Abstract
Objective
To investigate and compare drug prescription patterns in children admitted to a paediatric general medical ward in five countries.
Methods
A prospective cohort study conducted on paediatric medical wards in the UK, Germany, Australia, Hong Kong (HK) and Malaysia. Data were collected over 3 months in each country except in Australia (1 month). All medications prescribed were classified according to the WHO Anatomical Therapeutic Chemical (ATC) classification. For each drug, frequency of prescriptions and patient exposures were calculated for ATC anatomical and therapeutic levels overall and by country.
Results
One thousand two hundred and seventy-eight patients were included (Australia 146, Germany 376, UK 313, HK 143 and Malaysia 300); 89.2 % of patients (1140) received medications, median 3 (interquartile range 2–5) drugs per patient. 5367 drugs were prescribed. The most frequently prescribed therapeutic groups in all countries were: systemic antibacterials (1355; 25.2 %), analgesics/non-steroidal anti-inflammatory drugs (NSAIDs) (1173; 21.8 %) and drugs for obstructive airway diseases (472; 8.8 %). Overall, 65.1 % (742) of patients received at least one systemic antibacterial, 63.7 % (726) received one or more analgesic/NSAIDs, and 23.6 % (269) received ‘drugs for obstructive airway diseases’. The number of patients exposed to these groups differed significantly between countries (p < 0.05). Paracetamol was the most frequently prescribed in all countries, but metamizole was only used in Germany. Morphine was mainly prescribed in the UK.
Conclusion
This study provides an overview of drug use patterns in five culturally and ethnically diverse countries. The most frequently used therapeutic groups were similar, but the proportion of patients treated differed between countries. Also within a therapeutic group the specific drug used varied between countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The most utilised therapeutic groups in the participating countries were systemic antibacterials (25.2 %) and analgesics/NSAIDs (21.8 %); however, the use of specific drugs within a therapeutic group differed among countries. |
Prescription patterns varied among participating countries, which might be related to differences in treatment strategies or different clinical diagnoses of children in various parts of the world. |
1 Introduction
Drug utilisation is an important component of many research initiatives that examine the clinical and economic effectiveness of pharmacotherapy [1]. The World Health Organization (WHO) defines drug utilisation as “the marketing, distribution, prescription and use of drugs in a society, with special emphasis on the resulting medical, social and economic consequences” [2]. Thus, the goal of drug utilization research is to facilitate the rational use of drugs in populations, and provide evidence of prescribing patterns. Based on this evidence, measures may be recommended to improve prescribing behaviour.
Most of the previous drug utilisation studies on paediatric patients were conducted to describe how specific drugs or certain groups of drugs were used, for example, the prescribing trends with antimicrobials [3], antidiabetic drugs [4] and psychotropic drugs [5–7], or to evaluate how practice in children differed from the recommendations in the summary of product characteristics, adult dosing guidelines or hospital formularies [8, 9].
Sturkenboom et al. [10] have probably provided the most comprehensive overview of primary-care prescription patterns in a large multinational European paediatric population. This study found similarities between countries, e.g. children less than 2 years of age had the highest prescription rate, and also differences, e.g. prescription of nervous system drugs were higher in the UK compared to the other two countries. Another community setting study conducted in one million Canadian children showed that the drugs used and the rates of use were highly dependent on age [11]. However, there are limited international data available for comparison of secondary care prescription patterns in children. In most of the published studies to date different settings and different methods for data collection and analysis were used, which makes it difficult to compare the data [12–15].
Consequently, more systematic drug utilisation research is needed, particularly internationally for hospitalised children. We conducted a prospective, multicentre study, using a common protocol, standardised data collection methods and terminologies to describe and compare the drug prescription patterns in hospitalised children in a paediatric general medical ward in five countries, both European and non-European, with different cultures and ethnicity.
2 Methods
The findings presented are derived from secondary use of data collected in a previous study [16] conducted in 2008–2009; the study methodology has been reported previously [16] and the following is a brief summary.
A prospective multicentre cohort study was conducted in the paediatric general medical ward of a hospital in five countries: Australia, Germany, China [Hong Kong (HK)], Malaysia and the UK. Data were collected over a 3-month period in each country except Australia where it was collected for 1 month only due to resource limitations: Australia 10 November 2008–10 December 2008; Germany 15 October 2008–14 January 2009; UK 14 January 2009–14 April 2009; HK 15 August 2009–14 November 2009; Malaysia 1 April 2009–30 June 2009. Data were collected using a web-based data entry application designed specifically for this study. All children aged 0–18 years admitted to a paediatric general medical ward during the study period and who stayed for ≥24 h were included.
The data collected comprised patient demographics and drug prescription details including route of administration and reported diagnosis.
For standardisation the WHO Anatomical Therapeutic Chemical (ATC) classification system for medication was used by all participating hospitals [17]. WHO-ATC uses a hierarchical system for classifying medicines into distinct groups at five different levels according to the organ system which they act on and their therapeutic, pharmacological and chemical properties; anatomical main group (level 1), therapeutic subgroup (level 2), pharmacological subgroup (level 3), chemical subgroup (level 4),and chemical substance (level 5). The International Classification of Diseases version 10 (ICD 10) was used for classifying diagnoses [18].
2.1 Drug Prescriptions Details
All drugs prescribed for children during admission were collected from medication charts. This included all new medicines prescribed during admission as well as medicines the patient was taking prior to admission. Each prescribed drug and each chemical compound or combination of compounds, based on ATC classification, was considered only once per patient irrespective of whether the dose was changed or prescriptions were repeated during hospitalisation. Fluid and electrolyte infusions and total parenteral nutrition (TPN) were not documented. For the comparison between countries, we grouped the drug prescriptions based on various levels of the ATC classification system [17]. Routes of administration (e.g. oral, parenteral, topical or rectal) were recorded.
Drug prescriptions were stratified into three groups based on the number of prescribed drugs received per patient during their hospitalisation: 1–4, 5–10 and >10 drugs.
2.2 Drug Exposure
The percentage of patients exposed to a particular therapeutic group in the study cohort and in each country was calculated as the number of patients prescribed at least one drug in a particular therapeutic group with the total number of patients prescribed any drug in the study cohort and/or in each country cohort as the denominator. Also, patient exposure percentages were calculated for the following therapeutic groups: systemic antibacterials (J01), analgesics (N02), drugs for obstructive airway diseases (R03), anti-inflammatory and antirheumatic drugs (M01), systemic corticosteroids (H02), ‘blood substitutes and perfusions (B05)’, ‘drugs for acid-related disorders (A02)’, psycholeptics (N05), antiepileptics (N03) and laxatives (A06), because these were the most frequently prescribed therapeutic drug groups in this study. Because the usual use of an anti-inflammatory drug is as an analgesic, N02 (analgesic) and M01 (anti-inflammatory) were combined into one group (analgesics/NSAIDs) and patient exposure to this combined group was calculated.
2.3 Statistical Analysis
Statistical analyses were performed using Stata 11 (StataCorp, College Station, TX, USA). For descriptive analysis and differences between groups and countries, Chi-squared, Kruskal–Wallis rank and Wilcoxon rank-sum tests were used as appropriate. Significant differences were considered at p values <0.05.
The number of drugs prescribed per patient and drug exposures for the most frequently prescribed therapeutic drug groups were calculated in the overall study cohort and in each country.
Paediatric patients were grouped into three age groups (≤2, >2 to ≤11, >11 to ≤18 years), according to the International Conference of Harmonization (ICH) classification, in the overall study cohort and in each country [19].
3 Results
3.1 Study Population Descriptive
A total of 1278 paediatric patients were identified from five countries. 705 (55.2 %) of the 1278 children were male (Table 1). There was a significant difference in length of hospital stay between countries (p < 0.001), except between Germany and the UK and between HK and Malaysia, where no significant difference was found. Overall, 1140 (89.2 %) children were prescribed at least one medication. The majority (54.1 %; n = 617/1140) were aged ≤2 years, 32.7 % (n = 373/1140) were aged >2 to ≤11 years, and 13.2 % (n = 150/1140) were aged >11 to ≤18 years (Table 1).
The most commonly reported diseases overall and in each country were those of the respiratory system (417/1140; 36.6 %) (Table 1).
3.2 Prescription Prevalence
Overall, 1140 (89.2 %) patients were prescribed a total of 5367 drugs. The median number of drugs prescribed per patient was three [interquartile range (IQR) 2–5 drugs]. The majority of patients (n = 766/1140; 67.2 %) received 1–4 drugs, most of whom were aged ≤2 years (n = 445/766; 58.1 %); while 287 (25.2 %) patients received 5–10 drugs, and 87 (7.6 %) were prescribed more than ten drugs (Table 1). The average number of medicines prescribed per patient was greatest for older children (aged between 11 and 18 years) in all countries except HK where children aged between 2 and 11 years were prescribed the greatest number of medicines per patient (Fig. 1).
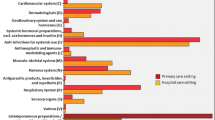
3.2.1 Drug Use by Anatomical Class (Level 1)
Overall, systemic anti-infectives (J) were the most frequently prescribed group (n = 1453; 27.1 %), followed by the nervous system group (N) (n = 1272; 23.7 %). This pattern was also shown in each country. However, whereas respiratory system (R) drugs were the third most commonly prescribed group in HK and Malaysia, in the other three countries the alimentary tract and metabolism drugs group (A) was the third most frequently prescribed group (Table 2).
3.2.2 Drug Use by Therapeutic Class (Level 2)
In the total cohort four therapeutic groups accounted for 55.9 % (n = 2999) of all prescriptions; the highest number was systemic antibacterials (n = 1355; 25.2 %), followed by analgesic drugs (n = 903; 16.8 %), drugs for obstructive airway diseases (n = 472; 8.8 %) and anti-inflammatory and antirheumatic products (n = 269; 5.0 %). Similar patterns were seen in each country for the systemic antibacterials and analgesics. Drugs for obstructive airway diseases were significantly more commonly prescribed in Malaysia compared to the other countries (p < 0.001).
3.2.3 Drug Use by Chemical Substance (Level 5)
Overall, paracetamol was the most frequently prescribed drug (n = 640; 11.9 %), followed by ibuprofen (n = 248; 4.6 %) and salbutamol (n = 226; 4.2 %) (Table 3). A similar pattern was seen in each country for paracetamol prescriptions, except in Germany where ibuprofen (n = 120; 8.9 %) was the most frequently used drug. The second most frequently prescribed drug varied between countries: in the UK it was ibuprofen (n = 108; 5.4 %), in Malaysia cefuroxime (n = 152; 16.8 %), in HK salbutamol (n = 17; 4.8 %), in Australia gentamicin (n = 36; 4.8 %) and in Germany it was metamizole (n = 115; 8.6 %), which was only prescribed in Germany.
Morphine was only prescribed in the UK (53/2010; 2.6 %) and Australia (12/753; 1.6 %); 92.8 % (n = 39/42) of total fluticasone prescribing occurred in Malaysia, where 4.3 % (n = 39/904) of prescriptions were for this medication.
3.2.4 Routes of Administration
Overall the oral route had the highest percentage of prescriptions (n = 2816/5367; 52.5 %), followed by the parenteral route (n = 1744/5367; 32.5 %) and inhalation (n = 468/5367; 8.7 %). The pattern was similar in each country cohort (Table 4). Topical (n = 149/5367; 2.8 %) and rectal (n = 135/5367; 2.5 %) routes were used less frequently.
Oral and parenteral routes were the most frequently used routes of administration for the five most frequently prescribed therapeutic groups. The majority of systemic antibacterials (n = 979/1355; 72.2 %) were given parenterally, while the majority of analgesics/NSAIDs (n = 922/1172; 78.7 %) were given orally.
Salbutamol was given via both inhalation and parental routes only in the UK (n = 58 and n = 7 prescriptions, respectively).
Of the total rectal prescriptions, 73.3 % (n = 99/135) occurred in Germany, where 7.4 % (n = 99/1343) of prescriptions were for rectal drugs. Of these, 56.6 % (n = 56/99) were paracetamol suppositories and 17.2 % (n = 17/99) were for sorbitol (laxative) administration.
With regard to topical prescriptions, 67.8 % (n = 101/149) occurred in the UK, where 5 % (n = 101/2010) of prescriptions were for a topical medication. Of these, 16.8 % (n = 17/101) were for lidocaine (in combination) as an anaesthetic.
3.3 Drug Exposure
The exposure of patients to the most frequently prescribed therapeutic groups in each country and overall, stratified by age groups, is shown in Table 5.
There was a significant difference between countries regarding the number of patients exposed to each of the most commonly prescribed therapeutic groups (p < 0.05). Use of ‘blood substitutes and perfusion solutions’ was not reported in Malaysia; a significant difference in the number of patients exposed to this group was found between the other four countries (p < 0.05).
3.3.1 Systemic Antibacterials
Overall, 65.1 % (n = 742) of the patients received at least one systemic antibacterial (median 1, IQR 1–2, range 1–10). Of the 742 patients, 51.3 % (n = 381) were exposed to one systemic antibacterial, 29.6 % (n = 220) to two different types of antibacterials, and 19 % (n = 141) were prescribed three or more different antibacterials. A similar pattern was shown in most individual countries with the exception of Australia, where the highest percentage was for patients who received three or more different antibacterials (37.6 %; n = 32/85). In Malaysia the number of patients (n = 244/288; 84.7 %) exposed to systemic antibacterials was higher than in the other countries (p < 0.001). Overall, 99.5 % (n = 1348/1355) of the prescriptions for this group were given parenterally (n = 979/1348; 72.6 %) or orally (n = 369/1348; 27.4 %). This pattern of a high percentage of the prescriptions for systemic antibacterials (J01) given parenterally was also shown in the individual countries [Australia 145/189 (76.7 %), Germany 213/291 (73.2 %), UK 252/397 (63.5 %), HK 41/61 (67.2 %) and Malaysia 328/417 (78.7 %)].
3.3.2 Analgesics and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
At least one analgesic was received by 60.9 % (n = 694) of patients (median 1, IQR 1, range 1–5) and 22.1 % (n = 252) received at least one ‘anti-inflammatory and anti-rheumatic product’ (median 1, IQR 1, range 1–2) (Table 5).
When analgesic and NSAID prescriptions were combined into one group (Analgesics/NSAIDs), the exposure rates varied between 84.2 % in the UK and 35.3 % in HK (p < 0.001). In the overall cohort there was no significant difference within age groups in the number of patients exposed to this combined group (p = 0.899), nor was there in each country.
3.3.3 Drugs for Obstructive Airway Diseases
Overall, 23.6 % (n = 269) of patients received at least one of the ‘drugs for obstructive airway diseases’ (medium 1, IQR 1–2, range 1–6). Overall, there was a significant difference in the exposure rates among age groups (p < 0.05), but this was not the case among age groups within each country.
Also there was a significant difference in the percentage of patients exposed to this therapeutic group between the countries (p < 0.01): highest in Malaysia (n = 97/288; 33.7 %) and lowest in Germany (n = 37/293; 12.6 %) (Table 5).
4 Discussion
The study showed that on average 89.2 % of the hospitalised paediatric patients in the study cohort were prescribed one or more drugs (new and/or continued from the community) during their admission, although the number of children exposed to drug therapy varied significantly between the countries. In Germany 77.9 % of patients received pharmacological treatment whereas in the UK and Malaysia it was higher (96.8 and 96.0 %, respectively). This may be due in part to the fact that in Germany particularly young children with ‘commotio cerebri’ are commonly hospitalised for monitoring purposes which may not be the case in the other countries.
Of significance is that the majority of poly-pharmacy occurs in older children. Whilst there may be many reasons for this, we could hypothesis that this is either due to co-morbidities increasing through childhood, increased severity of disease requiring multiple medications or poor management in terms of medicines being added but not being stopped. In line with these thoughts, the lowest tier (prescribed 1–4 drugs) was represented by a majority of children ≤2 years old. This might be because most young children have a single clinical condition at this stage of life and thus have a low medication need. However, it might also suggest that prescribing is carried out more conservatively in this age group, due to a lack of experience, lack of evidence base or lack of formulary drugs that the clinician is able to prescribe.
The average number of different drugs prescribed per patient was very high in some countries (>10 drugs per patient in the UK). This in itself is an interesting fact, with a perception that children use relatively few medicines. The variation, however, is of more interest and indicates that countries either have different reliance on medicines as a medical intervention or that paediatric general medical wards are used for sicker patients (more need for medicines) in some countries than others.
4.1 Drug Prescriptions
Overall and in each country individually, the majority of the paediatric patients (67 %) received 1–4 drugs.
4.1.1 Route of Administration
In our study we found some differences in the route of drug administration; Germany had the highest use of the rectal route. There are cultural and sexual restrictions to consider regarding this route as there is reluctance in some societies to administer drugs via the rectal route [20]. This might be related to child protection concerns, so rectal administration is only used in exceptional situations when the oral route is difficult to use, such as in a vomiting child [20, 21]. A recent review which investigated the reasons for the unpopularity of the rectal route for drug administration to children concluded that more effort needs to be focused on educating parents and care providers on the benefits of this route for drug administration [22].
Also, we found that administration of therapy by inhalation was particularly common in Malaysia. This is probably linked to the high use of drugs for obstructive airway diseases which is higher in Malaysia compared to the other countries.
The topical route was commonly used in the UK mainly for the administration of anaesthetics. It appears that particular caution is paid in the UK to avoid pain and distress when invasive procedures such as inserting a cannula are performed.
4.2 Drug Exposure: Main Therapeutic Classes
We need to consider that differences in the climate between participating countries may also have affected the type of reported diseases, and consequently prescribing pattern. Malaysia has a tropical climate and influenza symptoms peak during the rainy season, and the data collection period was during a considerably wet season. HK is a temperate southern hemisphere climate, and the data were collected between the summer–winter seasons. The UK and Germany are northern hemisphere countries and data were collected between the autumn–spring seasons, while Australia is a southern hemisphere country and at the time of the study it was spring–summer.
4.2.1 Antibacterials
In a German study, it was found that antibacterials were the most common drug class used to treat children in hospital [15]. Our study had similar findings. Antibiotics with broad-spectrum activity were most frequently prescribed. The increased use of broad-spectrum antibacterials, compared to those with a narrow spectrum of activity, in primary and secondary care has been recognised in previous studies [23, 24]. Fossum et al.’s study [24] investigated the antibiotic prescription patterns in primary healthcare in Norway, and found that there was an overuse of macrolides and penicillins with an extended spectrum. However, patients admitted to hospital are often severely ill and need immediate antibiotic therapy. Thus empirical antibiotic therapy to treat a broad spectrum of bacteria is usually commenced. Once the antibiogram is available the treatment is adjusted to eliminate the specific bacteria identified for a specific patient.
In our study, 48.7 % of patients treated with systemic antibacterials received two or more different types of antibacterials, which might have led to the high numbers of antibacterial prescriptions in all countries. The fact that different broad-spectrum antibiotics were used in each country may be due to differences in disease patterns and/or variation in guidelines. The high proportion of patients prescribed systemic antibacterial drugs in Malaysia may be because Malaysia is a tropical country and infectious diseases including respiratory tract infections occur with a reported prevalence of 61.3 % [16]. Our study found that the proportion of total prescriptions for antibacterials was much higher in Malaysia than in the other countries; also the proportion of patients with respiratory system disease was high, which supports this proposal.
The variation in the drugs used among the participating countries could be determined by cultural influences, national guidelines, local or regional policy, local resistance patterns, condition for which the child was admitted, knowledge of appropriate antibiotic prescribing and availability of drugs on the market.
4.2.2 Analgesics and NSAIDs
Paracetamol was widely used in all countries, but the use of other analgesics varied, e.g. metamizole was only used in Germany, whilst in the UK and Australia morphine was the most frequently prescribed analgesic after paracetamol. This is in line with previous studies from Germany, Australia, the UK, USA and Italy [10, 15, 25–29]. Though metamizole is a very effective analgesic and antipyretic and can be used in both adults and children, it is not available in some countries, e.g. the UK, because of its association with rare but life-threatening agranulocytosis and aplastic anaemia [30–32].
Our study shows there are differences between countries in the number of patients exposed to analgesics/NSAIDs, being highest in the UK and lowest in HK. Use of both an analgesic and an anti-inflammatory drug alternatively, e.g. paracetamol and ibuprofen, was seen commonly in some countries such as Germany, but was less frequent in other countries. It was not possible to ascertain the reason(s) for the differences in the prescription patterns of these drugs among the participating countries as we did not investigate the formularies of the participating hospitals nor their guidelines (if any), but a possible explanation could be due to differences in therapeutic practices, availability of drugs or beliefs in each country. Differences in clinical practice and prescribing behaviour between countries and even among healthcare settings within countries have been shown in previous studies [12, 26, 33, 34].
The study provides an interesting finding regarding differences in pain therapy among the participating countries: in the UK up to 90 % of patients received analgesic therapy whereas only 50 % did in some other countries and none of the adolescents in Malaysia received this treatment. However, it has been shown there is often insufficient pain treatment in paediatric patients [35] and our data indicate this may still be the case at some hospitals.
4.2.3 Drugs for Obstructive Airway Diseases
Our study results show a significant difference between countries in the percentage of patients exposed to this drug group, being highest in Malaysia and lowest in Germany. This could be explained by the high percentage of patients with respiratory system diseases and the tropical climate of Malaysia [36]. The use of two routes of administration for some drugs was found in some countries, for example the use of salbutamol via both inhalation and parenteral routes in the UK, but only by inhalation in the other four countries. The use of one drug via two different routes of administration has been shown to increase the risk of adverse drug reactions [16]. One of the reasons for such differences in practice might be related to the severity of the disease being treated or to variations in hospital guidelines.
4.3 Strengths and Limitations
This multicentre study provides useful information on drug utilisation in hospitalised paediatric patients admitted to paediatric general medical wards, from five hospitals in five countries. Data were collected prospectively, using the same protocol. Standardised data collection methods and terminologies enabled comparisons to be made between the countries.
However, this study has several limitations. It was conducted on paediatric general medical wards, so there may be differences between countries in the type of clinical conditions in patients admitted to these wards. If a hospital has specialist wards, e.g. a neurology or a metabolic ward, as in the UK, then that hospital would not admit these patients to a paediatric general medical ward, whilst those without specialist wards would. Another limitation is the seriousness and/or severity of the diagnosis reported on admission was not recorded, therefore some countries may have admitted more serious cases, which could help to explain the differences in drug use patterns.
The sample size from two hospitals, Australia and Hong Kong, was small. This was due to resource limitations in Australia which resulted in only 1 month of data collection. The spread of pandemic flu (influenza A H1N1) during the second half of 2009 in Hong Kong led to restrictions in ward visits for research, thus a smaller number of patients were recruited.
Also, although we limited the period to complete data collection from all countries to be within 1 year, we did not limit to it one season. Thus seasonal variation between countries might have an impact on the nature and/or number of admissions and thus on the prescription patterns.
Lack of data on the impact of cultural practices and lack of knowledge on formularies/guidelines are other limitations.
The findings in this paper were derived from the secondary use of data collected in a study of adverse drug reactions [16] in 2008–2009. However, the findings provide useful data on drug use in paediatric general medical wards in the countries that participated.
4.4 Implications for Practice and Research
This study may also help to prioritise drug utilisation research in children as it raises the need for more research on the use of different routes for drug administration, the use of opioids and combined analgesics. Also, the high use of antibacterials and differences in the use of specific antibiotics raises concerns for antibacterial resistance; further investigation is needed to determine the reasons for this, i.e. disease patterns, severity of disease or treatment strategies. Such information may help to improve the safety of drugs used in paediatric patients.
5 Conclusion
This multicentre study provides useful information on drug utilisation in children admitted to the paediatric general medical ward of five hospitals in five countries, culturally and ethnically diverse. It shows that the most frequently used therapeutic drugs were similar, but the proportion of patients treated differed between the countries. Within a therapeutic group the specific drug used varied from country to country. The prescription patterns differed among the countries, which might be related to differences in clinical practice regarding treatment strategies of paediatric drug therapy in these countries or differences in diagnoses on admission.
References
European Commission. Better medicines for children: proposed regulatory actions on paediatric medicinal products. 2002. http://ec.europa.eu/health/files/pharmacos/docs/doc2002/feb/cd_pediatrics_en.pdf. Accessed 20 May 2015.
World Health Organisation (WHO). Introduction to drug utilization research. 2003. http://www.whocc.no/filearchive/publications/drug_utilization_research.pdf. Accessed 20 May 2015.
Porta A, Hsia Y, Doerholt K, et al. Comparing neonatal and paediatric antibiotic prescribing between hospitals: a new algorithm to help international benchmarking. J Antimicrob Chemother. 2012;67:1278–86.
Neubert A, Hsia Y, de Jong-van den Berg LT, et al. Comparison of anti-diabetic drug prescribing in children and adolescents in seven European countries. Br J Clin Pharmacol. 2011;72:969–77.
Rani F, Murray M, Byrne P, et al. Epidemiologic features of antipsychotic prescribing to children and adolescents in primary care in the United Kingdom. Pediatrics. 2008;121:1002–9.
Ackers R, Murray ML, Besag FMC, et al. Prioritising Children’s medicines for research: A pharmacoepidemiological study on antiepileptic drugs. Br J Clin Pharmacol. 2007;63:689–97.
Murray ML, de Vries CS, Wong ICK. A drug utilisation study of antidepressants in children and adolescents using the General Practice Research Database. Arch Dis Child. 2004;89:1098–102.
Neubert A, Sturkenboom MC, Murray ML, et al. Databases for pediatric medicine research in European-assessment and critical appraisal. Pharmacoepidemiol Drug Saf. 2008;17:1155–67.
Star K, Caster O, Bate A, et al. Dose variations associated with formulations of NSAID prescriptions for children: a descriptive analysis of electronic health records in the UK. Drug Saf. 2011;34:307–17.
Sturkenboom MC, Verhamme KM, Nicolosi A, et al. Drug use in children: cohort study in three European countries. BMJ. 2008;337:a2245.
Abi Khaled L, Ahmad F, Brogan T, et al. Prescription medicine use by one million Canadian children. Paediatr Child Health. 2003;8(Suppl A):6A–56A.
Warrier I, Du W, Natarajan G, et al. Patterns of drug utilization in a neonatal intensive care unit. J Clin Pharmacol. 2006;46:449–55.
Pandolfini C, Kaguelidou F, Sequi M, et al. Wide intra- and inter-country variability in drug use and dosage in very-low-birth-weight newborns with severe infections. Eur J Clin Pharmacol. 2013;69:1031–6.
Cazzato T, Pandolfini C, Campi R, et al. Drug prescribing in out-patient children in Southern Italy. Eur J Clin Pharmacol. 2001;57:611–6.
Neubert A, Lukas K, Leis T, et al. Drug utilisation on a preterm and neonatal intensive care unit in Germany: a prospective, cohort-based analysis. Eur J Clin Pharmacol. 2010;66:87–95.
Rashed AN, Wong IC, Cranswick N, et al. Adverse drug reactions in children – international surveillance and evaluation (ADVISE): a multicentre cohort study. Drug Saf. 2012;35:481–94.
WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index [online]. 2013. Available: http://www.whocc.no/atc_ddd_index/. Accessed 20 May 2015.
International Classification of Diseases Version 10 (ICD 10). 2013. http://www.who.int/classifications/icd/en/. Accessed 20 May 2015.
International Conference on Harmonisation (ICH) Guideline. E11: clinical investigation of medicinal products in the paediatric population. London: European Medicines Agency for the Evaluation of Medicinal Products (EMEA). 2001. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002926.pdf . Accessed 20 Jul 2015.
Rogers J, Irwin K, Fenton J. Digital rectal examination. Guidance for nurses working with children and young people. Royal College of Nursing. 2005. http://www.rcn.org.uk/__data/assets/pdf_file/0009/78588/002062.pdf. Accessed 20 May 2015.
Dyer L, Furze C, Maddox C, Sales R. Administration of medicines. Practice in children’s nursing. 2005. http://www.us.elsevierhealth.com/media/us/samplechapters/9780443100222/9780443100222.pdf. Accessed 20 May 2015.
Jannin V, Lemagnen G, Gueroult P, et al. Rectal route in the 21st century to treat children. Adv Drug Deliv Rev. 2014;73:34–49.
van Houten MA, Luinge K, Laseur M, et al. Antibiotic utilisation for hospitalised paediatric pateitns. Int J Antimicob Agents. 1998;10:161–4.
Fossum GH, Lindbaek M, Gjelstad S, et al. Are children carrying the burden of broad-spectrum antibiotics in general practice? Prescription pattern for paediatric outpatients with respiratory tract infections in Norway. BMJ Open. 2013;3:e002285.
Rashed AN, Wong IC, Cranswick N, et al. Risk factors associated with adverse drug reactions in hospitalised children: international multicentre study. Eur J Clin Pharmacol. 2012;68:801–10.
Neubert A, Verhamme K, Murray ML, et al. The prescribing of analgesics and non-steroidal anti-inflammatory drugs in paediatric primary care in the UK, Italy and the Netherlands. Pharmacol Res. 2010;62:243–8.
O’Donnell CP, Stone RJ, Morely CJ. Unlicensed and off-label drug use in an Australian neonatal intensive care unit. Pediatrics. 2002;110:e52.
Lasky T, Ernst FR, Greenspan J, et al. Estimating pediatric inpatient medication use in the United States. Pharmacoepidemiol Drug Saf. 2011;20:76–82.
Lasky T, Greenspan J, Ernst FR, et al. Morphine use in hospitalized children in the United States: a descriptive analysis of data from pediatric hospitalizations in 2008. Clin Ther. 2012;34:720–7.
Hedenmalm K, Spigset O. Agranulocytosis and other blood dyscrasias associated with dipyrone (metamizole). Eur J Clin Pharmacol. 2002;58:265–74.
Gozzoli V, Treqqiari MM, Kleger GR, et al. Randomized trial of the effect of antipyresis by metamizol, propacetamol or external cooling on metabolism, hemodynamics and inflammatory response. Intensive Care Med. 2004;30:401–7.
Oehme AK, Rashed AN, Hefele B, et al. Adverse drug reactions in hospitalised children in Germany are decreasing: results of a nine year cohort-based comparison. PLoS One. 2012;7:e44349.
Jankovió SM, Đukić-Dejanović SM. Drug utilization trends in clinical hospital center “KRAGUJEVAC” from 1997 to 1999. Indian J Pharmcol. 2001;33:29–36.
Clavenna A, Sequi M, Bortolotti A, et al. Determinants of the drug utilization profile in the paediatric population in Italy’s Lombardy Region. Br J Clin Pharmacol. 2009;67:565–71.
Solomon P. Congruence between health professionals’ and patients’ pain ratings: a review of the literature. Scand J Caring Sci. 2001;15:174–80.
Khor CS, Sam IC, Hooi PS, Quek KF, Chan YF. Epidemiology and seasonality of respiratory viral infections in hospitalized children in Kuala Lumpur, Malaysia: a retrospective study of 27 years. BMC Pediatr. 2012;12:32.
Acknowledgments
Asia Rashed was funded by the Yamani Cultural and Charitable Foundation, London, UK.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
The study protocol was reviewed and approved by the appropriate national research ethics committee in each participating country and has been performed in accordance with the ethical standards of the declaration of Helsinki. As this was an observational study, involving intensive chart review, no direct contact with patients or informed consent was required. Only anonymised data was recorded which cannot be traced to individual patients.
Conflict of interest
ANR, IW, LW, ST and AN have declared that they have no competing interests.
Funding
None.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rashed, A.N., Wong, I.C.K., Wilton, L. et al. Drug Utilisation Patterns in Children Admitted to a Paediatric General Medical Ward in Five Countries. Drugs - Real World Outcomes 2, 397–410 (2015). https://doi.org/10.1007/s40801-015-0049-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-015-0049-y