Abstract
Purpose
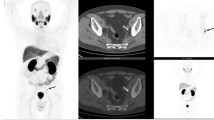
Binding of 68Ga-PSMA-HBED-CC (68Ga-PSMA) at prostate cancer (PC) cells increases over time. A biphasic protocol may help separating benign from tumor lesions. The aim of this study was the retrospective evaluation of a diagnostic incremental value of a dual-time point (biphasic) 68Ga-PSMA-PET/CT in patients with prostate cancer.
Methods
Retrospective analysis of 35 consecutive patients (49–78 years, median 71) with newly diagnosed PC (12/35) or recurrence of PC (23/35). PET/CT (Gemini TF16, Philips) was acquired 1 h and 3 h p. i. of 140–392 MBq (300 MBq median) 68Ga-PSMA, followed by a diagnostic contrast CT. PET findings were correlated with histology or unequivocal CT findings. Semiquantitative PET data (SUVmax, SUV mean) were acquired and target-to-background-ratios (T/B-ratio) were calculated for benign and malign lesions for both time points. Size of lymph nodes (LN) on diagnostic CT was recorded. Statistical analysis was performed for assessment of significant changes of semiquantitative PET-parameters over time and for correlation of size and uptake of lymph nodes.
Results
One hundred and four lesions were evaluated. Sixty lesions were referenced by histology or unequivocal CT findings, including eight (13.3 %) histopathologically benign lymph nodes, 12 (20 %) histopathologically lymph node metastases, 12 (20 %) primary tumors, three (5 %) local recurrences, and 25 (41.7 %) bone metastases. Forty-four lesions were axillary LN with normal CT-appearance. Benign lesions had significantly lower SUVmax and T/B-ratios compared with malignant findings. Malign lesions showed a significant increase of both parameters over time compared to benign findings. There was no correlation between LN size and SUVmax. The sensitivity, specificity, the positive predictive value and negative predictive value of PET/CT regarding pelvic LN was 94 %, 99 %, 89 %, and 99.5 %, respectively.
Conclusions
In contrast to benign tissues, the uptake of proven tumor lesions increases on 68Ga-PSMA-PET/CT over time. A biphasic PET-study may lead to a better detection of tumor lesions in unequivocal findings.


Similar content being viewed by others
References
Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol. 2012;61(6):1079–92.
Ward JF, Blute ML, Slezak J, Bergstralh EJ, Zincke H. The long-term clinical impact of biochemical recurrence of prostate cancer 5 or more years after radical prostatectomy. J Urol. 2003;170:1872–6.
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, et al. Comparison of PET imaging with a (68)Ga-labelled PSMA ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41(1):11–20. doi:10.1007/s00259-013-2525-5.
Zhuang H, Pourdehnad M, Lambright ES, Yamamoto AJ, Lanuti M, Li P, et al. Dual time point 18F-FDG PET imaging for differentiating malignant from inflammatory processes. J Nucl Med. 2001;42(9):1412–7.
Alkhawaldeh K, Bural G, Kumar R, Alavi A. Impact of dual-time-point (18)F-FDG PET imaging and partial volume correction in the assessment of solitary pulmonary nodules. Eur J Nucl Med Mol Imaging. 2008;35(2):246–52.
Sahlmann CO, Siefker U, Lehmann K, Meller J. Dual time point 2-[18F]fluoro-2'-deoxyglucose positron emission tomography in chronic bacterial osteomyelitis. Nucl Med Commun. 2004;25(8):819–23.
Schottelius M, Šimeček J, Hoffmann F, Willibald M, Schwaiger M, Wester HJ. Twins in spirit - episode I: comparative preclinical evaluation of [(68)Ga]DOTATATE and [(68)Ga]HA-DOTATATE. EJNMMI Res. 2015;5:22.
Meller B, Meller J, Sahlmann CO, Hijazi S, Trojan L, Thelen P. V52 Medikamentöse Beeinflussung der Aufnahme von F-18-Flormethylcholin (FMC) und Ga-68-PSMAHEBD sowie der prostataspezifischen Membranantigen (PSMA)-mRNAExpression in In-vitro-Modellen des Prostatakarzinoms (PC). Nuklearmedizin. 2014;53(1):A2–109.
Rajasekaran SA, Anilkumar G, Oshima E, Bowie JU, Liu H, Heston W, et al. A novel cytoplasmic tail MXXXL motif mediates the internalization of prostate-specific membrane antigen. Mol Biol Cell. 2003;14(12):4835–45.
Martin R, Juttler S, Muller M, Wester HJ. Cationic eluate pretreatment for automated synthesis of [(6)(8)Ga]CPCR4.2. Nucl Med Biol. 2014;41:84–9.
Eder M, Schafer M, Bauder-Wust U, Hull WE, Wangler C, Mier W, et al. 68Ga-complex lipophilicity and the targeting property of a urea-based PSMA inhibitor for PET imaging. Bioconjug Chem. 2012;23:688–97.
Bouchelouche K, Choyke PL, Capala J. Prostate specific membrane antigen a target for imaging and therapy with radionuclides. Discov Med. 2010;9:55–61.
Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, et al. Evaluation of Hybrid 68Ga-PSMA Ligand PET/CT in 248 Patients with Biochemical Recurrence After Radical Prostatectomy. J Nucl Med. 2015;56(5):668–74.
Hijazi S, Meller B, Leitsmann C, Strauss A, Meller J, Ritter CO, et al. Pelvic lymph node dissection for nodal oligometastatic prostate cancer detected by (68) Ga-PSMA-positron emission tomography/computerized tomography. Prostate. 2015. doi:10.1002/pros.23091.
Eder M, Neels O, Muller M, Bauder-Wust U, Remde Y, Schafer M, et al. Novel Preclinical and Radiopharmaceutical Aspects of [68Ga]Ga-PSMA-HBED-CC: A New PET Tracer for Imaging of Prostate Cancer. Pharmaceuticals. 2014;7:779–96.
Conti M. New prospects for PET in prostate cancer imaging: a physicist's viewpoint. EJNMMI Physics. 2014;1:11.
Kadrmas DJ, Casey ME, Conti M, Jakoby BW, Lois C, Townsend DW. Impact of time-of-flight on PET tumor detection. J Nucl Med. 2009;50:1315–23.
Krohn T, Verburg FA, Pufe T, Neuhuber W, Vogg A, Heinzel A, et al. [(68)Ga]PSMA-HBED uptake mimicking lymph node metastasis in coeliac ganglia: an important pitfall in clinical practice. Eur J Nucl Med Mol Imaging. 2015;42(2):210–4.
Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, et al. The diagnostic value of PET/CT imaging with the 68Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:197–209.
Weineisen M, Schottelius M, Simecek J, Baum RP, Yildiz A, Beykan S, et al. 68Ga- and 177Lu-labeled PSMA I&T: Optimization of a PSMA targeted theranostic concept and first proof of concept human studies. J Nucl Med. 2015;56(8):1169–76.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40(4):486–95. doi:10.1007/s00259-012-2298-2.
Schwarzenböck S, Souvatzoglou M, Krause BJ. Choline PET and PET/CT in Primary Diagnosis and Staging of Prostate Cancer. Theranostics. 2012;2(3):318–30. doi:10.7150/thno.4008.
Dietlein M, Kobe C, Kuhnert G, Stockter S, Fischer T, Schomäcker K, et al. Comparison of [(18)F]DCFPyL and [ (68)Ga]Ga-PSMA-HBED-CC for PSMA-PET Imaging in Patients with Relapsed Prostate Cancer. Mol Imaging Biol. 2015;17(4):575–84.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Carsten-Oliver Sahlmann declares that he has no conflict of interest. Birgit Meller declares that she has no conflict of interest. Caroline Bouter declares that she has no conflict of interest. Christian Oliver Ritter declares that he has no conflict of interest. Philipp Ströbel declares that he has no conflict of interest. Joachim Lotz declares that he has no conflict of interest. Lutz Trojan declares that he has no conflict of interest. Johannes Meller declares that he has no conflict of interest. Sameh Hijazi declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Sahlmann, CO., Meller, B., Bouter, C. et al. Biphasic 68Ga-PSMA-HBED-CC-PET/CT in patients with recurrent and high-risk prostate carcinoma. Eur J Nucl Med Mol Imaging 43, 898–905 (2016). https://doi.org/10.1007/s00259-015-3251-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-015-3251-y