Abstract
Background
There is a strong need for improvements in motion robust T1-weighted abdominal imaging sequences in children to enable high-quality, free-breathing imaging.
Objective
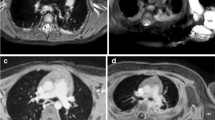
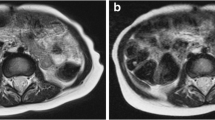
To compare imaging time and quality of a radial stack-of-stars, free-breathing T1-weighted gradient echo acquisition (volumetric interpolated breath-hold examination [VIBE]) three-dimensional (3-D) Dixon sequence in sedated pediatric patients undergoing abdominal magnetic resonance imaging (MRI) against conventional Cartesian T1-weighed sequences.
Materials and methods
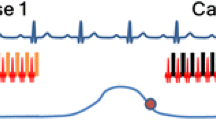
This study was approved by the institutional review board with informed consent obtained from all subjects. Study subjects included 31 pediatric patients (19 male, 12 female; median age: 5 years; interquartile range: 5 years) undergoing abdominal MRI at 3 tesla with a free-breathing T1-weighted radial stack-of-stars 3-D VIBE Dixon prototype sequence, StarVIBE Dixon (radial technique), between October 2018 and June 2019 with previous abdominal MR imaging using conventional Cartesian T1-weighed imaging (traditional technique). MRI component times were recorded as well as the total number of non-contrast T1-weighted sequences. Two radiologists independently rated images for quality using a scale from 1 to 5 according to the following metrics: overall image quality, hepatic edge sharpness, hepatic vessel clarity and respiratory motion robustness. Scores were compared between the groups.
Results
Mean T1-weighted imaging times for all subjects were 3.63 min for radial exams and 8.01 min for traditional exams (P<0.001), and total non-contrast imaging time was 32.7 min vs. 43.9 min (P=0.002). Adjusted mean total MRI time for all subjects was 60.2 min for radial exams and 65.7 min for traditional exams (P=0.387). The mean number of non-contrast T1-weighted sequences performed in radial MRI exams was 1.0 compared to 1.9 (range: 0–6) in traditional exams (P<0.001). StarVIBE Dixon outperformed Cartesian methods in all quality metrics. The mean overall image quality (scale 1–5) was 3.95 for radial exams and 3.31 for traditional exams (P<0.001).
Conclusion
Radial stack-of-stars 3-D VIBE Dixon during free-breathing abdominal MRI in pediatric patients offers improved image quality compared to Cartesian T1-weighted imaging techniques with decreased T1-weighted and total non-contrast imaging time. This has important implications for children undergoing sedation for imaging.


Similar content being viewed by others
References
Chavhan GB, Babyn PS, Vasanawala SS (2013) Abdominal MR imaging in children: motion compensation, sequence optimization, and protocol organization. Radiographics 33:703–719
Michael R (2008) Potential of MR-imaging in the paediatric abdomen. Eur J Radiol 68:235–244
Vasanawala SS, Iwadate Y, Church DG et al (2010) Navigated abdominal T1-W MRI permits free-breathing image acquisition with less motion artifact. Pediatr Radiol 40:340–344
Jaimes C, Kirsch JE, Gee MS (2018) Fast, free-breathing and motion-minimized techniques for pediatric body magnetic resonance imaging. Pediatr Radiol 48:1197–1208
Darge K, Anupindi SA, Jaramillo D (2011) MR imaging of the abdomen and pelvis in infants, children, and adolescents. Radiology 261:12–29
Rofsky NM, Lee VS, Laub G et al (1999) Abdominal MR imaging with a volumetric interpolated breath-hold examination. Radiology 212:876–884
Akisik FM, Sandrasegaran K, Aisen AM et al (2007) Abdominal MR imaging at 3.0 T. Radiographics 27:1433–1444
Azevedo RM, de Campos ROP, Ramalho M et al (2011) Free-breathing 3D T1-weighted gradient-echo sequence with radial data sampling in abdominal MRI: preliminary observations. AJR Am J Roentgenol 197:650–657
Young PM, Brau AC, Iwadate Y et al (2010) Respiratory navigated free-breathing 3D spoiled gradient-recalled echo sequence for contras-enhanced examination of the liver: diagnostic utility and comparison with free breathing and breath-hold conventional examinations. AJR Am J Roentgenol 195:687–691
Chandarana H, Block KT, Rosenkrantz AB et al (2011) Free-breathing radial 3D fat-suppressed T1-weighted gradient echo sequence. Invest Radiol 46:648–653
Block KT, Chandarana H, Milla S et al (2014) Towards routine clinical use of radial stack-of-stars 3D gradient-echo sequences for reducing motion sensitivity. J Korean Soc Magn Reson Med 18:87–106
Chandarana H, Block KT, Winfield MJ et al (2014) Free-breathing contrast-enhanced T1-weighted gradient-echo imaging with radial k-space sampling for paediatric abdominopelvic MRI. Eur Radiol 24:320–326
Balza R, Jaimes C, Risacher S et al (2019) Impact of a fast free-breathing 3T abdominal MRI protocol on improving scan time and image quality for pediatric patients with tuberous sclerosis complex. Pediatr Radiol 49:1788–1797
Dixon WT (1984) Simple proton spectroscopic imaging. Radiology 153:189–194
Ichikawa S, Motosugi U, Kromrey M-L et al (2020) Utility of stack-of-stars acquisition for hepatobiliary phase imaging without breath-holding. Magn Reson Med Sci 19:99–107
SAS Institute Inc (2015) SAS/STAT 14.1 User Guide. SAS Institute, Inc., Cary, NC
Fitzmaurice GM, Laird NM, Ware JH (2011) Applied longitudinal analysis, 2nd edn. Wiley, Hoboken, New Jersey
Lin L (2012) Statistical tools for measuring agreement. Springer, New York
Fleiss J (1981) Statistical methods for rates and proportions, 2nd edn. Wiley, New York
Agresti A (2013) Categorical data analysis, 3rd edn. John Wiley & Sons, Hoboken, New Jersey
Uebersax J (1987) Diversity of decision-making models and the measurement of interrater agreement. Psychol Bull 101:140–146
Callahan MJ, MacDougall RD, Bixby SD et al (2018) Ionizing radiation from computed tomography versus anesthesia for magnetic resonance imaging in infants and children: patient safety considerations. Pediatr Radiol 48:21–30
Low RN, Francis IR, Herfkens RJ et al (1993) Fast multiplanar spoiled gradient-recalled imaging of the liver: pulse sequence optimization and comparison with spin-echo MR imaging. AJR Am J Roentgenolog 160:501–509
Pipe JG (1999) Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 42:963–969
Hirokawa Y, Isoda H, Maetani YS et al (2008) MRI artifact reduction and quality improvement in the upper abdomen with PROPELLER and prospective acquisition correction (PACE) technique. AJR Am J Roentgenol 191:1154–1158
Bayramoglu S, Kilickesmez O, Cimilli T et al (2010) T2-weighted MRI of the upper abdomen: comparison of four fat-suppressed T2-weighted sequences including PROPELLER (BLADE) technique. Acad Radiol 17:368–374
Shin HJ, Kim M-J, Lee M-J, Kim HG (2016) Comparison of image quality between conventional VIBE and radial VIBE in free-breathing paediatric abdominal MRI. Clin Radiol 71:1044–1049
Kaltenbach B, Roman A, Polkowski C et al (2017) Free-breathing dynamic liver examination using a radial 3D T1-weighted gradient echo sequence with moderate undersampling for patients with limited breath-holding capacity. Eur J Radiol 86:26–32
Zhong X, Hu HH, Armstrong T et al (2020) Free-breathing volumetric liver R 2 * and proton density fat fraction quantification in pediatric patients using stack-of-radial MRI with self-gating motion compensation. J Magn Reson Imaging 53:118–129
Armstrong T, Ly KV, Ghahremani S et al (2019) Free-breathing 3-D quantification of infant body composition and hepatic fat using a stack-of-radial magnetic resonance imaging technique. Pediatr Radiol 49:876–888
Armstrong T, Ly KV, Murthy S et al (2018) Free-breathing quantification of hepatic fat in healthy children and children with nonalcoholic fatty liver disease using a multi-echo 3-D stack-of-radial MRI technique. Pediatr Radiol 48:941–953
Armstrong T, Dregely I, Stemmer A et al (2018) Free-breathing liver fat quantification using a multiecho 3D stack-of-radial technique. Magn Reson Med 79:370–382
Machado-Rivas F, Leitman E, Jaimes C et al (2020) Predictors of anesthetic exposure in pediatric MRI. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.20.23601
Cravero JP, Blike GT, Beach M et al (2006) Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: report from the pediatric sedation research consortium. Pediatrics 118:1087–1096
Cravero JP, Beach ML, Blike GT et al (2009) The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: a report from the pediatric sedation research consortium. Anesth Analg 108:795–804
Acknowledgments
The research reported in this publication was supported in part by the National Institute of Biomedical Imaging and Bioengineering for the National Institutes of Health under award number R01EB019483.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Alto Stemmer works for Siemens Healthineers.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duffy, P.B., Stemmer, A., Callahan, M.J. et al. Free-breathing radial stack-of-stars three-dimensional Dixon gradient echo sequence in abdominal magnetic resonance imaging in sedated pediatric patients. Pediatr Radiol 51, 1645–1653 (2021). https://doi.org/10.1007/s00247-021-05054-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05054-3