Abstract
Objective
To evaluate association of fatty infiltration in paraspinal musculature with clinical outcomes in patients suffering from lumbar spinal stenosis (LSS) using qualitative and quantitative grading in magnetic resonance imaging (MRI).
Materials and methods
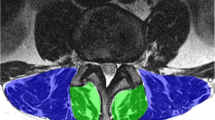
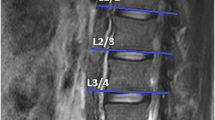
In this retrospective study, texture analysis (TA) was performed on postprocessed axial T2 weighted (w) MR images at level L3/4 using dedicated software (MaZda) in 62 patients with LSS. Associations in fatty infiltration between qualitative Goutallier and quantitative TA findings with two clinical outcome measures, Spinal stenosis measure (SSM) score and walking distance, at baseline and regarding change over time were assessed using machine learning algorithms and multiple logistic regression models.
Results
Quantitative assessment of fatty infiltration using the histogram TA feature “mean” showed higher interreader reliability (ICC 0.83–0.97) compared to the Goutallier staging (κ = 0.69–0.93). No correlation between Goutallier staging and clinical outcome measures was observed. Among 151 TA features, only TA feature “mean” of the spinotransverse group showed a significant but weak correlation with worsened SSM (p = 0.046). TA feature “S(3,3) entropy” showed a significant but weak association with worsened WD over 12 months (p = 0.046).
Conclusion
MR TA is a reproducible tool to quantitatively assess paraspinal fatty infiltration, but there is no clear association with the clinical outcome in asymptomatic LSS patients.



Similar content being viewed by others
Abbreviations
- CSA:
-
cross-sectional surface area
- FID:
-
free induction decay
- GLCM:
-
gray level co-occurrence
- ICC:
-
intraclass correlation coefficients
- ROC:
-
receiver operating characteristic
- TSE:
-
turbo spin echo
- w:
-
weighted
- AUC:
-
area under the curve
- BMI:
-
body mass index
- LSOS:
-
Lumbar Stenosis Outcome Study
- LSS:
-
lumbar spinal stenosis
- MRI:
-
magnetic resonance imaging
- ROI:
-
regions of interest
- SSM:
-
spinal stenosis measure
- TA:
-
texture analysis
- WD:
-
walking distance
References
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303(13):1259–65.
Waddell G. Low back pain: a twentieth century health care enigma. Spine (Phila Pa 1976). 1996;21(24):2820–5.
Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016;352:h6234.
Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15 Suppl 2:S192–300.
Savage RA, Whitehouse GH, Roberts N. The relationship between the magnetic resonance imaging appearance of the lumbar spine and low back pain, age and occupation in males. Eur Spine J. 1997;6(2):106–14.
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–6.
Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine (Phila Pa 1976). 2000;25(7):819–28.
Rantanen J, Hurme M, Falck B, Alaranta H, Nykvist F, Lehto M, et al. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 1993;18(5):568–74.
Leinonen V, Maatta S, Taimela S, Herno A, Kankaanpaa M, Partanen J, et al. Impaired lumbar movement perception in association with postural stability and motor- and somatosensory-evoked potentials in lumbar spinal stenosis. Spine (Phila Pa 1976). 2002;27(9):975–83.
Sebro R, O’Brien L, Torriani M, Bredella MA. Assessment of trunk muscle density using CT and its association with degenerative disc and facet joint disease of the lumbar spine. Skelet Radiol. 2016;45(9):1221–6.
Kalichman L, Hodges P, Li L, Guermazi A, Hunter DJ. Changes in paraspinal muscles and their association with low back pain and spinal degeneration: CT study. Eur Spine J. 2010;19(7):1136–44.
Keller A, Gunderson R, Reikeras O, Brox JI. Reliability of computed tomography measurements of paraspinal muscle cross-sectional area and density in patients with chronic low back pain. Spine (Phila Pa 1976). 2003;28(13):1455–60.
Winklhofer S, Held U, Burgstaller JM, Finkenstaedt T, Bolog N, Ulrich N, et al. Degenerative lumbar spinal canal stenosis: intra- and inter-reader agreement for magnetic resonance imaging parameters. Eur Spine J. 2017;26(2):353–61.
Betz M, Burgstaller JM, Held U, Andreisek G, Steurer J, Porchet F, et al. Influence of paravertebral muscle quality on treatment efficacy of epidural steroid infiltration or surgical decompression in lumbar spinal stenosis: analysis of the Lumbar Spinal Outcome Study (LSOS) data—a Swiss prospective multi-center cohort study. Spine (Phila Pa 1976). 2017;42(23):1792–8. https://doi.org/10.1097/BRS.0000000000002233.
Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278(2):563–77.
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Carvalho S, et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun. 2014;5:4006.
Sogawa K, Nodera H, Takamatsu N, Mori A, Yamazaki H, Shimatani Y, et al. Neurogenic and myogenic diseases: quantitative texture analysis of muscle US data for differentiation. Radiology. 2017;160826
Hainc N, Stippich C, Stieltjes B, Leu S, Bink A. Experimental texture analysis in glioblastoma: a methodological study. Invest Radiol. 2017;52(6):367–73.
Ingrisch M, Schneider MJ, Norenberg D. Negrao de Figueiredo G, Maier-Hein K, Suchorska B, et al. Radiomic analysis reveals prognostic information in T1-weighted baseline magnetic resonance imaging in patients with glioblastoma. Invest Radiol. 2017;52(6):360–6.
Hwang IP, Park CM, Park SJ, Lee SM, McAdams HP, Jeon YK, et al. Persistent pure ground-glass nodules larger than 5 mm: differentiation of invasive pulmonary adenocarcinomas from Preinvasive lesions or minimally invasive adenocarcinomas using texture analysis. Invest Radiol. 2015;50(11):798–804.
Pickles MD, Lowry M, Gibbs P. Pretreatment prognostic value of dynamic contrast-enhanced magnetic resonance imaging vascular, texture, shape, and size parameters compared with traditional survival indicators obtained from locally advanced breast cancer patients. Invest Radiol. 2016;51(3):177–85.
Rachidi M, Marchadier A, Gadois C, Lespessailles E, Chappard C, Benhamou CL. Laws’ masks descriptors applied to bone texture analysis: an innovative and discriminant tool in osteoporosis. Skelet Radiol. 2008;37(6):541–8.
Hofmann FC, Neumann J, Heilmeier U, Joseph GB, Nevitt MC, McCulloch CE, et al. Conservatively treated knee injury is associated with knee cartilage matrix degeneration measured with MRI-based T2 relaxation times: data from the osteoarthritis initiative. Skelet Radiol. 2018;47(1):93–106.
Ulrich NH, Burgstaller JM, Held U, Winklhofer S, Farshad M, Pichierri G, et al. The influence of single-level versus multilevel decompression on the outcome in multisegmental lumbar spinal stenosis: analysis of the lumbar spinal outcome study (LSOS) data. Clin Spine Surg. 2017;Dec;30(10):E1367–75.
Aichmair A, Burgstaller JM, Schwenkglenks M, Steurer J, Porchet F, Brunner F, et al. Cost-effectiveness of conservative versus surgical treatment strategies of lumbar spinal stenosis in the Swiss setting: analysis of the prospective multicenter lumbar stenosis outcome study (LSOS). Eur Spine J. 2017;26(2):501–9.
Burgstaller JM, Schuffler PJ, Buhmann JM, Andreisek G, Winklhofer S, Del Grande F, et al. Is there an association between pain and magnetic resonance imaging parameters in patients with lumbar spinal stenosis? Spine (Phila Pa 1976). 2016;41(17):E1053–62.
Bresnahan LE, Smith JS, Ogden AT, Quinn S, Cybulski GR, Simonian N, et al. Assessment of paraspinal muscle cross-sectional area following lumbar decompression: minimally invasive versus open approaches. Clin Spine Surg. 2017;30(3):E162–68.
Stucki G, Liang MH, Fossel AH, Katz JN. Relative responsiveness of condition-specific and generic health status measures in degenerative lumbar spinal stenosis. J Clin Epidemiol. 1995;48(11):1369–78.
Stucki G, Daltroy L, Liang MH, Lipson SJ, Fossel AH, Katz JN. Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine (Phila Pa 1976). 1996;21(7):796–803.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83.
Battaglia PJ, Maeda Y, Welk A, Hough B, Kettner N. Reliability of the Goutallier classification in quantifying muscle fatty degeneration in the lumbar multifidus using magnetic resonance imaging. J Manip Physiol Ther. 2014;37(3):190–7.
Crawford RJ, Cornwall J, Abbott R, Elliott JM. Manually defining regions of interest when quantifying paravertebral muscles fatty infiltration from axial magnetic resonance imaging: a proposed method for the lumbar spine with anatomical cross-reference. BMC Musculoskelet Disord. 2017;18(1):25.
Szczypinski PM, Strzelecki M, Materka A, Klepaczko A. MaZda: a software package for image texture analysis. Comput Methods Prog Biomed. 2009;94(1):66–76.
Collewet G, Strzelecki M, Mariette F. Influence of MRI acquisition protocols and image intensity normalization methods on texture classification. Magn Reson Imaging. 2004;22(1):81–91.
Tabari A, Torriani M, Miller KK, Klibanski A, Kalra MK, Bredella MA. Anorexia nervosa: analysis of trabecular texture with CT. Radiology. 2016;160970
Kursa MB, Rudnicki WR. Feature selection with the Boruta package. J Stat Softw. 2010;36(11):1–13.
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37–46.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69–71.
Aggarwal N, Agrawal RK. First and second order statistics features for classification of magnetic resonance brain images. J Signal Inf Proces. 2012;3(2):146–53.
Park MJ, Cho JM, Jeon KN, Bae KS, Kim HC, Choi DS, et al. Mass and fat infiltration of intercostal muscles measured by CT histogram analysis and their correlations with COPD severity. Acad Radiol. 2014;21(6):711–7.
Gloor M, Fasler S, Fischmann A, Haas T, Bieri O, Heinimann K, et al. Quantification of fat infiltration in oculopharyngeal muscular dystrophy: comparison of three MR imaging methods. J Magn Reson Imaging. 2011;33(1):203–10.
North American Spine Society. Diagnosis and treatment of degenerative lumbar spinal stenosis: evidence-based clinical guidelines for multidisciplinary spine care. Burr Ridge, IL: North American Spine Society; 2011.
Gassman EE, Powell SM, Kallemeyn NA, Devries NA, Shivanna KH, Magnotta VA, et al. Automated bony region identification using artificial neural networks: reliability and validation measurements. Skelet Radiol. 2008;37(4):313–9.
Yanik B, Keyik B, Conkbayir I. Fatty degeneration of multifidus muscle in patients with chronic low back pain and in asymptomatic volunteers: quantification with chemical shift magnetic resonance imaging. Skelet Radiol. 2013;42(6):771–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mannil, M., Burgstaller, J.M., Thanabalasingam, A. et al. Texture analysis of paraspinal musculature in MRI of the lumbar spine: analysis of the lumbar stenosis outcome study (LSOS) data. Skeletal Radiol 47, 947–954 (2018). https://doi.org/10.1007/s00256-018-2919-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-018-2919-3