Abstract
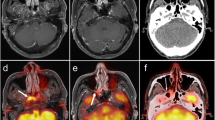
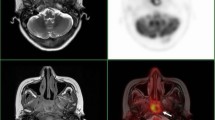
The patterns of nodal spread of nasopharyngeal carcinoma (NPC) have an important influence on treatment planning, but have not yet been fully addressed. We prospectively used MRI and FDG PET to document the patterns of nodal spread in NPC. One hundred and one patients with newly diagnosed NPC were studied with MRI and FDG PET. On MRI, nodes were considered as metastatic according to criteria regarding size, the presence of nodal necrosis, and extracapsular spread. FDG PET images were interpreted visually, and nodes were considered metastatic if they showed prominent FDG uptake against the background. Nodal metastases were found in 89 of our 101 patients. Analysis of the distributions of nodal metastases in these 89 patients showed that retropharyngeal nodes were less frequently involved than cervical nodes (82.0% vs 95.5%). The vast majority of cervical nodal metastases were to the internal jugular chain, including nodes at levels II, III, and IV, with decreasing incidences of 95.5%, 60.7%, and 34.8%, respectively. Level V nodal involvement was found in 27% of patients. Supraclavicular fossa nodal metastases were not uncommon and occurred in 22.5% of patients. Skip metastases in the lower-level nodes or supraclavicular fossa nodes occurred in 7.9% of patients. Mediastinal and abdominal metastatic adenopathy was present in 4.5% and 3.4% of patients, respectively, and was associated with advanced nodal metastasis in the supraclavicular fossa. Level VI (2.2%), level VII (1.1%), submandibular (2.2%), and parotid (3.4%) nodal metastases were uncommon and were always associated with advanced ipsilateral nodal metastases of the neck. We conclude that the combined use of FDG PET and MRI can comprehensively depict the pattern of nodal metastasis in NPC patients. Nodal metastases principally affected level II nodes, from which lymphatic spread extended down in an orderly manner to involve level III, level IV, and the supraclavicular fossa nodes, or extended posteriorly to involve level V nodes. The frequency of skip metastases was 7.9%. Distant spread to mediastinal or abdominal nodes was found in 3–5% of patients, usually in association with supraclavicular nodal metastases.






Similar content being viewed by others
References
Vokes EE, Liebowitz DN, Weichselbaum RR. Nasopharyngeal carcinoma. Lancet 1997; 350:1087–1091.
Huang DP. Epidemiology and aetiology. In: Hasselt CAV, Gibb AG, eds. Nasopharyngeal carcinoma. Hong Kong: The Chinese University Press; 1991:23.
Olmi P, Fallai C, Colagrande S, Giannardi G. Staging and follow up of nasopharyngeal carcinoma: magnetic resonance imaging versus computerized tomography. Int J Radiat Oncol Biol Phys 1995; 32:795–800.
Ng SH, Wan YL, Ko SF, Chang JT. MRI of nasopharyngeal carcinoma with emphasis on relationship to radiotherapy. JMRI 1998; 8:327–336.
Ng SH, Chang JT, Ko SF, Wan YL, Tang LM, WC Chen. MRI in recurrent nasopharyngeal carcinoma. Neuroradiology 1999; 41:855–862.
Ng SH, Chang TC, Ko SF, Yen PS, Wan YL, Tang LM, Tsai MH. Nasopharyngeal carcinoma: MRI and CT assessment. Neuroradiology 1997; 39:741–746.
King AD, Ahuja AT, Leung SF, et al. Neck node metastases from nasopharyngeal carcinoma: MRI of patterns of disease. Head Neck 2000; 22:275–281.
van den Brekel MW, Stel HV, Castelijns JA, et al. Cervical lymph node metastasis: assessment of radiologic criteria. Radiology 1990; 177:379–384.
Chong VF, Fan YF, Khoo JB. Retropharyngeal lymphadenopathy in nasopharyngeal carcinoma. Eur J Radiol 1995; 21:100–105.
Kao CH, Hsieh JF, Tsai SC, et al. Comparison of18F-2-fluoro-2-deoxyglucose positron emission tomography and computed tomography in detection of cervical lymph node metastases of nasopharyngeal carcinoma. Ann Otol Rhinol Laryngol 2000; 109:1130–1134.
Rege S, Maass A, Haiken L, et al. Use of positron emission tomography with fluoro-deoxyglucose in patients with extracranial head and neck cancers. Cancer 1997; 73:3047–3058.
Nishioka T, Shiga T, Shirato H, et al. Image fusion between18FDG-PET and MRI/CT for radiotherapy planning of oropharyngeal and nasopharyngeal carcinomas. Int J Radiat Oncol Biol Phys 2002; 53:1052–1057.
Adams S, Baum RP, Stuckensen T, et al. Prospective comparison of18F-FDG PET with conventional imaging modalities (CT, MRI, US) in lymph node staging of head and neck cancer. Eur J Nucl Med 1998; 25:1255–1260.
Kau RJ, Alexiou C, Laubenbacher C, Werner M, Schwaiger M, Arnold W. Lymph node detection of head and neck squamous cell carcinomas by positron emission tomography with fluorodeoxy-glucose F 18 in a routine clinical setting. Arch Otolaryngol Head Neck Surg 1999; 125:1322–1328.
Kostakoglu L, Agress H, Goldsmith S. Clinical role of FDG PET in evaluation of cancer patients. Radiographics 2003; 33:315–340.
Som PM, Curtin HD, Mancuso AA. Imaging-based nodal classification for evaluation of neck metastatic adenopathy. AJR 2000; 174:837–844.
Sham JST, Choy D, Wei WI. Nasopharyngeal carcinoma: orderly neck node spread. Int J Radiat Oncol Biol Phys 1990; 19:929–933.
Wakisaka M, Mori H, Fuwa N, Matsumoto A. MR analysis of nasopharyngeal carcinoma: correlation of the pattern of tumor extent at the primary site with the distribution of metastasized cervical lymph nodes. Preliminary results. Eur Radiol 2000; 10:970–977.
Lindberg R. Distribution of cervical lymph nodes metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer 1972; 29:1446–1449.
Sham JST, Cheung YK, Choy D, Chan FL, Leong L. Computed tomography evaluation of neck node metastases from nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 1993; 26:787–792.
Acknowledgements
This work was supported by grants NSC 92-2314-B-182A-081 from the National Science Council, Taiwan and CMRPG32034 from the Chang Gung Memorial Hospital and University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ng, SH., Chang, J.TC., Chan, SC. et al. Nodal metastases of nasopharyngeal carcinoma: patterns of disease on MRI and FDG PET. Eur J Nucl Med Mol Imaging 31, 1073–1080 (2004). https://doi.org/10.1007/s00259-004-1498-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-004-1498-9