies M, Du Y, Gleisner KS, et al. The evidence base for the use of internal dosimetry in the clinical practice of molecular radiotherapy. Eur J Nucl Med Mol Imag. 2014;41(10):1976–88.
Cremonesi M, Ferrari ME, Bodei L, Chiesa C, Sarnelli A, Garibaldi C, et al. Correlation of dose with toxicity and tumour response to (90)Y- and (177)Lu-PRRT provides the basis for optimization through individualized treatment planning. Eur J Nucl Med Mol Imag. 2018;45(13):2426–41.
Otte A, Herrmann R, Heppeler A, Behe M, Jermann E, Powell P, et al. Yttrium-90 DOTATOC: first clinical results. Eur J Nucl Med. 1999;26(11):1439–47.
Bodei L, Cremonesi M, Zoboli S, Grana C, Bartolomei M, Rocca P, et al. Receptor-mediated radionuclide therapy with 90Y-DOTATOC in association with amino acid infusion: a phase I study. Eur J Nucl Med Mol Imag. 2003;30(2):207–16.
Ilan E, Sandstrom M, Wassberg C, Sundin A, Garske-Roman U, Eriksson B, et al. Dose response of pancreatic neuroendocrine tumors treated with peptide receptor radionuclide therapy using 177Lu-DOTATATE. J Nucl Med. 2015;56(2):177–82.
Jahn U, Ilan E, Sandstrom M, Garske-Roman U, Lubberink M, Sundin A. 177Lu-DOTATATE peptide receptor radionuclide therapy: dose response in small intestinal neuroendocrine tumors. Neuroendocrinology. 2020;110(7–8):662–70.
Melis M, Krenning EP, Bernard BF, Barone R, Visser TJ, de Jong M. Localisation and mechanism of renal retention of radiolabelled somatostatin analogues. Eur J Nucl Med Mol Imag. 2005;32(10):1136–43.
Rolleman EJ, Valkema R, de Jong M, Kooij PP, Krenning EP. Safe and effective inhibition of renal uptake of radiolabelled octreotide by a combination of lysine and arginine. Eur J Nucl Med Mol Imag. 2003;30(1):9–15.
Bodei L, Cremonesi M, Ferrari M, Pacifici M, Grana CM, Bartolomei M, et al. Long-term evaluation of renal toxicity after peptide receptor radionuclide therapy with 90Y-DOTATOC and 177Lu-DOTATATE: the role of associated risk factors. Eur J Nucl Med Mol Imag. 2008;35(10):1847–56.
Barone R, Borson-Chazot F, Valkema R, Walrand S, Chauvin F, Gogou L, et al. Patient-specific dosimetry in predicting renal toxicity with (90)Y-DOTATOC: relevance of kidney volume and dose rate in finding a dose-effect relationship. JNuclMed. 2005;46(Suppl 1):99S-106S.
Valkema R, Pauwels SA, Kvols LK, Kwekkeboom DJ, Jamar F, de Jong M, et al. Long-term follow-up of renal function after peptide receptor radiation therapy with (90)Y-DOTA(0), Tyr(3)-octreotide and (177)Lu-DOTA(0), Tyr(3)-octreotate. J Nucl Med. 2005;46(Suppl 1):83S-91S.
Sundlov A, Sjogreen-Gleisner K, Svensson J, Ljungberg M, Olsson T, Bernhardt P, et al. Individualised (177)Lu-DOTATATE treatment of neuroendocrine tumours based on kidney dosimetry. Eur J Nucl Med Mol Imag. 2017;44(9):1480–9.
R Development Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2010.
Hagmarker L, Svensson J, Ryden T, van Essen M, Sundlov A, Gleisner KS, et al. Bone marrow absorbed doses and correlations with hematologic response during (177)Lu-DOTATATE treatments are influenced by image-based dosimetry method and presence of skeletal metastases. J Nucl Med. 2019;60(10):1406–13.
Ramage J, Naraev BG, Halfdanarson TR. Peptide receptor radionuclide therapy for patients with advanced pancreatic neuroendocrine tumors. Semin Oncol. 2018;45(4):246–8.
Garske-Roman U, Sandstrom M, Fross Baron K, Lundin L, Hellman P, Welin S, et al. Prospective observational study of (177)Lu-DOTA-octreotate therapy in 200 patients with advanced metastasized neuroendocrine tumours (NETs): feasibility and impact of a dosimetry-guided study protocol on outcome and toxicity. Eur J Nucl Med Mol Imag. 2018;45(6):970–88.
Del Prete M, Buteau FA, Arsenault F, Saighi N, Bouchard LO, Beaulieu A, et al. Personalized (177)Lu-octreotate peptide receptor radionuclide therapy of neuroendocrine tumours: initial results from the P-PRRT trial. Eur J Nucl Med Mol Imag. 2019;46(3):728–42.
Konijnenberg M, Melis M, Valkema R, Krenning E, de Jong M. Radiation dose distribution in human kidneys by octreotides in peptide receptor radionuclide therapy. J Nucl Med. 2007;48(1):134–42.
Sundlov A, Gustafsson J, Brolin G, Mortensen N, Hermann R, Bernhardt P, et al. Feasibility of simplifying renal dosimetry in (177)Lu peptide receptor radionuclide therapy. EJNMMI Phys. 2018;5(1):12.
Freedman N, Sandstrom M, Kuten J, Shtraus N, Ospovat I, Schlocker A, et al. Personalized radiation dosimetry for PRRT-how many scans are really required? EJNMMI Phys. 2020;7(1):26.
Chicheportiche A, Ben-Haim S, Grozinsky-Glasberg S, Oleinikov K, Meirovitz A, Gross DJ, et al. Dosimetry after peptide receptor radionuclide therapy: impact of reduced number of post-treatment studies on absorbed dose calculation and on patient management. EJNMMI Phys. 2020;7(1):5.
Willowson KP, Eslick E, Ryu H, Poon A, Bernard EJ, Bailey DL. Feasibility and accuracy of single time point imaging for renal dosimetry following (177)Lu-DOTATATE (‘Lutate’) therapy. EJNMMI Phys. 2018;5(1):33.
Hanscheid H, Lapa C, Buck AK, Lassmann M, Werner RA. Dose mapping after endoradiotherapy with (177)Lu-DOTATATE/DOTATOC by a single measurement after 4 days. J Nucl Med. 2017;59(1):75–81.
Svensson J, Berg G, Wangberg B, Larsson M, Forssell-Aronsson E, Bernhardt P. Renal function affects absorbed dose to the kidneys and haematological toxicity during (1)(7)(7)Lu-DOTATATE treatment. Eur J Nucl Med Mol Imag. 2015;42(6):947–55.
Acknowledgements
This trial has been carried out with the generous support of Skåne and Sahlgrenska University Hospitals. We would especially like to acknowledge the support of technologists Nadja Mortensen and Rebecca Hermann, research nurse Charlotte Fogelström, statistician Andrea Dahl Sturedahl, physicists Cecilia Hindorf and Erik Larsson, and oncologist Pernilla Asp, without whom this trial could not have been carried out.
Funding
Open access funding provided by University of Gothenburg. Generous support has been granted by the Mrs. Berta Kamprad’s Foundation, (FBKS-2019–44-270, 2020–8-270, and 2020–13-293), Gunnar Nilssons Cancer Foundation (GN 2020-16-173), the Swedish Cancer Society (CAN 2015/266, 2018/577, 2018/747 and 2021/1754), the King Gustav V Jubilee Clinic Cancer Research Foundation (2020:309), the ALF-agreement (ALFGBG-723481), and the Swedish Research Council (2018-05098VR).
Author information
Authors and Affiliations
Contributions
Conception and design: AS, JT, JS, KSG, ML, PB
Administrative support: AS, KH
Provision of study material or patients: AH, AS, CFW, JS, JT
Data analysis and interpretation: AH, AS, CFW, KSG, JS, JT, PB
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
Corresponding author
Ethics declarations
Ethics approval
The trial was conducted in accordance with ICH GCP and the Declaration of Helsinki and was approved by the regional ethics review board (EPN Lund 2011/287).
Consent to participate
Informed consent was obtained from all participants in this trial.
Consent for publication
All authors agree with the submitted version of the manuscript. The material submitted for publication has not been previously reported and is not under consideration for publication elsewhere.
Competing interests
Anna Sundlöv declares having received speaker honoraria from Novartis, Ipsen, and Sam Nordic, advisory board fees from Advanced Accelerator Applications, and consultancy fees from Spago Nanomedical.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology—General.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sundlöv, A., Gleisner, K., Tennvall, J. et al. Phase II trial demonstrates the efficacy and safety of individualized, dosimetry-based 177Lu-DOTATATE treatment of NET patients. Eur J Nucl Med Mol Imaging 49, 3830–3840 (2022). https://doi.org/10.1007/s00259-022-05786-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-022-05786-w