Abstract
Background
Conventional chest and abdominal MRI require breath-holds to reduce motion artifacts. Neonates and infants require general anesthesia with intubation to enable breath-held acquisitions.
Objective
We aimed to validate a free-breathing approach to reduce general anesthesia using a motion-insensitive radial acquisition with respiratory gating.
Materials and methods
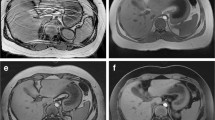
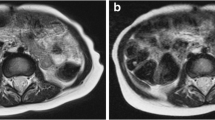
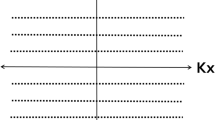
We retrospectively enrolled children <3 years old who were referred for MRI of the chest or abdomen. They were divided into two groups according to MRI protocol: (1) breath-held scans under general anesthesia with T2-weighted single-shot fast spin-echo (SSFSE) and contrast-enhanced T1-weighted modified Dixon, and (2) free-breathing scans using radial sequences (T2-W MultiVane XD and contrast-enhanced T1-W three-dimensional [3-D] Vane XD). Two readers graded image quality and motion artifacts.
Results
We included 23 studies in the free-breathing cohort and 22 in the breath-hold cohort. The overall imaging scores for the free-breathing radial T2-W sequence were similar to the scores for the breath-held T2-W SSFSE sequence (chest, 3.6 vs. 3.2, P=0.07; abdomen, 3.9 vs. 3.7, P=0.66). The free-breathing 3-D radial T1-W sequence also had image quality scores that were similar to the breath-held T1-W sequence (chest, 4.0 vs. 3.0, P=0.06; abdomen, 3.7 vs. 3.9, P=0.15). Increased motion was seen in the abdomen on the radial T2-W sequence (P<0.001), but increased motion was not different in the chest (P=0.73) or in contrast-enhanced T1-W sequences (chest, P=0.39; abdomen, P=0.15). The mean total sequence time was longer in free-breathing compared to breath-held exams (P<0.01); however, this did not translate to longer overall exam times (P=0.94).
Conclusion
Motion-insensitive radial sequences used for infants and neonates were of similar image quality to breath-held sequences and had decreased sedation and intubation






Similar content being viewed by others
References
Huang YY, Ing C, Li G, Sun LS (2016) Analysis of MRI utilization in pediatric patients. J Neurosurg Anesthesiol 28:413–418
Shi Y, Hu D, Rodgers EL et al (2018) Epidemiology of general anesthesia prior to age 3 in a population-based birth cohort. Paediatr Anaesth 28:513–519
United States Food and Drug Administration (2016) FDA drug safety communication: FDA review results in new warnings about using general anesthetics and sedation drugs in young children and pregnant women. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-review-results-new-warnings-about-using-general-anesthetics-and. Accessed 3 Jan 2022
United States Food and Drug Administration (2017) FDA drug safety communication: FDA approves label changes for use of general anesthetic and sedation drugs in young children. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-approves-label-changes-use-general-anesthetic-and-sedation-drugs. Accessed 3 Jan 2022
Stratmann G, Sall JW, May LD et al (2010) Beyond anesthetic properties: the effects of isoflurane on brain cell death, neurogenesis, and long-term neurocognitive function. Anesth Analg 110:431–437
Davidson AJ, Sun LS (2018) Clinical evidence for any effect of anesthesia on the developing brain. Anesthesiology 128:840–853
Davidson AJ, Disma N, de Graaff JC et al (2016) Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet 387:239–250
McCann ME, de Graaff JC, Dorris L et al (2019) Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): an international, multicentre, randomised, controlled equivalence trial [published correction appears in Lancet 394:638]. Lancet 393:664–677
Malviya S, Voepel-Lewis T, Eldevik OP et al (2000) Sedation and general anaesthesia in children undergoing MRI and CT: adverse events and outcomes. Br J Anaesth 84:743–748
Cravero JP, Beach ML, Blike GT et al (2009) The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: a report from the pediatric sedation research consortium. Anesth Analg 108:795–804
Schulte-Uentrop L, Goepfert MS (2010) Anaesthesia or sedation for MRI in children. Curr Opin Anesthesiol 23:513–517
Dorfman AL, Odegard KC, Powell AJ et al (2007) Risk factors for adverse events during cardiovascular magnetic resonance in congenital heart disease. J Cardiovasc Magn Reson 9:793–798
Jaimes C, Gee MS (2016) Strategies to minimize sedation in pediatric body magnetic resonance imaging. Pediatr Radiol 46:916–927
Jaimes C, Kirsch JE, Gee MS (2018) Fast, free-breathing and motion-minimized techniques for pediatric body magnetic resonance imaging. Pediatr Radiol 48:1197–1208
Lee JH, Choi YH, Cheon JE et al (2015) Improved abdominal MRI in non-breath-holding children using a radial k-space sampling technique. Pediatr Radiol 45:840–846
Cheng JY, Zhang T, Ruangwattanapaisarn N et al (2015) Free-breathing pediatric MRI with nonrigid motion correction and acceleration. J Magn Reson Imaging 42:407–420
Ruangwattanapaisarn N, Loening AM, Saranathan M et al (2015) Faster pediatric 3-T abdominal magnetic resonance imaging: comparison between conventional and variable refocusing flip-angle single-shot fast spin-echo sequences. Pediatr Radiol 45:847–854
Zucker EJ, Cheng JY, Haldipur A et al (2018) Free-breathing pediatric chest MRI: performance of self-navigated golden-angle ordered conical ultrashort echo time acquisition. J Magn Reson Imaging 47:200–209
Hirokawa Y, Isoda H, Maetani YS et al (2008) Evaluation of motion correction effect and image quality with the periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) (BLADE) and parallel imaging acquisition technique in the upper abdomen. J Magn Reason Imaging 28:957–962
Chandarana H, Block TK, Rosenkrantz AB et al (2011) Free-breathing radial 3D fat-suppressed T1-weighted gradient echo sequence: a viable alternative for contrast-enhanced liver imaging in patients unable to suspend respiration. Investig Radiol 46:648–653
Pipe JG (1999) Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 42:963
Hirokawa Y, Isoda H, Maetani YS et al (2008) MRI artifact reduction and quality improvement in the upper abdomen with PROPELLER and prospective acquisition correction (PACE) technique. AJR Am J Roentgenol 191:1154–1158
Liu J, Jin H, Chen Y et al (2021) Free-breathing BLADE acquisition method improves T2-weighted cardiac MR image quality compared with conventional breath-hold turbo spin-echo Cartesian acquisition. Acta Radiol 62:341–347
Choi KS, Choi YH, Cheon JE et al (2020) Application of T1-weighted BLADE sequence to abdominal magnetic resonance imaging of young children: a comparison with turbo spin echo sequence. Acta Radiol 61:1406–1413
Meier-Schroers M, Kukuk G, Homsi R et al (2016) MRI of the lung using the PROPELLER technique: artifact reduction, better image quality and improved nodule detection. Eur J Radiol 85:707–713
Zhang L, Tian C, Wang P et al (2015) Comparative study of image quality between axial T2-weighted BLADE and turbo spin-echo MRI of the upper abdomen on 3.0 T. Jpn J Radiol 33:585–590
Lane BF, Vandermeer FQ, Oz RC et al (2011) Comparison of sagittal T2-weighted BLADE and fast spin-echo MRI of the female pelvis for motion artifact and lesion detection. AJR Am J Roentgenol 197:W307–W313
Haneder S, Dinter D, Gutfleisch A et al (2011) Image quality of T2w-TSE of the abdomen and pelvis with Cartesian or BLADE-type k-space sampling: a retrospective interindividual comparison study. Eur J Radiol 79:177–182
Bayramoglu S, Kilickesmez O, Cimilli T et al (2010) T2-weighted MRI of the upper abdomen: comparison of four fat-suppressed T2-weighted sequences including PROPELLER (BLADE) technique. Acad Radiol 17:368–374
Vertinsky AT, Rubesova E, Krasnokutsky MV et al (2009) Performance of PROPELLER relative to standard FSE T2-weighted imaging in pediatric brain MRI. Pediatr Radiol 39:1038–1047
Zaccagnino E, Devincent C, Leelakanok N et al (2019) Assessment of quiet T2 weighted PROPELLER sequence in pediatric abdominal imaging. Clin Imaging 53:12–16
Balza R, Jaimes C, Risacher S et al (2019) Impact of a fast free-breathing 3-T abdominal MRI protocol on improving scan time and image quality for pediatric patients with tuberous sclerosis complex. Pediatr Radiol 49:1788–1797
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Quin Lu is an employee of Philips Healthcare. The remaining authors have no conflicts or competing interests relevant to this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Browne, L.P., Malone, L.J., Englund, E.K. et al. Free-breathing magnetic resonance imaging with radial k-space sampling for neonates and infants to reduce anesthesia. Pediatr Radiol 52, 1326–1337 (2022). https://doi.org/10.1007/s00247-022-05298-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-022-05298-7