Abstract
Purpose
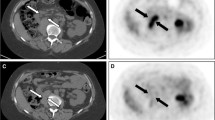
The different stages in idiopathic retroperitoneal fibrosis (IRF) are generally assessed by assay of inflammatory markers and analysis of contrast-enhanced CT images of the retroperitoneal mass. We investigated the potential role of 18F-FDG PET/CT in this clinical setting.
Methods
18F-FDG uptake was assessed visually and semiquantitatively (using maximum standardized uptake values, SUVmax) in images of the abdominal mass in 22 patients prospectively enrolled from June 2008 to December 2010 who underwent a total of 33 PET/CT studies. The accuracy in discriminating active from inactive disease was calculated assuming as reference a biochemical instrumental evaluation of patients with IRF mostly based on the level of inflammatory indices and contrast enhancement (CE) of the mass at the time of each PET study. In particular, the relationship between SUVmax and CE, the latter calculated from the change in radiodensity (Hounsfield units) between the basal and postcontrast venous portal phases, was evaluated on a three-point scale (0 <20 HU, 1 20–30 HU, 2 ≥30 HU). SUVmax and CE scores were correlated with the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels. The value of PET/CT in assessing the variation of disease activity over time was also investigated by analysing the changes in metabolic volume (MV) of the retroperitoneal lesion between repeat patient studies.
Results
PET/CT accurately discriminated (93.9 %) active from inactive disease. Significant agreement (p < 0.01) was observed between visual and semiquantitative analysis of 18F-FDG uptake, and CE score. A significant correlation (p < 0.01) was found among SUVmax, CRP levels (rho = 0.54) and ESR (rho = 0.55). Corresponding variations in MV and CE score were observed in patients with multiple studies (p < 0.01; rho = 0.68).
Conclusion
18F-FDG PET/CT may be considered an alternative imaging method for the assessment of different stages of IRF.







Similar content being viewed by others
References
Gilkeson GS, Allen NB. Retroperitoneal fibrosis. A true connective tissue disease. Rheum Dis Clin North Am. 1996;22:23–38.
Moroni G, Dore R, Collini P. Idiopathic retroperitoneal fibrosis. J Nephrol. 2005;18:794–808.
Magrey MN, Husni ME, Kushner I, Calabrese LH. Do acute-phase reactants predict response to glucocorticoid therapy in retroperitoneal fibrosis? Arthritis Rheum. 2009;61:674–9.
Moroni G, Gallelli B, Banfi G, Sandri S, Messa P, Ponticelli C. Long-term outcome of idiopathic retroperitoneal fibrosis treated with surgical and/or medical approaches. Nephrol Dial Transplant. 2006;21:2485–90.
Kamper L, Brandt AS, Scharwächter C, Kukuk S, Roth S, Haage P, et al. MR evaluation of retroperitoneal fibrosis. Rofo. 2011;183:721–6.
Burn PR, Singh S, Barbur S, Boustead G, King CM. Role of gadolinium-enhanced magnetic resonance imaging in retroperitoneal fibrosis. Can Assoc Radiol J. 2002;53:168–70.
Yuh WT, Barloon TJ, Sickels WJ, Kramolowsky EV, Williams RD. Magnetic resonance imaging in the diagnosis and follow-up of idiopathic retroperitoneal fibrosis. J Urol. 1989;141:602–5.
Cavalcanti Filho JL, de Souza Leão Lima R, de Souza Machado Neto L, Kayat Bittencourt L, Domingues RC, da Fonseca LM. PET/CT and vascular disease: current concepts. Eur J Radiol. 2011;80:60–7.
Vaglio A, Greco P, Versari A, Filice A, Cobelli R, Manenti L, et al. Post-treatment residual tissue in idiopathic retroperitoneal fibrosis: active residual disease or silent "scar"? A study using 18F-fluorodeoxyglucose positron emission tomography. Clin Exp Rheumatol. 2005;23:231–4.
Pipitone N, Ghinoi A, Versari A, Vaglio A, Palmisano A, Salvarani C. Images in cardiovascular medicine. Chronic periaortitis. Circulation. 2008;118:1214–6.
Papathanasiou ND, Du Y, Menezes LJ, Al-Muhaideb A, Shastry M, Beynon H, et al. 18F-Fluorodeoxyglucose PET/CT in the evaluation of large-vessel vasculitis: diagnostic performance and correlation with clinical and laboratory parameters. Br J Radiol. 2011. doi:10.1259/bjr/16422950.
Nakajo M, Jinnouchi S, Tanabe H, Tateno R, Nakajo M. 18F-fluorodeoxyglucose positron emission tomography features of idiopathic retroperitoneal fibrosis. J Comput Assist Tomogr. 2007;31:539–43.
Cronin CG, Lohan DG, Blake MA, Roche C, McCarthy P, Murphy JM. Retroperitoneal fibrosis: a review of clinical features and imaging findings. AJR Am J Roentgenol. 2008;191:423–31.
Jansen I, Hendriksz TR, Han SH, Huiskes AW, van Bommel EF. (18)F-fluorodeoxyglucose position emission tomography (FDG-PET) for monitoring disease activity and treatment response in idiopathic retroperitoneal fibrosis. Eur J Intern Med. 2010;21:216–21.
Chander S, Ergun EL, Chugani HT, Chugani DC, Juhasz C, Shields AF, et al. High 2-deoxy-2-18F-fluoro-D-glucose accumulation in a case of retroperitoneal fibrosis following resection of carcinoid tumor. Mol Imaging Biol. 2002;4:363–8.
Vaglio A, Versari A, Fraternali A, Ferrozzi F, Salvarani C, Buzio C. 18F-Fluorodeoxyglucose positron emission tomography in the diagnosis and follow up of idiopathic retroperitoneal fibrosis. Arthritis Rheum. 2005;53:122–5.
Takahashi M, Momose T, Kameyama M, Ohtomo K. Abnormal accumulation of 18F-fluorodeoxyglucose in the aortic wall related to inflammatory changes: three case reports. Ann Nucl Med. 2006;20:361–4.
Sakamoto A, Okamoto K, Ishizaka N, Tejima K, Hirata Y, Nagai R. 18F-Fluorodeoxyglucose positron emission tomography in a case of retroperitoneal fibrosis. Int Heart J. 2006;47:645–50.
Young PM, Peterson JJ, Calamia KT. Hypermetabolic activity in patients with active retroperitoneal fibrosis on F-18 FDG PET: report of three cases. Ann Nucl Med. 2008;22:87–92.
Washino S, Hirai M, Matsuzaki A, Kobayashi Y. 18F-Fluorodeoxyglucose positron emission tomography for diagnosis and monitoring of idiopathic retroperitoneal fibrosis associated with mediastinal fibrosis. Ann Nucl Med. 2010;24:225–9.
Palmisano A, Vaglio A. Chronic periaortitis: a fibro-inflammatory disorder. Best Pract Res Clin Rheumatol. 2009;23:339–53.
Salvarani C, Pipitone N, Versari A, Vaglio A, Serafini D, Bajocchi G, et al. Positron emission tomography (PET): evaluation of chronic periaortitis. Arthritis Rheum. 2005;53:298–303.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moroni, G., Castellani, M., Balzani, A. et al. The value of 18F-FDG PET/CT in the assessment of active idiopathic retroperitoneal fibrosis. Eur J Nucl Med Mol Imaging 39, 1635–1642 (2012). https://doi.org/10.1007/s00259-012-2144-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-012-2144-6