Abstract
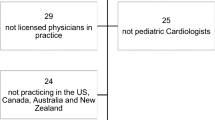
Atrial septal defect (ASD) is a common congenital heart defect. Variability in management of this lesion exists among clinicians. A review of the literature reveals that there is lack of standard guidelines for the evaluation and management of patients with different types of ASDs. This survey-based study was conducted to test the uniformity of diagnostic and therapeutic approach to management of children with secundum, sinus venosus, and primum ASDs. Survey questionnaires were prepared to include questions regarding follow-up, diagnosis, and therapeutic intervention of different types and sizes of ASDs. Questions addressed follow-up visitations, type and frequency of investigative studies, pharmacological therapy, and choice of repair method. Surveys were sent out to all pediatric cardiology academic programs in the United States (n=48) and randomly selected international programs from Europe, Asia, and Australia (n=19). A total of 23 programs (34%) responded to the survey (15 from the United States and 8 internationally). A separate questionnaire was prepared for secundum, primum, and sinus venosus ASD. In each questionnaire, lesion types were subdivided into small, moderate, and large defect sizes to address differences of management approaches to each defect type and size. Results indicate that in secundum ASD, most participants use size of the defect and/or evidence of right-sided volume overload as criteria for defining small, moderate, and large defects. Frequency of follow-up does not vary with the type of lesion but is more frequent with larger defects. Most participants see patients with small defects at intervals of 6 months to 1 year and those with large defects at 3- to 6-month intervals. Age of patient and presence of symptoms determined the frequency of follow-up across all defects. Echocardiography was the most frequently used investigative modality in all defect sizes and types during follow-up visits (used by >80% for follow-up), followed by electrocardiography (ECG). There is a striking preference for the use of pharmacological therapy in primum ASD compared with secundum and sinus venosus ASD. The timing of repair was mainly dependent on patient age and symptomatology in different defects, with the presence of associated anomalies contributing to that in primum and sinus venosus ASD. Most participants use percutaneous approach to close secundum ASD (either as a first choice or as one of two choices depending on the presence of certain features). Before repair, participants use MRI or cardiac catheterization to fully evaluate a secundum ASD if it is large. These investigative modalities are not commonly used in primum and sinus venosus ASD. There is agreement on postoperative follow-up in different types of defects, with most participants continuing follow-up indefinitely, especially in larger defects.



Similar content being viewed by others
References
Al-Bustami O, Sharifi M, Hijazi Z, et al. (2005) Necessity for evaluation of anomalous pulmonary venous return before percutaneous closure of atrial septal defects. Angiology 56(0):T1–T4
Agrawal S, Khanna S, Tampe D (1997) Sinus venosus atrial septal defects: surgical follow-up. Eur J Cardio-thorac Surg 11:455–457
Angy M, Cobanoglu A (1999) Repair of partial atrioventricular septal defect in children less than five years of age: late results. Ann Thorac Surg 67:1412–1414
Attenhofer Jost C, Connolly H, Danielson G, et al. (2005) Sinus venosus atrial septal defect; long-term postoperative outcome for 115 patients. Circulation 112:1953–1958
Beerbaum P, Körperich H, Esdorn H, et al. (2003) Atrial septal defects in pediatric patients: noninvasive sizing with cardiovascular MR imaging. Radiology 228:361–369
Berger F, Ewert P, Björnstad P, et al. (1999) Transcatheter closure as standard treatment for most interatrial defects: experience in 200 patients treated with the Amplatzer Septal Occluder. Cardiol Young 9(5):468–473
Brassard M, Fouron J, van Doesburg N, et al. (1999) Outcome of children with atrial septal defect considered too small for surgical closure. Am J Cardiol 83:1552–1555
Burke R, Horvath K, Landzberg M, et al. (1996) Long-term follow-up after surgical repair of ostium primum atrial septal defect in adults. J Am Coll Cardiol 27(3):696–699
Campbell M (1970) Natural history of atrial septal defect. Br Heart J 32(6):820–826
Du Z, Hijazi Z, Kleinman C, et al. (2002) Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults. J Am Coll Cardiol 39(11):1836–1844
El-Najdawi E, Driscoll D, Puga F, et al. (2000) Operation for partial atrioventricular septal defect: a forty-year review. J Thorac Cardiovasc Surg 119(5):880–890
Hausdorf G, Schneider M, Franzbach B, et al. (1996) Transcatheter closure of secundum atrial septal defects with the atrial septal defect occlusion system (ASDOS): initial experience in children. Heart 75:83–88
Hein R, Büscheck F, Fisher E, et al. (2005) Atrial and ventricular septal defects can safely be closed by percutaneous intervention. J Interv Cardiol 18:515–522
Helber U, Baumann R, Seboldt H, et al. (1997) Atrial septal defects in adults: cardiopulmonary exercise capacity before and 4 months and 10 years after defect closure. J Am Coll Cardiol 29(6):1345–1350
Helgason H, Jonsdottir G (1999) Spontaneous closure of atrial septal defects. Pediatr Cardiol 20:195–199
Hughes M, Maskell G, Goh T, et al. (2002) Prospective comparison of costs and short term health outcomes of surgical versus device closure of atrial septal defect in children. Heart 88(1):67–70
Hunt C, Lucas R (1972) Symptomatic atrial septal defects in infancy. Circulation 47:1042–1048
Ivan Dimich, Steinfeld L, Park S (1973) Symptomatic atrial septal defects in infants. Am Heart J 85(5):601–604
Kim J, Hijazi ZM (2002) Clincial outcomes and costs of Amplatzer transcatheter closure as compared with surgical closure of ostium secundum atrial septal defects. Med Sci Monit 8:787–791
Khalid O, Luxenberg DM, Sable C, et al. (2006) Aortic stenosis: spectrum of care. Pediatr Cardiol 27:661–669
King M, Puga F, Danielson G, et al. (1986) Prognostic factors and surgical treatment of partial atrioventricular canal. Circulation 74(Suppl I):I42–I46
Kostantinides S, Giebel A (1995) A comparison of surgical and medical therapy for atrial septal defects in adults. N Engl J Med 333:469–473
Manning P, Mayer J, Sanders S, et al. (1994) Unique features and prognosis of primum ASD Presenting in the first year of life. Circulation 90(5):30–35
Matthewson J, Bichell D, Rothman A, et al. (2004) Absent posteroinferior and anterosuperior atrial septal defect rims: factors affecting nonsurgical closure of large secundum defects using the Amplatzer occluder. J Am Soc Echocardiogr 17(1):62–69
McMahon C, Feltes T, Fraley J, et al. (2002) Natural history of growth of secundum atrial septal defects and implications for transcatheter closure. Heart 87:256–259
Murphy J, Gersh B, McGoon M, et al. (1990) Long-term outcome after surgical repair of isolated atrial septal defect. Follow up at 27 to 32 years. N Engl J Med 323:1645–1650
Otsuka M, Itoh A, Haze K (2003) Sinus venosus type of atrial septal defect with partial anomalous pulmonary venous return evaluated by multislice CT. Heart 91(8):901
Omeish A, Hijazi ZM (2001) Transcatheter closure of atrial septal defects in children & adults using the Amplatzer Septal Occluder. J Interv Cardiol 14:37–44
Pascoe R, Warnes C, Danielson G (1996) Heart disease in the young: diagnosis of sinus venosus atrial septal defect with transesophageal echocardiography. Circulation 94(5):1049–1055
Portman M, Beder S, Ankeney J, et al. (1985) A 20 year review of ostium primum defect repair in children. Am Heart J 110(5):1054–1058
Radzik D, Davignon A, van Doesburg N, et al. (1994) Predictive factors for spontaneous closure of atrial septal defects diagnosed in the first 3 months of life. J Am Coll Cardiol 23(3):851–853
Russell J, LeBlanc J, Deagle M, et al. (2002) Outcome following repair of sinus venosus atrial septal defects in children. Asian Cardiovasc Thorac Ann 10(3):231–234
Shah D, Azhar M, Oakley C, et al. (1994) Natural history of secundum atrial septal defect in adults after medical or surgical treatment: a historical prospective study. Br Heart J 71(3):224–227
Somerville J (1965) Ostium primum defect: factors causing deterioration in the natural history. Br Heart J 27:413–416
Thilén U, Berlind S, Varnauskas E (2000) Atrial septal defects in adults. Thirty eight years of follow up of a surgically and a conservatively managed group. Scand Cardiovasc J 34:79–83
Thomson J, Aburawi E, Watterson K, et al. (2002) Surgical and transcatheter (Amplatzer) closure of atrial septal defects: a prospective comparison of results and cost. Heart 87(5):466–469
Van Praagh S, Carrera M, Sanders S, et al. (1994) Sinus venosus defects: unroofing of the right pulmonary veins—anatomic and echocardiographic findings and surgical treatment. Am Heart J 128(2):365–379
Vincent R, Raviele A, Diehl H (2003) Single-center experience with the Helex septal occluder for closure of atrial septal defects in children. J Interv Cardiol 16(1):79–82
Visconti K, Bichell D, Jonas R, et al. (1999) Developmental outcome after surgical versus interventional closure of secundum atrial septal defect in children. Circulation 100(19):II-145–II-150
Vogel M, Berger F, Kramer A, et al. (1999) Incidence of secondary pulmonary hypertension in adults with atrial septal or sinus venosus defects. Heart 82:30–33
Wang J, Tsai S, Wu M, et al. (2004) Short- and intermediate-term results of transcatheter closure of atrial septal defect with the Amplatzer septal occluder. Am Heart J 148:511–517
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kharouf, R., Luxenberg, D.M., Khalid, O. et al. Atrial Septal Defect: Spectrum of Care. Pediatr Cardiol 29, 271–280 (2008). https://doi.org/10.1007/s00246-007-9052-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-007-9052-8