Abstract
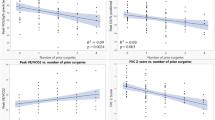
Congenital heart disease (CHD) is a common chronic disease. This study aimed to verify the relationship between spirometry and exercise capacity in children, considering the CHD severity. All cardiopulmonary exercise testing (CPET) and Spirometry from CHD children (5–18 years) were retrospectively reviewed during three years. CPET and Spirometry were analyzed and correlated based on the CHD severity[modified Ross classification (mR)]. Patients (n = 321) were analyzed and subdivided for CHD severity (n = 49, n = 149, n = 80, n = 43, from mR1 to mR4, respectively). The maximal workload (Wmax) in mR1 and mR2 was higher than in patients from mR3 and mR4. Peak oxygen uptake (peak VO2) was reduced in mR3 and mR4 compared to mR1 and mR2. Carbon dioxide output was only significantly lower in mR4. Although spirometric parameters were globally in the normal range, forced expiratory volume and forced vital capacity were different between subgroups (p < 0.001 and p = 0.002, respectively). Wmax and peakVO2 were weakly or moderately but significantly correlated with spirometry. Respiratory exchange ratio and final blood oxygen saturation were only significantly and weakly correlated to obstruction in small airways. The most severe CHD patients had lower exercise capacity and lung function parameters. A weak to moderate correlation between CPET and spirometry was found. However, the lung function reported in our study was normal, but with a negative correlation with the age. It reinforces the benefits of precocious and regularly spirometry and CPET assessment in CHD children.

Similar content being viewed by others
References
Tikkanen AU, Oyaga AR, Riaño OA, Álvaro EM, Rhodes J (2012) Paediatric cardiac rehabilitation in congenital heart disease: a systematic review. Cardiol Young 22(03):241–250
Rhodes J, Ubeda T, Jenkins KJ (2010) Exercise testing and training in children with congenital heart disease. Circulation 122(19):1957–1967
Amedro P, Picot MC, Moniotte S et al (2015) Correlation between cardio-pulmonary exercise test variables and health-related quality of life among children with congenital heart diseases. Int J Cardiol 203:1052–1060
Baumgartner H, Bonhoeffer P, De Groot NMS et al (2010) ESC Guidelines for the management of grown-up congenital heart disease. Eur Heart J 31(23):2915–2957
Barron A, Francis DP, Mayet J et al (2016) Oxygen uptake efficiency slope and breathing reserve, not anaerobic threshold, discriminate between patients with cardiovascular disease over chronic obstructive pulmonary disease. JACC Heart Fail 4(4):252–261
Myers J, Arena R, Dewey F et al (2008) A cardiopulmonary exercise testing score for predicting outcomes in patients with heart failure. Am Heart J 156(6):1177–1183
Taylor C, Nichols S, Ingle L (2015) A clinician’s guide to cardiopulmonary exercise testing 1: an introduction. Br J Hsopital Med 76(4):192–196
Longmuir PE, Brothers JA, De Ferranti SD et al (2013) Promotion of physical activity for children and adults with congenital heart disease: a scientific statement from the American Heart Association. Circulation 127(21):2147–2159
Gomes-Neto M, Saquetto MB (2015) Impact of exercise training in aerobic capacity and pulmonary function in children and adolescents after congenital heart disease surgery: a systematic review with meta-analysis. Pediatr Cardiol 37:217–224
Dulfer K, Helbing WA, Duppen N, Utens EM (2014) Associations between exercise capacity, physical activity, and psychosocial functioning in children with congenital heart disease: a systematic review. Eur J Prev Cardiol 21(10):1200–1215
Duppen N, Takken T, Hopman MTE et al (2013) Systematic review of the effects of physical exercise training programmes in children and young adults with congenital heart disease. Int J Cardiol 168(3):1779–1787
Hawkins SMM, Taylor AL, Sillau SH, Mitchell MB, Rausch CM (2014) Restrictive lung function in pediatric patients with structural congenital heart disease. J Thorac Cardiovasc Surg 148(1):207–211
Zaqout M, De Baets F, Schelstraete P et al (2010) Pulmonary function in children after surgical and percutaneous closure of atrial septal defect. Pediatr Cardiol 31(8):1171–1175
Giannico S, Hammad F, Amodeo A et al (2006) Clinical outcome of 193 extracardiac fontan patients. The first 15 years. J Am Coll Cardiol 47(10):2065–2073
Healy F, Hanna BD, Zinman R (2012) Pulmonary complications of congenital heart disease. Paediatr Respir Rev 13(1):10–15
Hancox RJ, Rasmussen F (2018) Does physical fitness enhance lung function in children and young adults? Eur Respir J 51(2):1701374
Takken T, Blank a CC, Hulzebos EHH, van Brussel M, Groen WGG, Helders PJJ (2009) Cardiopulmonary exercise testing in congenital heart disease: (contra)indications and interpretation. Neth Heart J 17(10):385–392
Beaver WL, Wasserman K, Whipp B (1986) A new method for detecting anaerobic threshold by gas exchange. Am Physiol Soc 60:2020–2027
Baba R, Nagashima M, Goto M et al (1996) Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol 28(6):1567–1572
Bongers BC, Hulzebos HJ,. van Brussel C, Takken M, Blank AT (2011) The oxygen uptake efficiency slope in children with congenital heart disease: construct and group validity. Eur J Cardiovasc Prev Rehabil 18(April):384–392
Giardini A, Specchia S, Gargiulo G, Sangiorgi D, Picchio FM (2009) Accuracy of oxygen uptake efficiency slope in adults with congenital heart disease. Int J Cardiol 133(1):74–79
Cooper D, Berry C, Lamarra N, Wasserman K (1985) Kinetics of oxygen uptake and heart rate at onset of exercise in children. J Appl Physiol 59(1):211–217
Cooper DM, Weiler-Ravell D, Whipp BJ, Wasserman K (1984) Growth-related changes in oxygen uptake and heart rate during progressive exercise in children. Pediatr Res 18:845
Cooper D, Weiler-Ravell D, Whipp B, Wasserman K (1984) Aerobic parameters of exercise as a function of body size during growth in children. J Appl Physiol Respir Env Exerc Physiol 56(3):628–634
Zapletal A, Motoyama EK, Van DeWoestijne KP, Hunt VR, Bouhuys A (1969) Maximum expiratory flow-volume curves and airway conductance in children and adolescents. J Appl Physiol 26:308–316
Quanjer PH, Stanojevic S, Cole TJ et al (2012) Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 40(6):1324–1343
Hinton RB, Ware SM (2017) Heart failure in pediatric patients with congenital heart disease. Circ Res 120(6):978–994
Ross RD, Bollinger RO, Pinsky WW (1992) Grading the severity of congestive heart failure in infants. Pediatr Cardiol 13(2):72–75
Singh AK, Patel N, Leung K, Patel P, Talwar A (2013) Manifestation of pulmonary disease in adults with CHD. Indian J Chest Dis Allied Sci 55(516):85–95
Uzark K, Jones K, Slusher J, Limbers C, Burwinkle TM, Varni JW (2008) Quality of life in children with heart disease as perceived by children and parents. Pediatrics 121(5):e1060–e1067
Houyel L, Khoshnood B, Anderson RH et al (2011) Population-based evaluation of a suggested anatomic and clinical classification of congenital heart defects based on the International Paediatric and Congenital Cardiac Code. Orphanet J Rare Dis 6(1):64
Jayaprasad N (2016) Heart failure in children. Hear Views 17(3):92–99
Muller J, Bohm B, Semsch S, Oberhoffer R, Hess J, Hager A (2013) Currently, children with congenital heart disease are not limited in their submaximal exercise performance. Eur J Cardio-Thoracic Surg 43(6):1096–1100
Voss C, Duncombe SL, Dean PH, de Souza AM, Harris KC (2017) Physical activity and sedentary behavior in children with congenital heart disease. J Am Heart Assoc 6(3):1–11
Hirth A, Reybrouck T, Bjarnason-Wehrens B, Lawrenz W, Hoffmann A (2006) Recommendations for participation in competitive and leisure sports in patients with congenital heart disease: a consensus document. Eur J Cardiovasc Prev Rehabil 13(3):293–299
Takken T, Giardini A, Reybrouck T et al (2012) Recommendations for physical activity, recreation sport, and exercise training in paediatric patients with congenital heart disease: a report from the Exercise, Basic & Translational Research Section of the European Association of Cardiovascular Prevention and Rehabilitation, the European Congenital Heart and Lung Exercise Group, and the Association for European Paediatric Cardiology. Eur J Prev Cardiol 19(5):1034–1065
Westhoff-bleck M, Treptau J, Löffler F (2015) Exercise training in adults with complex congenital heart disease. Ann Sport Med Res 2(6):1037
Rhodes J, Curran TJ, Camil L et al (2005) Impact of cardiac rehabilitation on the exercise function of children with serious congenital heart disease. Pediatrics 116(6):1339–1345
Turquetto ALR, Canêo LF, Agostinho DR et al (2017) Impaired pulmonary function is an additional potential mechanism for the reduction of functional capacity in clinically stable fontan patients. Pediatr Cardiol 38(5):981–990
Alonso-Gonzalez R, Borgia F, Diller GP et al (2013) Abnormal lung function in adults with congenital heart disease: prevalence, relation to cardiac anatomy, and association with survival. Circulation 127(8):882–890
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that we have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morales Mestre, N., Reychler, G., Goubau, C. et al. Correlation Between Cardiopulmonary Exercise Test, Spirometry, and Congenital Heart Disease Severity in Pediatric Population. Pediatr Cardiol 40, 871–877 (2019). https://doi.org/10.1007/s00246-019-02084-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02084-5