Abstract
Introduction
Scarce information about comparative diagnostic and therapeutic patterns in paediatric outpatients of different countries is found in the literature.
Objective
To describe the similarities and differences observed in diagnosis and therapeutic patterns of paediatric patients of seven locations in different countries.
Design
Cross-sectional, prospective, international comparative, descriptive study.
Patients and methods
A randomly selected sample of 12,264 paediatric outpatients seen in consultation rooms of urban and rural areas and attended by paediatricians or general practitioners of the participating locations. Data on patient demographic information, diagnosis and pharmacological treatment were collected using pre-designed forms. Diagnoses were coded using the ICD-9 and drugs according to the ATC classification.
Results
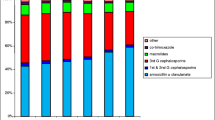
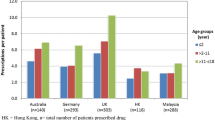
Among the ten most common diagnoses, upper respiratory tract infections are in the first position in all locations; asthma prevalence is highest in Tenerife (8.4%). Tonsillitis, otitis, bronchitis and dermatological affections are the most common diagnoses in all locations. Pneumonia is only reported in Sofia (3.8%) and Smolensk (2.3%). The average number of drugs prescribed per child varied from 1.3 in Barcelona to 2.9 in Smolensk. There are no great differences in the profile of pharmacological groups prescribed, but a considerable range of variations in antibiotic therapy is observed: prescription of cephalosporins is low in Smolensk (0.7%) and higher in the other locations, from 16.5% (Bratislava) to 28% (Tenerife). Macrolides prescriptions range from 12.6% (Toulouse) to 24.7% (Smolensk), except in Sofia where they drop to 5.6%. Trimethoprim and its combinations are used in Smolensk (23.3%), Sofia (11.8%) and Bratislava (8.7%). Check-up consultations are not recorded in Smolensk and Bratislava, whereas in Toulouse these visits account for 16.2% of all consultations and in the other locations the percentage varies from 6.1% (Tenerife) to 1.9% (Sofia). Homeopathic treatments are registered only in Toulouse.
Conclusion
Except in asthma prevalence, there are no great differences in diagnostic maps among locations. Significant variations in the number of drugs prescribed per child and antibiotic therapies are observed. Areas for improvement have been identified.


Similar content being viewed by others
Reference
Hong SH, Shepherd MD (1996) Outpatient prescription drug use by children enrolled in five drug benefit plans. Clin Ther 18:528–545
McCaig LF, Besser RE, Hughes JM (2002) Trends in antimicrobial prescribing rates for children and adolescents. JAMA 287:3096–3102
Vaccheri A, Castelvetri C, Esaka E, Del Favero A, Montanaro N (2000) Pattern of antibiotic use in primary health care in Italy. Eur J Clin Pharmacol 56:417–425
Nyquist AC, Gonzales R, Steiner JF, Sande MA (1998) Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 279:875–877
Dowell SF, Schwartz B, Phillips WR (1998) Appropriate use of antibiotics for URIs in children. Part I. Otitis media and acute sinusitis. The Pediatric URI Consensus Team. Am Fam Physician 58:1113–1123
Smucny J, Fahey T, Becker L, Glazier R, McIsaac W (2003) Antibiotics for acute bronchitis. Cochrane Database Syst Rev 4:CD000245
Glasziou PP, Hayem M, Del Mar CB (2003) Antibiotics for acute otitis media in children. Cochrane Database Syst Rev 2:CD000219
Cazzato T, Pandolfini C, Campi R, Bonati M (2001) Drug prescribing in out-patient children in Southern Italy. Eur J Clin Pharmacol 57:611–616
Wessling A, Soderman P, Boethius G (1991) Monitoring of drug prescriptions for children in the county of Jamtland and Sweden as a whole in 1977–1987. Acta Paediatr Scand 80:944–952
Collet JP, Bossard N, Floret D, Gillet J, Honegger D, Boissel JP (1991) Drug prescription in young children: results of a survey in France. Epicreche Research Group. Eur J Clin Pharmacol 41:489–491
Niclasen BV, Moller SM, Christensen RB (1995) Drug prescription to children living in the Arctic. An investigation from Nuuk, Greenland. Arctic Med Res 54[Suppl 1]:95–100
Thrane N, Sorensen HT (1999) A one-year population-based study of drug prescriptions for Danish children. Acta Paediatr 88:1131–1136
Madsen H, Andersen M, Hallas J (2001) Drug prescribing among Danish children: a population-based study. Eur J Clin Pharmacol 57:159–165
McCaig LF, Besser RE, Hughes JM (2002) Trends in antimicrobial prescribing rates for children and adolescents. JAMA 287:3096–3102
Sanz EJ (1998) Drug prescribing for children in general practice. Acta Paediatr 87:489–490
Sanz E (2001) Are antibiotics overprescribed in primary care? Acta Paediatr 90:1223–1225
Sanz EJ, Boada JN (1988) Drug utilization by children in Tenerife Island. Eur J Clin Pharmacol 34:495–499
Sanz EJ, Bergman U, Dahlstrom M (1989) Paediatric drug prescribing. A comparison of Tenerife (Canary Islands, Spain) and Sweden. Eur J Clin Pharmacol 37:65–68
Schindler C, Krappweis J, Morgenstern I, Kirch W (2003) Prescriptions of systemic antibiotics for children in Germany aged between 0 and 6 years. Pharmacoepidemiol Drug Saf 12:113–120
Cazzato T, Pandolfini C, Campi R, Bonati M (2001) Drug prescribing in out-patient children in Southern Italy. Eur J Clin Pharmacol 57:611–616
Pichichero ME (2002) Dynamics of antibiotic prescribing for children. JAMA 287:3133–3135
Pickering L, Georges P, Baker C, Gerber M, MacDonald N, Orenstein W et al (2000) Red book: report of the committee on infectious diseases. American Academy of Pediatrics, Illinois, p 25
Boccazzi A, Noviello S, Tonelli P, Coi P, Esposito S, Carnelli V (2002) The decision-making process in antibacterial treatment of pediatric upper respiratory infections: a national prospective office-based observational study. Int J Infect Dis 6:103–107
Chandran R (2001) Should we prescribe antibiotics for acute bronchitis? Am Fam Physician 64:135–138
Rautakorpi UM, Lumio J, Huovinen P, Klaukka T (1999) Indication-based use of antimicrobials in Finnish primary health care. Description of a method for data collection and results of its application. Scand J Prim Health Care 17:93–99
Kawamoto R, Asai Y, Nago N, Okayama M, Mise J, Igarashi M (1998) A study of clinical features and treatment of acute bronchitis by Japanese primary care physicians. Fam Pract 15:244–251
Straand J, Rokstad KS, Sandvik H (1998) Prescribing systemic antibiotics in general practice. A report from the More and Romsdal prescription study. Scand J Prim Health Care 16:121–127
Dosh SA, Hickner JM, Mainous AG III, Ebell MH (2000) Predictors of antibiotic prescribing for nonspecific upper respiratory infections, acute bronchitis, and acute sinusitis. An UPRNet study. Upper peninsula research network. J Fam Pract 49:407–414
Hueston WJ, Hopper JE, Dacus EN, Mainous AG III (2000) Why are antibiotics prescribed for patients with acute bronchitis? A postintervention analysis. J Am Board Fam Pract 13:398–402
Lee AC, Kemper KJ (2000) Homeopathy and naturopathy: practice characteristics and pediatric care. Arch Pediatr Adolesc Med 154:75–80
Calderon C (1998) Homeopathic and primary care doctors: how they see each other and how they see their patients: results of a qualitative investigation. Aten Primaria 21:367–375
Pedersen EJ, Norheim AJ, Fonnebe V (1996) Attitudes of Norwegian physicians to homeopathy. A questionnaire among 2019 physicians on their cooperation with homeopathy specialists. Tidsskr Nor Laegeforen 116:2186–2189
Sanz E (2003) Concordance and children’s use of medicines. BMJ 327:858–860
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanz, E., Hernández, M.A., Ratchina, S. et al. Drug utilisation in outpatient children. A comparison among Tenerife, Valencia, and Barcelona (Spain), Toulouse (France), Sofia (Bulgaria), Bratislava (Slovakia) and Smolensk (Russia). Eur J Clin Pharmacol 60, 127–134 (2004). https://doi.org/10.1007/s00228-004-0739-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-004-0739-y