Abstract
Background
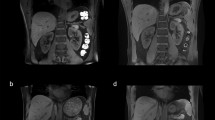
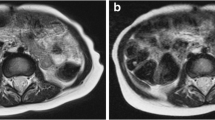
Magnetic resonance imaging (MRI) of the abdomen can be especially challenging in pediatric patients because of image quality degradation from respiratory motion. Abdominal MR protocols tailored for free-breathing children can potentially improve diagnostic image quality and reduce scan time.
Objective
To evaluate the performance of a free-breathing 3-T MRI protocol for renal evaluation in pediatric patients with tuberous sclerosis complex (TSC).
Materials and methods
A single institution, Institutional Review Board-approved, retrospective database query identified pediatric TSC patients who underwent a free-breathing 3-T MR abdominal protocol including radial and respiratory-triggered pulse sequences and who also had a prior abdominal MRI on the same scanner using a traditional MR protocol utilizing signal averaging and Cartesian k-space sampling. Scan times and use of sedation were recorded. MR image quality was compared between the two protocols using a semiquantitative score for overall image quality and sharpness.
Results
Forty abdominal MRI studies in 20 patients were evaluated. The mean scan time of the fast free-breathing protocol was significantly lower (mean: 42.5±9.8 min) compared with the traditional protocol (58.7±11.7 min; P=<0.001). Image sharpness was significantly improved for radial T2-weighted and T1-weighted triggered Dixon and radial T1-weighted fat-suppressed post-contrast images in the free-breathing protocol, while image quality was significantly higher on radial and Dixon T1-weighted sequences.
Conclusion
A free-breathing abdominal MR protocol in pediatric TSC patients decreases scan time and improves image quality and should be considered more widely for abdominal MRI in children.



Similar content being viewed by others
References
Hinton R, Prakash A, Romp RL et al (2014) Cardiovascular manifestations of tuberous sclerosis complex and summary of the revised diagnostic criteria and surveillance and management recommendations from the international tuberous sclerosis consensus group. J Am Heart Assoc 3:e001493
Northrup H, Krueger DA, International Tuberous Sclerosis Complex Consensus Group (2013) Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 international tuberous sclerosis complex consensus conference. Pediatr Neurol 49:243–254
Sasiwimonphan K, Takahashi N, Leibovich B et al (2012) Small (< 4 cm) renal mass: differentiation of angiomyolipoma without visible fat from renal cell carcinoma utilizing MR imaging. Radiology 263:160–168
Jaimes C, Gee MS (2016) Strategies to minimize sedation in pediatric body magnetic resonance imaging. Pediatr Radiol 46:916–927
Lim RS, Flood TA, McInnes MDF et al (2018) Renal angiomyolipoma without visible fat: can we make the diagnosis using CT and MRI? Eur Radiol 28:542–553
Farrell C, Noyes SL, Tourojman M, Lane BR (2015) Renal angiomyolipoma: preoperative identification of atypical fat-poor AML. Curr Urol Rep 16:12
Chandarana H, Block TK, Rosenkrantz AB et al (2011) Free-breathing radial 3D fat-suppressed T1-weighted gradient echo sequence: a viable alternative for contrast-enhanced liver imaging in patients unable to suspend respiration. Investig Radiol 46:648–653
Pipe JG (1999) Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 42:963–969
Hirokawa Y, Isoda H, Maetani YS et al (2008) MRI artifact reduction and quality improvement in the upper abdomen with PROPELLER and prospective acquisition correction (PACE) technique. AJR Am J Roentgenol 191:1154–1158
Cruz G, Atkinson D, Buerger C et al (2016) Accelerated motion corrected three-dimensional abdominal MRI using total variation regularized SENSE reconstruction. Magn Reson Med 75:1484–1498
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Jaimes C, Kirsch JE, Gee MS (2018) Fast, free-breathing and motion-minimized techniques for pediatric body magnetic resonance imaging. Pediatr Radiol 48:1197–1208
Chandarana H, Feng L, Block TK et al (2013) Free-breathing contrast-enhanced multiphase MRI of the liver using a combination of compressed sensing, parallel imaging, and golden-angle radial sampling. Investig Radiol 48:10–16
Vanderby SA, Babyn PS, Carter MW et al (2010) Effect of anesthesia and sedation on pediatric MR imaging patient flow. Radiology 256:229–237
Uffman JC, Tumin D, Raman V et al (2017) MRI utilization and the associated use of sedation and anesthesia in a pediatric ACO. J Am Coll Radiol 14:924–930
Robertson RL, Silk S, Ecklund K et al (2018) Imaging optimization in children. J Am Coll Radiol 15:440–443
Flick R, Katusic SK, Colligan RC et al (2011) Cognitive and behavioral outcomes after early exposure to anesthesia and surgery. Pediatrics 128:e1053–e1061
Zhang H, Du L, Du Z et al (2015) Association between childhood exposure to single general anesthesia and neurodevelopment: a systematic review and meta-analysis of cohort study. J Anesth 29:749–757
Gale EM, Caravan P, Rao AG et al (2017) Gadolinium-based contrast agents in pediatric magnetic resonance imaging. Pediatr Radiol 47:507–521
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Keith Heberlein is an employee of Siemens Medical Solutions, USA.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Balza, R., Jaimes, C., Risacher, S. et al. Impact of a fast free-breathing 3-T abdominal MRI protocol on improving scan time and image quality for pediatric patients with tuberous sclerosis complex. Pediatr Radiol 49, 1788–1797 (2019). https://doi.org/10.1007/s00247-019-04496-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-019-04496-0