Abstract
Purpose
The use of DSC-MR imaging in pediatric neuroradiology is gradually growing. However, the number of studies listed in the literature remains limited. We propose to assess the perfusion and permeability parameters in pediatric brain tumor grading.
Methods
Thirty children with a brain tumor having benefited from a DSC-MR perfusion sequence have been retrospectively explored. Relative CBF and CBV were computed on the ROI with the largest lesion coverage. Assessment of the lesion’s permeability was also performed through the semi-quantitative PSR parameter and the K2 model-based parameter on the whole-lesion ROI and a reduced ROI drawn on the permeability maps. A statistical comparison of high- and low-grade groups (HG, LG) as well as a ROC analysis was performed on the histogram-based parameters.
Results
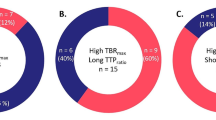
Our results showed a statistically significant difference between LG and HG groups for mean rCBV (p < 10-3), rCBF (p < 10-3), and for PSR (p = 0.03) but not for the K2 factor (p = 0.5). However, the ratio K2/PSR was shown to be a strong discriminating factor between the two groups of lesions (p < 10-3). For rCBV and rCBF indicators, high values of ROC AUC were obtained (> 0.9) and mean value thresholds were observed at 1.07 and 1.03, respectively. For K2/PSR in the reduced area, AUC was also superior to 0.9.
Conclusions
The implementation of a dynamic T2* perfusion sequence provided reliable results using an objective whole-lesion ROI. Perfusion parameters as well as a new permeability indicator could efficiently discriminate high-grade from low-grade lesions in the pediatric population.



Similar content being viewed by others
References
Koob M, Girard N (2014) Cerebral tumors: specific features in children. Diagn Interv Imaging 95:965–983. https://doi.org/10.1016/j.diii.2014.06.017
Arvinda HR, Kesavadas C, Sarma PS, Thomas B, Radhakrishnan VV, Gupta AK, Kapilamoorthy TR, Nair S (2009) Glioma grading: sensitivity, specificity, positive and negative predictive values of diffusion and perfusion imaging. J Neuro-Oncol 94:87–96. https://doi.org/10.1007/s11060-009-9807-6
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol (Berl) 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol (Berl) 114:97–109. https://doi.org/10.1007/s00401-007-0243-4
Combaz X, Girard N, Scavarda D, Chapon F, Pineau S, Levrier O, Viout P, Confort-Gouny S (2008) Imagerie des tumeurs cérébrales de l’enfant. J Neuroradiol 35:261–267. https://doi.org/10.1016/j.neurad.2008.03.004
Rickert C, Paulus W (2001) Epidemiology of central nervous system tumors in childhood and adolescence based on the new WHO classification. Childs Nerv Syst 17:503–511. https://doi.org/10.1007/s003810100496
Allen ED, Byrd SE, Darling CF, Tomita T, Wilczynski MA (1993) The clinical and radiological evaluation of primary brain neoplasms in children, part II: radiological evaluation. J Natl Med Assoc 85:546
Bjornerud A, Sorensen AG, Mouridsen K, Emblem KE (2011) T1- and T*2-dominant extravasation correction in DSC-MRI: part I—theoretical considerations and implications for assessment of tumor hemodynamic properties. J Cereb Blood Flow Metab 31:2041–2053
Donahue KM, Krouwer HG, Rand SD, Pathak AP, Marszalkowski CS, Censky SC, Prost RW (2000) Utility of simultaneously acquired gradient-echo and spin-echo cerebral blood volume and morphology maps in brain tumor patients. Magn Reson Med 43:845–853
Boxerman JL, Schmainda KM, Weisskoff RM (2006) Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. Am J Neuroradiol 27:859–867
Bouzerar R, Chaarani B, Gondry-Jouet C, Zmudka J, Balédent O (2013) Measurement of choroid plexus perfusion using dynamic susceptibility MR imaging: capillary permeability and age-related changes. Neuroradiology 55:1447–1454. https://doi.org/10.1007/s00234-013-1290-2
Tzika AA, Zarifi MK, Goumnerova L, Astrakas LG, Zurakowski D, Young-Poussaint T, Anthony DC, Scott RM, Black PM (2002) Neuroimaging in pediatric brain tumors: Gd-DTPA–enhanced, hemodynamic, and diffusion MR imaging compared with MR spectroscopic imaging. Am J Neuroradiol 23:322–333
Cha S (2006) Dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging in pediatric patients. Neuroimaging Clin N Am 16:137–147. https://doi.org/10.1016/j.nic.2005.11.006
Ho CY, Cardinal JS, Kamer AP, Kralik SF (2015) Relative cerebral blood volume from dynamic susceptibility contrast perfusion in the grading of pediatric primary brain tumors. Neuroradiology 57:299–306. https://doi.org/10.1007/s00234-014-1478-0
Ho CY, Cardinal JS, Kamer AP, Lin C, Kralik SF (2016) Contrast leakage patterns from dynamic susceptibility contrast perfusion MRI in the grading of primary pediatric brain tumors. Am J Neuroradiol 37:544–551. https://doi.org/10.3174/ajnr.A4559
Law M, Young R, Babb J, Pollack E, Johnson G (2007) Histogram analysis versus region of interest analysis of dynamic susceptibility contrast perfusion MR imaging data in the grading of cerebral gliomas. Am J Neuroradiol 28:761–766
Mangla R, Kolar B, Zhu T, Zhong J, Almast J, Ekholm S (2011) Percentage signal recovery derived from MR dynamic susceptibility contrast imaging is useful to differentiate common enhancing malignant lesions of the brain. Am J Neuroradiol 32:1004–1010. https://doi.org/10.3174/ajnr.A2441
Bewick V, Cheek L, Ball J (2004) Statistics review 13: receiver operating characteristic curves. Crit Care 8:508
Paulson ES, Schmainda KM (2008) Comparison of dynamic susceptibility-weighted contrast-enhanced MR methods: recommendations for measuring relative cerebral blood volume in brain tumors 1. Radiology 249:601–613
Leu K, Boxerman JL, Ellingson BM (2017) Effects of MRI protocol parameters, preload injection dose, fractionation strategies, and leakage correction algorithms on the Fidelity of dynamic-susceptibility contrast MRI estimates of relative cerebral blood volume in gliomas. Am J Neuroradiol 38:478–484. https://doi.org/10.3174/ajnr.A5027
Jiang J, Zhao L, Zhang Y, Zhang S, Yao Y, Qin Y, Wang C-Y, Zhu W (2014) Comparative analysis of arterial spin labeling and dynamic susceptibility contrast perfusion imaging for quantitative perfusion measurements of brain tumors. Int J Clin Exp Pathol 7:2790
Cebeci H, Aydin O, Ozturk-Isik E, Gumus C, Inecikli F, Bekar A, Kocaeli H, Hakyemez B (2014) Assesment of perfusion in glial tumors with arterial spin labeling; comparison with dynamic susceptibility contrast method. Eur J Radiol 83:1914–1919. https://doi.org/10.1016/j.ejrad.2014.07.002
Khashbat Md D, Abe Md T, Ganbold Md M, Iwamoto Md S, Uyama Md N, Irahara Md S, Otomi Md PhD Y, Harada Md PhD M, Kageji Md PhD T, Nagahiro Md PhD S (2016) Correlation of 3D arterial spin labeling and multi-parametric dynamic susceptibility contrast perfusion MRI in brain tumors. J Med Investig JMI 63:175–181. https://doi.org/10.2152/jmi.63.175
Yun TJ, Sohn C-H, Han MH, Kang H-S, Kim JE, Yoon B-W, Paeng JC, Choi SH, Kim J, Song IC, Chang K-H (2013) Effect of delayed transit time on arterial spin labeling: correlation with dynamic susceptibility contrast perfusion magnetic resonance in moyamoya disease. Investig Radiol 48:795–802. https://doi.org/10.1097/RLI.0b013e3182981137
Williams DS, Detre JA, Leigh JS, Koretsky AP (1992) Magnetic resonance imaging of perfusion using spin inversion of arterial water. Proc Natl Acad Sci 89:212–216
Yeom KW, Mitchell LA, Lober RM, Barnes PD, Vogel H, Fisher PG, Edwards MS (2014) Arterial spin-labeled perfusion of pediatric brain tumors. Am J Neuroradiol 35:395–401. https://doi.org/10.3174/ajnr.A3670
Dangouloff-Ros V, Deroulers C, Foissac F, Badoual M, Shotar E, Grévent D, Calmon R, Pagès M, Grill J, Dufour C, others (2016) Arterial spin labeling to predict brain tumor grading in children: correlations between histopathologic vascular density and perfusion MR imaging. Radiology 281:553–566
Gevers S, Van Osch MJ, Bokkers RP, Kies DA, Teeuwisse WM, Majoie CB, Hendrikse J, Nederveen AJ (2011) Intra-and multicenter reproducibility of pulsed, continuous and pseudo-continuous arterial spin labeling methods for measuring cerebral perfusion. J Cereb Blood Flow Metab 31:1706–1715
Wintermark M, Lepori D, Cotting J, Roulet E, van Melle G, Meuli R, Maeder P, Regli L, Verdun FR, Deonna T, others (2004) Brain perfusion in children: evolution with age assessed by quantitative perfusion computed tomography. Pediatrics 113:1642–1652
Van Gelderen P, de Zwart JA, Duyn JH (2008) Pitfalls of MRI measurement of white matter perfusion based on arterial spin labeling. Magn Reson Med 59:788–795. https://doi.org/10.1002/mrm.21515
Boxerman JL, Paulson ES, Prah MA, Schmainda KM (2013) The effect of pulse sequence parameters and contrast agent dose on percentage signal recovery in DSC-MRI: implications for clinical applications. Am J Neuroradiol 34:1364–1369. https://doi.org/10.3174/ajnr.A3477
Lupo JM, Cha S, Chang SM, Nelson SJ (2005) Dynamic susceptibility-weighted perfusion imaging of high-grade gliomas: characterization of spatial heterogeneity. Am J Neuroradiol 26:1446–1454
Kassner A, Annesley DJ, Zhu XP, Li KL, Kamaly-Asl ID, Watson Y, Jackson A (2000) Abnormalities of the contrast re-circulation phase in cerebral tumors demonstrated using dynamic susceptibility contrast-enhanced imaging: a possible marker of vascular tortuosity. J Magn Reson Imaging JMRI 11:103–113
Kaisti KK, Langsjo JW, Aalto S, Oikonen V, Sipila H, Teras M, Hinkka S, Metsahonkala L, Scheinin H (2003) Effects of sevoflurane, propofol, and adjunct nitrous oxide on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology 99:603–613
Murat I, Dubois M-C, Piat V (1995) Le sévoflurane. Ann Francaises Anesth Réanimation 14:489–501
Laswad T, Wintermark P, Alamo L, Moessinger A, Meuli R, Gudinchet F (2009) Method for performing cerebral perfusion-weighted MRI in neonates. Pediatr Radiol 39:260–264. https://doi.org/10.1007/s00247-008-1081-9
Tanner SF, Cornette L, Ramenghi LA, Miall LS, Ridgway JP, Smith MA, Levene MI (2003) Cerebral perfusion in infants and neonates: preliminary results obtained using dynamic susceptibility contrast enhanced magnetic resonance imaging. Arch Fetal Neonatal 88:F525–F530. https://doi.org/10.1136/fn.88.6.F525
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of retrospective study formal consent is not required.
Rights and permissions
About this article
Cite this article
Dallery, F., Bouzerar, R., Michel, D. et al. Perfusion magnetic resonance imaging in pediatric brain tumors. Neuroradiology 59, 1143–1153 (2017). https://doi.org/10.1007/s00234-017-1917-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-017-1917-9