Abstract
Objective
To study the effect of material deprivation on prescribing trends in primary care, using a locally derived deprivation score.
Methods
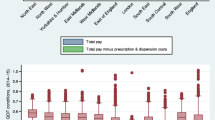
A retrospective analysis of prescribing trends linked to material deprivation by district electoral division (DED) in the Eastern Region of the General Medical Services in Ireland (population of 334,031) was performed. Standardised prescribing ratios were determined for a number of drug classes, including those that could be used to identify particular diseases for 181,647 patients who were assigned a locally derived material deprivation score.
Results
Prescribing rates for a number of medications including anti-asthma, nitrate and benzodiazepine medications increased, whilst the prescribing of other medications such as anti-parkinsonian and antidepressive agents decreased with increasing deprivation.
Conclusions
Our results suggest that, even within a population considered to be economically deprived, different levels of deprivation may significantly influence general practitioner prescribing patterns. Within the group of centrally active medications, the prescription of symptomatic medications increased with increasing material deprivation, whilst the prescription of disease-specific medications decreased with increasing material deprivation.




Similar content being viewed by others
References
Macintyre K, Stewart S, Chalmers J, Pell J, Finlayson A, Boyd J, Redpath A, McMurray J, Campbell S (2001) Relation between socioeconomic deprivation and death from a first myocardial infarction in Scotland: population-based analysis. BMJ 322:1152–1153
Pollock A, Vickers N (1998) Deprivation and emergency admissions for cancers of colorectum, lung, and breast in south east England: ecological study. BMJ 317:245–252
Sloggett A, Joshi H (1994) Higher mortality in deprived areas: community or personal disadvantage. BMJ 309:1470–1474
Worral A, Rea J, Ben-shlomo Y (1997) Counting the cost of social disadvantage in primary care: retrospective analysis of patient data. BMJ 314:38–42
Carlisle R, Groom L, Avery AJ, Boot D, Earwicker S (1998) Relation of out of hours activity by general practice and accident and emergency services with deprivation in Nottingham: longitudinal survey. BMJ 316:520–523
Carr-Hill RA, Rice N, Roland M (1996) Socioeconomic determinants of rates of consultation in general practice based on fourth national morbidity survey of general practices. BMJ 312:1008–1012
National Heart Forum (1999) Social inequalities in coronary heart disease: opportunities for action. Stationery Office, London
Townsend P, Phillimore P, Beattie A (1988) Health and deprivation: inequality and the North. Croom Helm, London
Carstairs V, Morris R (1991) Deprivation and health in Scotland. Aberdeen University Press, Aberdeen
Feely J (1992) The influence of pharmacoeconomic factors on prescribing patterns in Ireland. Pharmacoeconomics 2:99–106
General Medical Services (Payments) Board (2001) Annual report for the year ended 31st December 2000. Dublin
Ryan C, Ryan F, Keane E, Hegarty H (2000) Trend analysis and socio-economic differentials in infant mortality in the Southern Health Board, Ireland (1988–1997). Ir Med J 93:204–206
WHO Collaborating Centre for Drug Statistics Methodology (1999) Anatomical therapeutic chemical (ATC) classification index including defined daily doses (DDDs) for plain substances. WHO, Oslo
Cannon P, Connell P, Stockley I, Garner S (1988) Prevalence of angina as assesses by a survey of prescriptions for nitrates. Lancet 1:979–981
Johnson Z, Hayes C, Dack P (1997) The standardised prescribing ratio—a new method for comparing prescribing between GPs, controlling for patient age and sex. Pharmacoepidemiol Drug Saf 6:337–345
Cuzick J (1985) A Wilcoxon-type test for trend. Statistics in Medicine 4:87–90
Morrison C, Woodward M, Leslie W, Tunstall-Pedoe H (1997) Effect of socioeconomic group on incidence of, and survival after myocardial infarction and coronary death: analysis of community event register. BMJ 314:541
Wilson R, Hatcher J, Barton S, Walley T (1999) The association of some practice characteristics with antibiotic prescribing. Pharmacoepidemiol Drug Saf 8:15–21
Davey P, Rutherford D, Graham B (1994) Repeat consultations after antibiotic prescribing for respiratory infection: a study in one general practice. Br J Gen Pract 44:509–513
McGavock H (1988) Some patterns of prescribing by urban general practitioners. BMJ 296:900–902
Bell RA, Camacho F, Goonan K, Duren-Winfield V, Anderson RT, Konen JC, Goff DC Jr (2001) Quality of diabetes care among low-income patients in North Carolina. Am J Prev Med 21:124–131
Weng C, Coppini DV, Sonksen PH (2000) Geographic and social factors are related to increased morbidity and mortality rates in diabetic patients. Diabet Med 17:612–617
Burr ML, Verrall C, Kaur B (1997) Social deprivation and asthma. Respir Med 91:603–608
Mielck A, Reitmeir P, Wjst M (1996) Severity of childhood asthma by socioeconomic status. Int J Epidemiol 25:388–393
Watson JP, Cowen P, Lewis RA (1996) The relationship between asthma admission rates, routes of admission, and socioeconomic deprivation. Eur Respir J 9:2087–2093
Wilson KC, Chen R, Taylor S, McCracken CF, Copeland JR (1999) Socio-economic deprivation and the prevalence and prediction of depression in older community residents. The MRC-ALPHA Study. Br J Psychiatry 175:549–553
Yen IH, Kaplan GA (1999) Poverty area residence and changes in depression and perceived health status: evidence from the Alameda County study. Int J Epidemiol 28:90–94
Morgan CL, Ahmed Z, Kerr MP (2000) Social deprivation and prevalence of epilepsy and associated health usage. J Neurol Neurosurg Psychiatry 69:13–17
Acknowledgements
We would like to acknowledge the GMS(Payments) Board, the Small Area Health Research Unit and the Health Information Unit of the Eastern Regional Health Authority for their help in conducting this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Williams, D., Teljeur, C., Bennett, K. et al. Influence of material deprivation on prescribing patterns within a deprived population. Eur J Clin Pharmacol 59, 559–563 (2003). https://doi.org/10.1007/s00228-003-0650-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-003-0650-y