Abstract
Enter toxigenic Escherichia coli (ETEC) is a major pathogen of swine industry that can have a substantial impact on morbidity and mortality. Therefore, it is necessary to develop effective vaccines for the prevention of ETEC infection. Live attenuated bacteria delivery system are effective tools for mucosal immunization. The purpose of this study was to construct a novel delivery system that can present the LTR192G-STb fusion protein as oral vaccine candidate. Firstly, the PRPL-mKate2 fluorescent cassette was inserted into the genome (yaiT pseudogene) of an attenuated E. coli by homologous recombination methods to construct the delivery system O142(yaiT::PRPL-mKate2). Secondly, the oral vaccine O142(yaiT:: LT192-STb) (ER-B) was derived for replacing the PRPL-mKate2 by LT192-STb fusion gene, and then it was tested for its feasibility as oral vaccine candidate. Subsequently, BALB/c mice were orogastrically immunized with ER-B. Results showed that mice orally immunized with ER-B produced high levels of specific IgA and IgG antibodies. The induced antibodies demonstrated neutralizing effects to enter toxins LT and STb. In addition, results of cellular immune responses showed that stimulation index values of immunized mice were significantly higher than the control group (P < 0.05) and with a marked shift towards Th 2 immunity. These data indicated that the recombinant E. coli ER-B could be a valuable candidate of future vaccines against ETEC infection.
Similar content being viewed by others
Introduction
Enter toxigenic Escherichia coli (ETEC)-associated diarrhea causes a substantial economic loss to pig industry worldwide due to high morbidity, mortality, and reduced growth rates (Liu et al. 2014b). The key virulence factors of ETEC in diarrhea are fimbriae and enterotoxins. Fimbriae mediate the attachment of E. coli to the surface of host epithelium cells. Enterotoxins, heat-labile (LT) and heat-stable (STa, STb), disrupt intestinal fluid homeostasis and cause fluid hypersecretion that results in diarrhea (Zhang et al. 2007). Generally, ETEC control was mainly based on antibiotic therapy and vaccines. However, antibiotic administration runs the risk of causing the emergence of drug-resistant E. coli strains (Bischoff et al. 2002; Feng et al. 2013; Smith et al. 2010; Wang et al. 2010), and vaccination is also an effective tool for ETEC prevention.
In China, sows are often vaccinated with inactivated vaccines containing K88 and LT antigens to protect their offspring against enteric infection with E. coli. However, these inactivated vaccines suffer from their relative slow onset of immunity and the lack of protection effect (Liu et al. 2014b). In addition, experimental subunit vaccines containing K88, K99, 987P, F41, and F18 fimbrial antigens show only limited protection against ETEC infection. Noticeably and interestingly, a recent epidemiological study showed that more than half of the porcine ETEC strains did not carry any of the fimbriae or adhesion genes (Liu et al. 2014b). In addition, this epidemiological study also showed that STb and LT were widely expressed in porcine ETEC strains, and they always reside in the same ETEC strain (Liu et al. 2014b). This may attribute to the reason that LT and STb genes were usually located in the same plasmid. Therefore, more emphasis should be laid on the entorotoxin antigens for future ETEC vaccine research, and STb and LT antigens need to be included for development of broadly polyvalent vaccines. Previously, antitoxin vaccines under development largely use LT antigens because they are strongly immunogenic (Zhang and Francis 2010). However, the STb antigen cannot be used directly as a vaccine component because of poor immunogenicity, only when it was conjugated to a large carrier protein (Zhang and Francis 2010). So far, a better way of conjugating STb to carrier protein was genetic fusions of STb and a detoxified heat-labile toxin protein (LTR192G) to elicit protective anti-STb and anti-LT antibodies simultaneously (Zhang and Francis 2010).
However, traditionally, subunit ETEC vaccines are delivered by injection, which makes mass immunization more costly and less safe, particularly in resource-poor developing countries (Wang and Coppel 2008). In addition, the expense of subunit vaccines also limits their use in developing countries. In order to avoid these drawbacks, alternative vaccination approaches are needed, and an alternative approach to prevention of ETEC infection is oral immunization. Orally delivered vaccines have several advantages over other routes of antigen delivery, including convenience, cost-effectiveness, and, most importantly, induction of both local and systemic immune responses (Liu et al. 2014a; Lourdault et al. 2014). Moreover, oral vaccination typically generates a large amount of secretory IgA (sIgA), which provides the first line in mucosal defense to animals (Wang and Coppel 2008). Despite vaccination of parent that could induce neutralizing antibodies, such could not be developed further due to loss of stimulating mucosal immune responses and keeping the enterotoxins from entering the body via the mucosa (Xu et al. 2011). Therefore, development of oral vaccines to elicit mucosal and systemic immune responses could be an effective strategy in ETEC control.
Given its ability for colonization in the intestine, attenuated E. coli may be appropriate for use as an oral antigen delivery vector that directly and efficiently presents antigen to the intestinal mucosa. Therefore, this study developed a live attenuated E. coli delivery system and utilized it to express LT192-STb fusion immunogen for oral vaccine candidate. This recombinant E. coli strain was evaluated in a mice model. The results indicated that oral immunization of this strain could induce specific mucosal and systemic immune response against ETEC infection.
Materials and methods
Bacterial strains, plasmids, and cells
The strains and plasmids used and constructed in this study are listed in Tables 1 and 2. E. coli O142 was deposited in the Chinese Veterinary Culture Collection Center (CVCC: C83920) and kindly provided by Prof. Yudong Cui (Heilongjiang Bayi Agricultural University, China). E. coli C83903 was purchased from China Institute of Veterinary Drug Control. Plasmids pDOC-K and pACBSCE were kindly supplied by Prof. David J Lee (School of Biosciences, University of Birmingham, UK). Plasmid pCP20 was kindly provided by Prof. Siguo Liu (Harbin Veterinary Research Institute, CAAS, China). Plasmid pMAL-c4x was purchased from NEB Co. (American). The pEASY-Blunt-Simple Cloning Kit was purchased from Bejing TransGen Biotech Co. (China). Plasmid pBV220 was stored in this lab. Plasmid pmKate2-N was kindly supplied by Dr. Dmitriy M. Chudakov (Shemiakin-Ovchinnikov Institute of Bioorganic Chemistry, Moscow, Russia). Plasmid pDS132 was kindly provided by Prof. D. Schneider (Joseph Fourier University, France). Small intestine cell lines of pigs (ZYM-DIEC02) were kindly provided by Prof. Yijing Li (Northeast Agricultural University, China).
Construction and characterization of the attenuated E. coli strain
Attenuated E. coli O142: △STa was constructed according to Gene Doctoring method (Lee et al. 2009) and λ-Red method (Datsenko and Wanner 2000). A schematic outline of the recombination strategy for constructing attenuated E. coli is shown in Appendix: Supplementary file, Fig. S1, panel A. Briefly, the 5′ end of the STa toxin gene (H1) was amplified from the E. coli O142 genome by PCR with the primers B1 and B2; these primers incorporated 5′ EcoR I and 3′ BamHI restriction sites into the amplified products which were used to ligate the H1 coding sequence into the pDOC-K plasmid (see Appendix: Supplementary file, Fig. S1, panel B). Similarly, the 3′ end of the STa toxin gene (H2) was amplified with the primers B3 and B4 and then subcloned into the pDOC-K plasmid by XhoI and SalI after the H1 fragment was inserted. Finally, the pSTa donor plasmid had been constructed. The pSTa donor plasmid was transformed into the E. coli O142 strain with the pACBSCE plasmid (see Appendix: Supplementary file, Fig. S1, panel C). Production of the I-SceI and the λ-Red recombinase originate from the pACBSCE plasmid which was then induced with l-arabinose. I-SceI cleaves the pSTa donor plasmid, resulting in generation of the linear DNA fragment for λ-Red-mediated recombination to generate the recombinant E. coli O142: Kan. E. coli O142: Kan was transformed with pCP20 plasmid (see Appendix: Supplementary file, Fig. S1, panel D) to express the FLP recombinase at 43 °C for removing the kanamycin cassette. Finally, the attenuated E. coli O142: △STa was constructed. The E. coli O142, O142: Kan, and O142: △STa were verified by PCR using the primers B1 and B4. The primers used for constructing the attenuated E. coli are listed in Table 3. The toxicity reduction in O142: △STa was examined using the suckling mouse assay and ZYM-DIEC02 cell assay. Overall, 100 μL of culture supernatant was inoculated intragastrically to suckling mice aged 4 days, and then the mice were killed after 4 h of inoculation. G/C (weight ratio of gut to the remaining carcass) ratios of ≥ 0.090 were considered positive for toxicity of STa (You et al. 2011). ZYM-DIEC02 cells were cultured in Dulbecco’s modification of Eagle medium (DMEM) containing 10 % heat-inactivated fetal bovine serum in a 96-well plate at 37 °C under 5 % CO2. The 100 μL of culture supernatant was added to each well. After 24 h of incubation at 37 °C under 5 % CO2, the change of the cells was observed. O142 was used as a positive control for STa toxicity.
Construction and characterization of the attenuated E. coli delivery system
A schematic outline of the recombination strategy for constructing the attenuated E. coli delivery system is shown in Appendix: Supplementary file, Fig. S2. Firstly, the rrnB terminator gene was amplified from the pMAL-c4x vector by PCR with the primers B5 and B6, which were designed to flank the rrnB with 5′-BamHI, SacI, NdeI, and SmaI and 3′-KpnI and NotI restriction enzyme sites. BamHI-SacI-NdeI-SmaI-rrnB-KpnI-NotI fragment was purified and cloned into the TA cloning vector pEASY-Blunt-Simple. Secondly, the CIts857-PRPL gene was amplified from the pBV220 vector with the primers B7 and B8 and then cloned into the BamHI-SacI-NdeI-SmaI-rrnB-KpnI-NotI fragment by SacI and NdeI to construct the CIts857-PRPL-rrnB fragment. Thirdly, the mKate2 far-red fluorescent protein gene was amplified from the pmKate2-N vector with the primers B9 and B10 and then cloned into the CIts857-PRPL-rrnB fragment by NdeI and SmaI to construct the PRPL-mKate2 cassette. The PRPL-mKate2 cassette was inserted into the MCS1 of pDOC-K plasmid by BamHI and KpnI to construct the pmKate2 plasmid.
The insertion site of IS3B element on the pseudogene yaiT located at E. coli O142: △STa genome was chosen for insertion of exogenous gene. The 400 bp of the left side of the insertion site (yaiT-L) was amplified with the primers B11 and B12 and cloned into pmKate2 plasmid by BamHI and SacI. Similarly, the 400 bp of the right side of the insertion site (yaiT-R) was amplified with the primers B13 and B14 and then cloned into the MCS2 of pmKate2 plasmid by XhoI and SpeI after the yaiT-L fragment was inserted to construct the pmKate2-donor plasmid. The pmKate2-donor plasmid was transformed into the E. coli O142: △STa strain with the pACBSCE plasmid and induced the recombination as mentioned above for constructing the red-fluorescent indicator E. coli strain O142(yaiT::PRPL-mKate2), which was verified by PCR using the primers B11 and B14. The primers used for constructing the attenuated E. coli delivery system are listed in Table 4. The delivery system was cultured on LB medium and shaked separately at 43 and 30 °C to verify its ability to be counter-selected.
Construction and characterization of the recombinant E. coli for oral vaccine candidate
The LT gene was mutated at the nucleotides coding for the 192nd amino acid, and the STb-6*His chimeric gene was fused at the 3′ end of the LT192 genes by using an Arg-Ala-Arg-Tyr-Pro-Gly-Ile linker (Zhang and Francis 2010). Nucleotide segments coding for the LT192-STb chimeric gene were amplified by joining two pieces of DNA fragments by splice overlapping extension (SOE) PCR (see Appendix: Supplementary file, Fig. S3, panel A). Briefly, the first piece of fragment consisted of the native LT promoter, the LT192 A subunit, the LT B subunit, and the linker. That came from an overlap of two PCR products: one by primer B15 paired with primer B16 and the other by primer B17 paired with primer B18, with E. coli C83903 as the template. The second piece of fragment contained nucleotides coding the linker, the STb, the 6*his, the stop codon, and the native LT terminator. This fragment was generated by the overlap of another two PCR products: one by primer B19 with primer B20 and the other by primer B21 with primer B22, with E. coli C83903 as the template. The second fragment was further overlapped to the first fragment in a final SOE PCR to generate the LT192-STb chimeric gene (LT192-STb cassette).
LT192-STb cassette was inserted into pDS132 suicide plasmid by PstI to yield the pL-STb plasmid. The 800 bp of the left side of the insertion site (yaiT-L-arm) was amplified with the primers B23 and B24 and cloned into pL-STb plasmid by NotI and NheI. Then, the 800 bp of the right side of the insertion site (yaiT-R-arm) was amplified with the primers B25 and B26 and cloned into the pL-STb plasmid by XhoI and SpeI after the yaiT-L-arm fragment was inserted to yield the pL-S-Donor plasmid. The pL-S-Donor plasmid was electrotransformed into E. coli O142(yaiT::PRPL-mKate2), and then chloromycetin (cat)- and kanamycin (kan)-resistant colonies were subcultured on LB agar plates containing 5 % sucrose. Appropriate transconjugants were grown in sucrose-supplemented LB agar plates and cannot emit fluorescence under ultraviolet rays due to lose of the pL-S-Donor suicide plasmid and replacement of the PRPL-mKate2 cassette (see Appendix: Supplementary file, Fig. S3, panel B). The recombinant E. coli O142(yaiT:: LT192-STb) (ER-B) was further identified by PCR using primers B27 and B28, which anneals to the STb gene and the yaiT-R-arm, respectively. The primers used for constructing the recombinant E. coli are listed in Table 5. For analysis of LT192-STb fusion protein expression by ER-B, a colony of the recombinant strain was inoculated into 3 mL LB medium at 37 °C with 200 rpm shaking on a HZQX100 orbital shaker (Harbin Dongming Medical Instrument Factory, China). A 500-μL volume of an overnight culture was centrifuged at 10,000 g for 5 min and the bacterial pellet washed twice in phosphate-buffered saline (PBS, pH 7.4). The bacterial pellet was suspended in 500 μL deionised water and boiled for 10 min, and then 12 % sodium dodecyl sulphate–polyacrylamide gel electrophoresis was performed. Protein extracts were then electrotransferred onto a nitrocellulose membrane for western blot analysis using anti-his (ZSGB-BIO Co.; 1:500) and HRP-conjugated goat anti-mouse IgG (ZSGB-BIO Co.; 1:2500) antibodies and detected with ECL Plus Reagent Kit (7 Sea Biotech, China) following the manufacturer's instructions.
Feasible evaluation of recombinant E. coli for oral vaccine candidate
The E. coli strain ER-B was tested for its feasibility as oral vaccine in six aspects. Firstly, toxicity reduction in ER-B was tested as mentioned above. Briefly, soybean trypsin inhibitor (2 mg/mL; Solarbio, Beijing, China) was added in the suckling mouse assay. 344-C was used as a positive control for STb toxicity, and 274-A was used as a positive control for LT toxicity. Secondly, survival properties of the recombinant E. coli in gastrointestinal environments were analyzed. Briefly, the LB medium containing 10 % of the recombinant E. coli strains was supplemented with gastric acid (1.5, 2.5, 3.5, or 4.5 in pH), intestinal juice, and bile (0.05, 0.1, 0.2, 0.3, and 0.4 %), respectively, and grown at 37 °C for 8 h with shaking. The surviving bacteria were enumerated intermittently via the plate method. Thirdly, BALB/c mice aged 6 weeks were divided into five groups. The control group received 100 μL doses of PBS, and the four test groups were fed ER-B doses of 109 CFU, 1010 CFU, 1011 CFU, and 1012 CFU, respectively, to evaluate its safety. The mice were fed with ER-B or PBS for 3 days and then were measured to the feed intake and body weight at 2-day intervals. Fourth, one isolated colony on LB agar of E. coli strain ER-B, O142, O142: △STa was inoculated in 50 mL of LB medium and cultured at 37 °C with 220 rpm shaking. Samples were taken at 2-h intervals and analyzed via the plate method to generate growth curves. Fifth, the ER-B was grown in LB medium at 37 °C with shaking. Serial subcultures were performed by diluting the culture in fresh broth (1:100) and growing until the mid-exponential phase was reached (OD600 at 1.0). After 100 generations, several colonies were randomly picked and analyzed by PCR with primers B27 and B28 as described above to assess the structural stability of ER-B. Sixth, 6-week-old BALB/c mice were dosed with nalidixic acid-resistant strains of ER-B( Nal R ) for 109 CFU. The fecal samples were collected on days 0, 7, 14, 21, 28, 35, and 42. The fecal sample of 1 g was dissolved in sterile PBS and then incubated at LBNal agar plates at 37 °C overnight. Mice fed with sterile PBS were used as the control. The colonies from the LBNal agar plates were further analyzed by PCR using primers B27 and B28 as mentioned above to determine if the colonies are ER-B strain.
Intragastric immunization and sample collection
A total of 40 six-week-old female BALB/c mice (Liaoning Changsheng Biotechnology Co., Ltd., China) were divided into four groups (A, B, C1, and C2) of ten mice per group. These mice had free access to a standard mouse diet and water. ER-B was cultured in improved MINCA medium and centrifuged. Cell pellets were washed once with sterile PBS and resuspended in milk to a concentration of 1010 CFU/mL. Mice in groups A and B were orally immunized with 109 CFUs of ER-B. Mice in groups C1 and C2 received 0.1 mL doses of milk. Mice in all groups were immunized on days 0, 14, and 28. The immune protocol was administered on 6-h intervals thrice at every immune phase. Mice in groups B and C2 were coupled with equivalent male mice at day 21 and got pregnant by the male mice.
ELISA analysis for antibody levels
Mouse serum and fecal samples was collected on days 0, 7, 14, 21, 28, 35, and 42. Spleens, mesenteric lymph nodes, and intestinal mucus samples were collected on day 42. Milk of pregnant mice was collected on day 4 after delivery. Spleens, mesenteric lymph nodes, intestinal mucus, and fecal samples were homogenized in 400 μL of PBS, followed by centrifugation at 12,000 g for 30 min. The supernatant was stored at −20 °C.
Indirect ELISA with F41 fimbriae (200 ng/well), LTA recombinant protein (50 ng/well), LTB recombinant protein (50 ng/well), and MBP-STb recombinant protein (200 ng/well) were used to titrate antibodies. Treated samples were used as the primary antibodies in a binary dilution. HRP-conjugated goat anti-mouse IgA (Sigma-Aldrich, America) or IgG (ZSGB-BIO Co., China) diluted at 1:5000 was used as the secondary antibody. The optical density (OD) was measured at 450 nm after 10 min of development in preoxidase substrates (TMB, Tiangen Biotech Co., China).
Lymphocyte proliferation assay and flow cytometry for cellular immune responses
On day 42 after the first vaccination, splenic lymphocytes and mesenteric lymphocytes were collected for the determination of lymphocyte proliferation by MTT assay as described previously (Zeng et al. 2013). Briefly, cells (5 × 105/well) were added to 96-well plates for 100 μL and stimulated in vitro with LT (10 μg/mL), STb (10 μg/mL), and LT192-STb (10 μg/mL) proteins for 100 μL, respectively. Then, 10 μg/mL of concanavalin A (con A) as a positive control was added for 100 μL. Black controls without proteins were set up. The absorbance at 570 nm (A 570) was measured. The stimulation index (SI) was calculated according to the A 570 ratio and used to evaluate the proliferation of splenic lymphocytes and mesenteric lymphocytes.
For Th cell differentiation, Th 1 (IFN-γ) and Th 2 (IL-4) were detected using flow cytometry. Cytometry protocols were deployed in accordance with those suggested by the manufacturer. Briefly, cells were treated with fluorescein isothiocyanate-labeled anti-CD3 (Miltenyi Biotec, Germany) and allophycocyanin-labeled anti-CD8 (Miltenyi Biotec, Germany) antibody. After washing, cells were treated with phycoerythrin (PE)-labeled anti-IFN-γ (eBiosciences, USA) and PE-labeled anti-IL-4 (eBiosciences, USA) antibody, respectively. Finally, the treated cells were analyzed using flow cytometry (FCM).
In vitro neutralization ability of the induced antibodies on ZYM-DIEC02 cell
Serum, intestinal mucus, splenocyte lysate, and mesenteric lymphocyte lysate from mice immunized with recombinant E. coli expressing LT192-STb fusion antigen were evaluated to determine the neutralization ability of the induced antibodies with slight modifications as described previously (Feng et al. 2013). Briefly, enterotoxins (STb and LT) were diluted (1:2.5, 1:5, 1:10, 1:15, 1:20, and 1:25) with DMEM, and 50 μL of it was added into an equal volume of samples from immunized mice described above; the mixture was incubated at 37 °C for 2 h. Then, the antibody–toxin mixture was added to the ZYM-DIEC02 cells and incubated at 37 °C under 5 % CO2 and observed for 24 h. Samples from control group as the negative control were used.
In vivo neutralization ability of the induced antibodies to STb toxin on suckling mice
In vivo neutralization ability of the induced antibodies to STb toxin was determined using the suckling mouse assay as described above with slight modifications. In brief, 50 μL of STb toxin in serial dilutions (1:2.5, 1:5, 1:7.5, 1:10, 1:12.5, and 1:15) was mixed with equal volume of samples from immunized mice for 2 h at 37 °C, and then soybean trypsin inhibitor (2 mg/ml; Solarbio, Beijing, China) was added. The suckling mice of 4 days were inoculated intragastrically with the antibody–toxin mixture and killed after 4 h of inoculation. Samples from control group as the negative control were used.
Suckling mice challenge after birth by the immunized pregnant mice
The protective efficacy of passive immunization with milk from the immunized pregnant mice was evaluated using the suckling mouse assay as described above. In brief, 100 μL of STb toxin in serial dilutions (1:5, 1:10, 1:15, 1:20, 1:25, 1:30, and 1:35) was added to soybean trypsin inhibitor (2 mg/ml; Solarbio, Beijing, China) and then fed to suckling mice on day 4 after birth by the immunized pregnant mice. After 4 h, the suckling mice were killed and considered for the G/C ratios. Suckling mice from the control group as the negative control were used.
Statistical analysis
Statistical analysis was performed using ANOVA by SPSS version 19.0. P values of <0.05 were considered to be statistically significant.
Ethics statement
The present study did not involve endangered or protected species. The animal study complied with the Animal Welfare Act by following the NIH guidelines (NIH Pub. No. 85-23, revised 1996), and protocols were approved and supervised by Animal Care and Use Committee of Northeast Agricultural University.
Results
Construction of the attenuated E. coli and its toxicity
E. coli O142, O142: Kan, and O142: △STa were verified by PCR using the primers B1 and B4. PCR products showed the expected size from E. coli O142 (STa gene, 526 bp), O142: Kan (Kan cassette, 1549 bp), and O142: △STa (FRT site, 305 bp) (see Appendix: Supplementary file, Fig. S1, panel E). Supernatant of E. coli O142: △STa did not induce a significant fluid accumulation (G/C = 0.071 ± 0.007), in contrast to that of E. coli O142 (G/C = 0.127 ± 0.011) (see Appendix: Supplementary file, Fig. S1, panel F). Similarly, supernatant of O142: △STa did not induce ZYM-DIEC02 cells to death, in contrast to that of O142 (see Appendix: Supplementary file, Fig. S1, panel G), indicating that O142: △STa had toxicity eliminated.
Construction of the attenuated E. coli delivery system and its ability for inversion screen
The red-fluorescent indicator E. coli strain was identified by PCR using the primers B11 and B14. PCR products showed the expected size from E. coli O142: △STa (yaiT gene, 795 bp), O142: △STa/pmKate2-donor (yaiT gene, 795 bp; pmKate2-donor, 4393 bp), and O142(yaiT::PRPL- mKate2) (PRPL- mKate2 cassette flanked with yaiT, 4393 bp) (see Appendix: Supplementary file, Fig. S2, panel B).
The O142(yaiT::PRPL-mKate2) was cultured on LB medium and incubated at 30 and 43 °C, respectively. Colonies expressing mKate2 fluorescent protein showed a characteristic red color under normal light and a stronger red fluorescence under ultraviolet rays after 18 h at 43 °C, and colonies showed normal color at 30 °C (see Appendix: Supplementary file, Fig. S2, panel C).
Construction of the recombinant E. coli and its expression of LT192-STb fusion antigen
The recombinant E. coli ER-B was verified by PCR using the primers B27 and B28. PCR product of ER-B showed the expected size (795 bp) for LT192-STb fusion gene, and PCR product of O142: △STa and O142(yaiT::PRPL- mKate2) did not show any bands (see Appendix: Supplementary file, Fig. S3, panel C). Furthermore, Western blot analysis of LT192-STb fusion protein showed the expected size (20.9 kDa) for His-tagged LTB-STb (see Appendix: Supplementary file, Fig. S3, panel D).
Feasible analysis of recombinant E. coli for oral vaccine candidate
In the presence of trypsin inhibitor, supernatant of ER-B did not induce significant fluid accumulation within the intestinal tract of mice (G/C = 0.073 ± 0.008); in contrast, the supernatant of E. coli 344-C induced an obvious fluid secretion in the intestinal lumen (G/C = 0.118 ± 0.014), indicating that ER-B is no longer toxic (see Appendix: Supplementary file, Fig. S4, panel A). Meanwhile, in vitro cytotoxicity assay showed that supernatant of E. coli 274-A (LT) and 344-C (STb) caused ZYM-DIEC02 cells death, and the cells that were treated with supernatant of ER-B grew well (see Appendix: Supplementary file, Fig. S4, panel B). The tolerance of ER-B indicated that this strain had a good property of tolerance of pH 2.5 to 4.5 gastric acid, intestinal juice, and 0.05 to 0.2 % bile (see Appendix: Supplementary file, Fig. S4, panel C to E). Results of safety assay showed that appetite and avoirdupois did not have obvious change after feeding with 109 and 1010 CFU of ER-B to mice (see Appendix: Supplementary file, Fig. S4, panel F to G). The growth in LB medium of the E. coli strains showed that deletion of STa gene and insertion of LT192-STb fusion gene into the genome did not substantially affect the growth of the bacterial cell (see Appendix: Supplementary file, Fig. S4, panel H). Results of structural stability assay showed that ER-B had good stability properties, with no loss of the LT192-STb fusion gene (data not show). Fimbriae on the surface of E. coli ER-B, O142: △STa, and O142 were examined with an electron microscope, and the results showed that deletion of the STa gene and insertion of the LT192-STb fusion gene did not affect the fimbriae expression (see Appendix: Supplementary file, Fig. S4, panel I). The count of ER-B from immunized mice was determined via the plate method and PCR. Data showed that ER-B was able to colonize the intestinal tract of immunized mice (see Appendix: Supplementary file, Fig. S4, panel J).
Systemic and mucosal immunogenicity in mice induced by recombinant E. coli
The local mucosal and systemic immune responses were investigated by measuring the specific IgG and IgA levels after oral immunization, respectively. The results showed that there was no substantial difference (P > 0.05) in specific IgG and IgA levels between experimental groups and control groups prior to immunization, while oral immunization of ER-B elicited an antigen-specific antibody response. From days 7, 14, 21, 28, 35, and 42 after first immunization, high levels of anti-LTA, anti-LTB, anti-STb, and anti-F41 IgG were obtained in serum samples (Fig. 1a–d). Similarly, the specific IgG antibodies could be observed on day 42 after first immunization in milk, spleens, mesenteric lymph nodes, and intestinal mucus samples, respectively (Fig. 1e–h). Likewise, analysis of specific IgA antibodies obtained from the same animals revealed that the mice displayed a high level of IgA in feces, spleens, milk, mesenteric lymph nodes, and intestinal mucus samples, respectively (Fig. 2a–h).
The specific IgG response induced after intragastric immunization with ER-B. a Anti-LTA-specific IgG level in the serum of immunized mice. b Anti-LTB-specific IgG level in the serum of immunized mice. c Anti-STb-specific IgG level in the serum of immunized mice. d Anti-F41-specific IgG level in the serum of immunized mice. e Specific IgG level in the milk samples of immunized mice. f Specific IgG level in the spleen samples of immunized mice. g Specific IgG level in the mesenteric lymph node samples of immunized mice. h Specific IgG level in the intestinal mucus samples of immunized mice. Mean values are shown, and error bars represent standard deviations. *P < 0.05; **P < 0.01; ***P < 0.001
The specific IgA response induced after intragastric immunization with ER-B. a Anti-LTA-specific IgA level in the fecal samples of immunized mice. b Anti-LTB-specific IgA level in the fecal samples of immunized mice. c Anti-STb-specific IgA level in the fecal samples of immunized mice. d Anti-F41-specific IgA level in the fecal samples of immunized mice. e Specific IgA level in the spleen samples of immunized mice. f Specific IgA level in the milk samples of immunized mice. g Specific IgA level in the mesenteric lymph node samples of immunized mice. h Specific IgA level in the intestinal mucus samples of immunized mice. Mean values are shown, and error bars represent standard deviations. *P < 0.05; **P < 0.01; ***P < 0.001
Cellular immunogenicity in mice induced by recombinant E. coli
Proliferations of splenic lymphocytes and mesenteric lymphocytes were detected by MTT assay. For splenic lymphocyte proliferation, the stimulation by LT192-STb (SI = 2.219 ± 0.221, P < 0.01) stimulated the most potent production of specific T-lymphocytes, followed by STb (SI = 1.963 ± 0.155, P < 0.01) and LT (SI = 1.635 ± 0.142, P < 0.05) (Fig. 3a). For mesenteric lymphocyte proliferation, the stimulation by LT192-STb (SI = 3.442 ± 0.757, P < 0.001) stimulated the most potent production of specific T-lymphocytes, followed by LT (SI = 3.233 ± 0.566, P < 0.001) and STb (SI = 2.755 ± 0.815, P < 0.01) (Fig. 3b).
Results of cellular immune responses in mice following oral immunization with recombinant E. coli strain ER-B. a Proliferative responses in splenic lymphocytes stimulated with different antigens. b Proliferative responses in mesenteric lymphocytes stimulated with different antigens. c FCM assay for specific Th 1 (IFN-γ) and Th 2 (IL-4) cytokine production in mesenteric lymph node cells of mice immunized with ER-B. d FCM assay for specific Th 1 (IFN-γ) and Th 2 (IL-4) cytokine production in spleen cells of mice immunized with ER-B. SI stimulation index, FCM flow cytometry
The Th 1 (IFN-γ)/Th 2 (IL-4) ratio in mesenteric lymph node cells of immunized mice (ratio = 0.75) was lower than the PBS-controlled mice (ratio = 1.04), supporting the idea of a biased Th 2 immune response in immunized mice (Fig. 3c). However, there was no obvious change of Th 1 (IFN-γ)/Th 2 (IL-4) ratio in spleen cells between immunized mice (ratio = 1.01) and the PBS-controlled mice (ratio = 1.00) (Fig. 3d).
Toxin-neutralizing activity in vitro
The protective ability of serum, intestinal mucus, splenocyte lysate, and mesenteric lymphocyte lysate from immunized mice was evaluated in an in vitro neutralization assay performed using ZYM-DIEC02 cells. Samples from the immunized mice showed obvious neutralization efficiency to STb toxin when compared with that from control mice in serum (1: 15 vs. 1: 25), intestinal mucus (1: 15 vs. 1: 25), splenocyte lysate (1: 15 vs. 1: 25), and mesenteric lymphocyte lysate (1: 10 vs. 1: 25) (see Appendix: Supplementary file, Fig. S5, panel A). Similarly, the minimum dilution gradient of samples from the immunized mice for LT toxin causing ZYM-DIEC02 cells to death greater than that of control mice in serum (1: 20 vs. 1: 25), intestinal mucus (1: 15 vs. 1: 25), splenocyte lysate (1: 10 vs. 1: 25), and mesenteric lymphocyte lysate (1: 10 vs. 1: 25) (see Appendix: Supplementary file, Fig. S5, panel B). These results indicated that the presence of specific antibodies conferred obvious neutralizing effects against the toxicity of LT and STb.
Toxin-neutralizing activity in vivo
The neutralizing potential to STb toxin of samples from immunized mice was tested in the suckling mouse assay. The results showed that samples from the immunized mice showed obvious neutralization efficiency when compared with that from control mice in serum (1: 5 vs. 1: 12.5), intestinal mucus (1: 5 vs. 1: 12.5), splenocyte lysate (1: 7.5 vs. 1: 15), and mesenteric lymphocyte lysate (1: 5 vs. 1: 12.5) (Fig. 4a–d).
Neutralization of STb activity in the suckling mice assay by samples from mice immunized with ER-B. The toxin–sample mixtures were made by mixing serially twofold diluted STb toxin in PBS with an equal volume of samples. a Serum from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice. b Intestinal mucus from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice. c Splenocyte lysate from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice. d Mesenteric lymphocyte lysate from immunized mice showed neutralization efficiency to STb toxin when compared with that from control mice
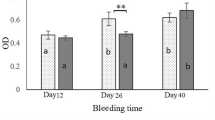
Protection efficacy of the suckling mice after intaking milk of immunized mice
To test the protective efficacy of passive immunization with milk, the suckling mice from the immunized pregnant mice were challenged with STb toxin. The results showed that G/C ratios from the immunized suckling mice had a negative value (G/C = 0.084 ± 0.006) after challenge with 1:10 diluted STb toxin. By contrast, G/C ratios from the control mice had a negative value (G/C = 0.086 ± 0.004) after challenge with a comparatively large diluted toxin (1:20) (Fig. 5).
Discussion
For a delivery system, being able to adhere to and colonize the intestinal tract is important and desirable. In this study, we investigated the colonization potentiality of the vaccine strain in mouse intestines by using the plate method. It was shown that the amounts of ER-B vaccine strain fed orally to mice were able to maintain at high numbers in the intestines. This colonization is expected to result in the expression of LT192-STb antigens in situ, achieving a more appropriate presentation of antigens for a prolonged period to the immune system (Turner et al. 2006). In addition, the tolerance of ER-B strain to gastric acid (pH 2.5) was determined for up to 3 h, to intestinal juice was determined for up to 16 h, and to bile was determined for up to 8 h. These results made it an attractive candidate as an agent for the delivery of antigens to the mucosa in particular vaccines. Furthermore, the live attenuated oral vaccine based on natural ETEC strains may have the added advantage of presenting ETEC antigens in addition to LT192-STb fusion antigen, which may add to the protection elicited. Finally, the stability of LT192-STb operon in ER-B is also an important parameter for vaccination efficiency. In this study, the ER-B containing LT192-STb operon was stably maintained in the constructs, and the expressed LT192-STb fusion antigen may be effectively secreted into the host animal (data not shown). These results indicated that the attenuated wild-type recombinant ETEC strain ER-B would be suitable for oral vaccine candidate.
mKate2 is a monomeric far-red fluorescent protein that has high brightness, far-red emission spectrum, strong penetrability, and excellent pH resistance and photostability, coupled with low toxicity, making it a superior fluorescent tag for imaging in living cells (Shcherbo et al. 2009). In a previous preliminary experiment, mKate2 was placed downstream of different promoters (Ptac, PRPL, Prhamnose, and Pmelibiose) and signal peptide (pelB, phoA, ompA, and lamB) for generating several different indicators (data not shown). In these combinations, the PRPL-mKate2 operon showed the best effect (data not shown). Therefore, we further inserted the Kan-PRPL-mKate2 operon into the genome of E. coli to construct the live attenuated E. coli delivery system, which showed normal color at lower temperature, but showed a characteristic red color under normal light and a stronger red fluorescence under ultraviolet rays. According to this characteristic, we replaced the Kan-PRPL-mKate2 operon by target gene (LT192-STb fusion gene) for generating the recombinant vaccine strain ER-B readily. A feature of this study was that we are able to use the pseudogene for insertion of the exogenous gene. The bacterial pseudogenes are defined as defunct genomic loci with sequence similarity to functional genes but lacking coding potential due to the presence of disruptive mutations such as frame shifts and premature stop codons. Therefore, deletion, insertion, or mutation of the pseudogene has no influence on growth or biological activity for bacterial strains (Balakirev and Ayala 2003; Echols et al. 2002; Harrison et al. 2001; Mighell et al. 2000). Of the pseudogenes, yaiT gene, inserted by IS element in many E. coli strains, was selected for exogenous gene inserted since it is far away from the origin (84 min on the E. coli K-12 genetic map) and the termination (33 min on the E. coli K-12 genetic map) of chromosomal replication, adding no additional stress for growth and biological activity of the bacterial strain (Liu et al. 2014a). After insertion, exogenous gene replicates in company with genome of E. coli, allowing a high and stable expression of the heterologous protein. The results also showed that LT192-STb fusion gene of ER-B strain has good segregational and structural stability without showing any structural rearrangement (data not shown).
The STb gene is highly prevalent in ETEC strains isolated from diarrheal piglets (Liu et al. 2014b; Zhang et al. 2007), and infection with an ETEC strain containing STb as the only toxin caused clinical diarrhea in more than half of gnotobiotic piglets (Zhang and Francis 2010). In addition, STb is more potent to older piglets and tends to stimulate more fluid in ligated loops (Erume et al. 2008; Zhang and Francis 2010). Therefore, STb antigen must be included in developing broadly effective vaccines against ETEC infection. However, STb toxin cannot be used as an antigen in vaccine development, unless it is conjugated to a large carrier protein to enhance its immunogenicity (Dubreuil et al. 1996; Sears and Kaper 1996; Taxt et al. 2010). Of the carrier proteins, LT protein has been regarded as the best adjuvant in eliciting host mucosal immunity and plays a key role in enhancing the immunogenicity of passenger proteins (Taxt et al. 2010). Most of the previous studies used the B subunit of LT as the carried protein since it provides immunization against LT as well as having the ability to target the conjugate to the GM1 receptors at host epithelial cells, resulting in the uptake of co-administered proteins and enhancement of both mucosal and cellular immune responses. Cardenas and Clements (1993) constructed a recombinant E. coli strain expressing LTB-ST fusion peptide, which was able to elicit mucosal protection against ST toxin (Cardenas and Clements 1993). Further, a recent study indicated that the A subunit of LT also plays a role as mucosal adjuvant and promotes IgG2a, IgA, and Th17 responses to vaccine antigens (Norton et al. 2012). Therefore, selection of the full-length LT as carrier protein would be more suitable for enhancing the immunogenicity of passenger proteins. Zhang and Francis (2010) used an open reading frame (ORF) of LT toxin (LTR192G) derived from porcine ETEC to carry a mature STb peptide for LT192 (ORFs)-STb fusions to elicit anti-LT and anti-STb immunity simultaneously (Zhang and Francis 2010). However, this LT192 (ORFs)-STb fusion gene was controlled by l-arabinose promoter and induced by l-arabinose as the inducer, making it incompatible for designing the LT-STb fusion antigen into oral vaccine development. Therefore, in this study, we used the full-length porcine LT192 operon to conjugate with STb for generating LT192-STb fusion antigen, which retained the native LT promoter and expressed without induction and stimulated a fully mucosal immune response, making it more appropriate as a target immunogen for oral vaccine development. In addition, signal peptide of LT protein could secrete the LT192-STb antigen to the external of E. coli, and secretion is more suitable for heterologous antigen delivery by live bacteria than the cytoplasmic and surface-displayed expression (Hotz et al. 2009; Yigang and Yijing 2008).
The IgA and IgG antibody concentration was examined in the immunized group and control group for 6 weeks. Results showed that the specific IgA and IgG antibody titer in immunized group was generally increased post-inoculation of the ER-B, compared to those of control group. IgA is the predominant antibody at the mucosal surface, as its local production is greater than other immunoglobulins. Therefore, an efficient ETEC oral vaccine should be able to induce a specific mucosal IgA response. The result clearly showed that fecal sIgA levels against LTA (day 14, P < 0.05), LTB (day 21, P < 0.01), STb (day 21, P < 0.05), and F41 (day 14, P < 0.05) in immunized group were significantly increased compared to those of the control group. In addition, statistically significant differences of IgA were also observed for spleens, milk, mesenteric lymph nodes, and intestinal mucus. Similarly, the systemic IgG responses were also significantly increased in immunized groups compared to the control group (P < 0.05). These data suggest that oral immunizations can stimulate antigen-specific mucosal and systemic immune responses after intragastric administration.
In addition, SI ratio of cell proliferative responses showed a significant increase of splenocytes and mesenteric lymphocytes, indicating that LT-STb fusion antigen can stimulate antigen-sepcific cellular immune responses. Th 1 (IFN-γ)/Th 2 (IL-4) ratio in mesenteric lymph node cells of immunized mice was obviously decreased as compared to controlled mice, which further demonstrated that this cellular immune response is more skewed toward Th2. To maximize the protective efficacy, we evaluated the immunization strategy with the ER-B thrice with a 2-week interval. This protocol was adapted from a previous study (Challacombe 1983), which was consistently effective when mice were immunized with particulate oral vaccines. After immunization, the neutralization assay and the suckling mice challenge study showed that the immune potency could efficiently inhibit the toxicity of LT and STb, thereby resulting in effective protection against ETEC infection.
In summary, our results showed that recombinant E. coli RE-B possessed stronger immunogenicity, which made it a more appropriate candidate as orogastrically live bacterial vaccine against ETEC infection.
References
Balakirev ES, Ayala FJ (2003) Pseudogenes: are they “junk” or functional DNA? Annu Rev Genet 37:123–151. doi:10.1146/annurev.genet.37.040103.103949
Bischoff KM, White DG, McDermott PF, Zhao S, Gaines S, Maurer JJ, Nisbet DJ (2002) Characterization of chloramphenicol resistance in beta-hemolytic Escherichia coli associated with diarrhea in neonatal swine. J Clin Microbiol 40(2):389–394
Cardenas L, Clements JD (1993) Development of mucosal protection against the heat-stable enterotoxin (ST) of Escherichia coli by oral immunization with a genetic fusion delivered by a bacterial vector. Infect Immun 61(11):4629–4636
Challacombe SJ (1983) Salivary antibodies and systemic tolerance in mice after oral immunization with bacterial antigens. Ann N Y Acad Sci 409:177–193
Datsenko KA, Wanner BL (2000) One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc Natl Acad Sci U S A 97(12):6640–6645. doi:10.1073/pnas.120163297
Dubreuil JD, Letellier A, Harel J (1996) A recombinant Escherichia coli heat-stable enterotoxin b (STb) fusion protein eliciting neutralizing antibodies. FEMS Immunol Med Microbiol 13(4):317–323
Echols N, Harrison P, Balasubramanian S, Luscombe NM, Bertone P, Zhang Z, Gerstein M (2002) Comprehensive analysis of amino acid and nucleotide composition in eukaryotic genomes, comparing genes and pseudogenes. Nucleic Acids Res 30(11):2515–2523
Erume J, Berberov EM, Kachman SD, Scott MA, Zhou Y, Francis DH, Moxley RA (2008) Comparison of the contributions of heat-labile enterotoxin and heat-stable enterotoxin b to the virulence of enterotoxigenic Escherichia coli in F4ac receptor-positive young pigs. Infect Immun 76(7):3141–3149. doi:10.1128/IAI. 01743-07
Feng Y, Liu W, Shi D (2013) Effectiveness of egg yolk antibody against shiga toxin II variant toxicity in vitro and in vivo. Curr Microbiol 67(4):448–453. doi:10.1007/s00284-013-0384-8
Harrison PM, Echols N, Gerstein MB (2001) Digging for dead genes: an analysis of the characteristics of the pseudogene population in the Caenorhabditis elegans genome. Nucleic Acids Res 29(3):818–830
Hotz C, Fensterle J, Goebel W, Meyer SR, Kirchgraber G, Heisig M, Furer A, Dietrich G, Rapp UR, Gentschev I (2009) Improvement of the live vaccine strain Salmonella enterica serovar typhi Ty21a for antigen delivery via the hemolysin secretion system of Escherichia coli. Int J Med Microbiol 299(2):109–119. doi:10.1016/j.ijmm.2008.06.006
Lee DJ, Bingle LE, Heurlier K, Pallen MJ, Penn CW, Busby SJ, Hobman JL (2009) Gene doctoring: a method for recombineering in laboratory and pathogenic Escherichia coli strains. BMC Microbiol 9:252. doi:10.1186/1471-2180-9-252
Liu W, Yuan C, Bao J, Guan W, Zhao Z, Li X, Tang J, Li D, Shi D (2014a) Generation of an attenuated strain oral vaccine candidate using a novel double selection platform in Escherichia coli. Appl Microbiol Biotechnol. doi:10.1007/s00253-014-6099-3
Liu W, Yuan C, Meng X, Du Y, Gao R, Tang J, Shi D (2014b) Frequency of virulence factors in Escherichia coli isolated from suckling pigs with diarrhoea in China. Vet J 199(2):286–289. doi:10.1016/j.tvjl.2013.11.019
Lourdault K, Wang LC, Vieira A, Matsunaga J, Melo R, Lewis MS, Haake DA, Gomes-Solecki M (2014) Oral immunization with Escherichia coli expressing a lipidated form of LigA protects hamsters against challenge with Leptospira interrogans serovar copenhageni. Infect Immun 82(2):893–902. doi:10.1128/IAI. 01533-13
Mighell AJ, Smith NR, Robinson PA, Markham AF (2000) Vertebrate pseudogenes. FEBS Lett 468(2–3):109–114
Norton EB, Lawson LB, Mahdi Z, Freytag LC, Clements JD (2012) The A subunit of Escherichia coli heat-labile enterotoxin functions as a mucosal adjuvant and promotes IgG2a, IgA, and Th17 responses to vaccine antigens. Infect Immun 80(7):2426–2435. doi:10.1128/IAI. 00181-12
Philippe N, Alcaraz J P, Coursange E, Geiselmann J, Schneider D (2004) Improvement of pCVD442, a suicide plasmid for gene allele exchange in bacteria. Plasmid 51(3):246–55
Sears CL, Kaper JB (1996) Enteric bacterial toxins: mechanisms of action and linkage to intestinal secretion. Microbiol Rev 60(1):167–215
Shcherbo D, Murphy CS, Ermakova GV, Solovieva EA, Chepurnykh TV, Shcheglov AS, Verkhusha VV, Pletnev VZ, Hazelwood KL, Roche PM, Lukyanov S, Zaraisky AG, Davidson MW, Chudakov DM (2009) Far-red fluorescent tags for protein imaging in living tissues. Biochem J 418(3):567–574. doi:10.1042/BJ20081949
Smith MG, Jordan D, Chapman TA, Chin JJ, Barton MD, Do TN, Fahy VA, Fairbrother JM, Trott DJ (2010) Antimicrobial resistance and virulence gene profiles in multi-drug resistant enterotoxigenic Escherichia coli isolated from pigs with post-weaning diarrhoea. Vet Microbiol 145(3–4):299–307. doi:10.1016/j.vetmic.2010.04.004
Taxt A, Aasland R, Sommerfelt H, Nataro J, Puntervoll P (2010) Heat-stable enterotoxin of enterotoxigenic Escherichia coli as a vaccine target. Infect Immun 78(5):1824–1831. doi:10.1128/IAI. 01397-09
Turner AK, Beavis JC, Stephens JC, Greenwood J, Gewert C, Thomas N, Deary A, Casula G, Daley A, Kelly P, Randall R, Darsley MJ (2006) Construction and phase I clinical evaluation of the safety and immunogenicity of a candidate enterotoxigenic Escherichia coli vaccine strain expressing colonization factor antigen CFA/I. Infect Immun 74(2):1062–1071. doi:10.1128/IAI. 74.2.1062-1071.2006
Wang L, Coppel RL (2008) Oral vaccine delivery: can it protect against non-mucosal pathogens? Expert Rev Vaccines 7(6):729–738. doi:10.1586/14760584.7.6.729
Wang XM, Jiang HX, Liao XP, Liu JH, Zhang WJ, Zhang H, Jiang ZG, Lu DH, Xiang R, Liu YH (2010) Antimicrobial resistance, virulence genes, and phylogenetic background in Escherichia coli isolates from diseased pigs. FEMS Microbiol Lett 306(1):15–21. doi:10.1111/j.1574-6968.2010.01917.x
Xu Y, Cui L, Tian C, Zhang G, Huo G, Tang L, Li Y (2011) Immunogenicity of recombinant classic swine fever virus CD8(+) T lymphocyte epitope and porcine parvovirus VP2 antigen coexpressed by Lactobacillus casei in swine via oral vaccination. Clin Vaccine Immunol 18(11):1979–1986. doi:10.1128/CVI. 05204-11
Yigang XU, Yijing LI (2008) Construction of recombinant Lactobacillus casei efficiently surface displayed and secreted porcine parvovirus VP2 protein and comparison of the immune responses induced by oral immunization. Immunology 124(1):68–75. doi:10.1111/j.1365-2567.2007.02738.x
You J, Xu Y, He M, McAllister TA, Thacker PA, Li X, Wang T, Jin L (2011) Protection of mice against enterotoxigenic E. coli by immunization with a polyvalent enterotoxin comprising a combination of LTB, STa, and STb. Appl Microbiol Biotechnol 89(6):1885–1893. doi:10.1007/s00253-010-2991-7
Zeng Y, You X, Liu L, He J, Zhu C, Yu M, Ma X, Wu Y (2013) The immune effects of multiple antigen peptides containing the mimic epitopes of the adhesion protein of Mycoplasma genitalium. Can J Microbiol 59(7):479–484. doi:10.1139/cjm-2013-0204
Zhang W, Francis DH (2010) Genetic fusions of heat-labile toxoid (LT) and heat-stable toxin b (STb) of porcine enterotoxigenic Escherichia coli elicit protective anti-LT and anti-STb antibodies. Clin Vaccine Immunol 17(8):1223–1231. doi:10.1128/CVI. 00095-10
Zhang W, Zhao M, Ruesch L, Omot A, Francis D (2007) Prevalence of virulence genes in Escherichia coli strains recently isolated from young pigs with diarrhea in the US. Vet Microbiol 123(1–3):145–152. doi:10.1016/j.vetmic.2007.02.018
Acknowledgments
Financial support for this study was provided by grants from Synergetic Innovation Center of Food Safety and Nutrition, the National Science and Technology Support Project (2012BAD12B03-3, 2012BAD12B05-2), and the Science and Technology Planning Project of Heilongjiang Province (GC12B303). The authors thank director John E. Wertz (Yale University, American) for assistance in selecting the pseudogene for insertion of exogenous gene. We are grateful to Prof. David J. Lee for providing G-DOC recombination system, Prof. Siguo Liu for providing pCP20 plasmid, Prof. Yudong Cui for providing E. coli O142, Dr. Dmitriy Chudakov for providing pmKate2-N plasmid, Prof. D. Schneider for providing pDS132 suicide plasmid, and Prof. Yijing Li for providing ZYM-DIEC02 cell lines.
Conflict of interest
None of the authors has any financial or personal relationships that could inappropriately influence or bias the content of the paper.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 1322 kb)
Rights and permissions
About this article
Cite this article
Liu, W., Li, X., Bao, J. et al. Construction and evaluation of a fluorescence-based live attenuated Escherichia coli delivery system for generating oral vaccine candidate. Appl Microbiol Biotechnol 99, 4005–4018 (2015). https://doi.org/10.1007/s00253-014-6332-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-014-6332-0